Retrospective Observational Study of Cervical Epidural Injection: A Comparison between Dexamethasone vs Triamcinolone
Dr. Yogita Bhargude M*, Dr. Manjiri Ranade, Dr. Rutvi Mody,Dr. Prakash Deshmukh and Dr. Kailash Kothari
Pain Clinic of India Private Limited, Mumbai, Maharashtra, India
Submission: April 3, 2023; Published: August 03, 2023
*Corresponding author: Yogita Bhargude M, pain Clinic of India Private Limited, Mumbai, Maharashtra. email: yogitambk1593@gmail.com
How to cite this article: Yogita Bhargude M, Manjiri R, Rutvi M, Prakash D, Kailash K. Retrospective Observational Study of Cervical Epidural Injection: 002 A Comparison between Dexamethasone vs Triamcinolone. Nov Tech Arthritis Bone Res. 2023; 4(1): 555630. DOI 10.19080/NTAB.2023.04.555630
Abstract
Introduction: Cervical epidural steroid injections (CESI) have been frequently used since long time for diagnosis and treatment cervical radiculopathies. cervical epidural corticosteroid injection helps in reducing swelling and inflammation of the compressed nerves, hence improving pain for several days to months or longer which leads to help delaying or avoiding the need for surgery. In this retrospective observational study, we aim to compare clinical efficacy of Dexamethasone vs Triamcinolone in the management of chronic neck, shoulder, and arm pain due to herniated intervertebral disc in the cervical region.
Methodology: A retrospective observational study of 1 year follow up was performed in 100 patients of either sex complaining of chronic neck pain with signs of cervical radiculopathy. Patients were divided into 2 groups of 50 each. Those in Group A received Injection Dexamethasone sodium phosphate 12mg and in Group B received Injection Triamcinolone acetonide 40mg in the cervical epidural space under fluoroscopy guidance. All the patients were monitored before the procedure and post-procedure for 4 h following epidural injection and subsequently followed by at the 10 days, 1 month, 3 months, 6 months, 8 months, 10 months and 1 year on telephonic conversation. The primary outcome was to measure the intensity of pain using Visual Analog score (VAS) score of 0-10.
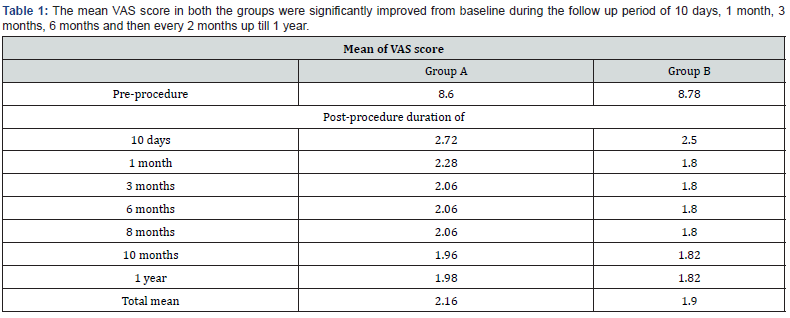
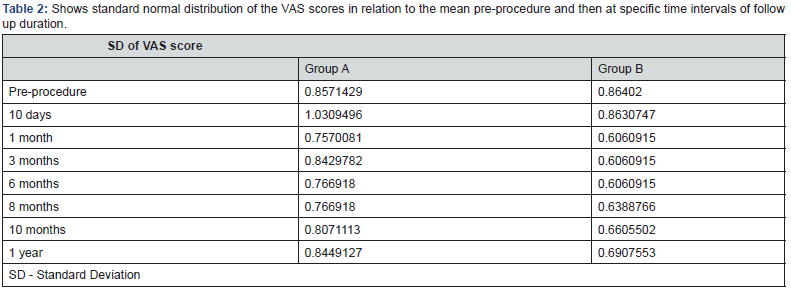
Result: The mean VAS score in both the group A and B pre-procedure was 8.6 and 8.78 respectively and Mean VAS scores were significantly improved to 2.16 and 1.90 respectively post-procedure for 1 year follow up with p value of 0.76. hence from mentioned quantitative data it can be stated that there is no statistically significant difference in the efficacy of both the drugs used in cervical epidural injection.
Conclusion: Based on the results, this retrospective study strengthens the existing evidence that dexamethasone can produce equivalent pain relief to triamcinolone for the treatment of cervical radiculopathy. Though the need for more research studies to prove that Dexamethasone can be used an effective alternative to Triamcinolone continues.
Keywords:Cervical Epidural Steroid Injections; Dexamethasone Sodium Phosphate; Triamcinolone; Dexamethasone; Triamcinolone; Fluoroscopy
Abbreviations:CESI: Cervical Epidural Steroid Injections; VAS: Visual Analog Score; MRI: Magnetic Resonance Imaging; TFESI: Transforaminal Epidural Steroid Injections
Introduction
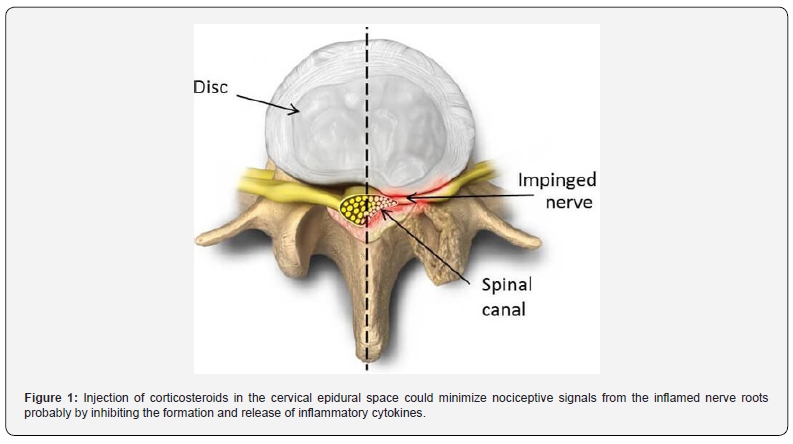
Cervical epidural steroid injections (CESI) have been frequently used since long time for diagnosis and treatment cervical radiculopathies. There are 2 types of CESI: Interlaminar and Transforaminal. CESI is a shot of corticosteroid-an anti-inflammatory medicine into the epidural space around the spinal nerves in the cervical region. The main purpose of CESI is to help manage chronic pain caused by irritation and inflammation of the spinal nerve roots in the cervical spine. Cervical pain can be a consequence of cervical radiculopathy, where patient can have combination of neck pain, shoulder, and arm pain with or without involving hands (Figure 1).
Injection of corticosteroids in the cervical epidural space could minimize nociceptive signals from the inflamed nerve roots probably by inhibiting the formation and release of inflammatory cytokines, which will eventually stabilize neural membranes, and modulate peripheral nociceptive pathway [1-3]. A cervical epidural corticosteroid injection helps in reducing swelling and inflammation of the compressed nerves, hence improving pain for several days to months or longer which leads to help delaying or avoiding the need for surgery. Triamcinolone, Methylprednisolone, and betamethasone are the particulate corticosteroid preparations conventionally used for epidural injections in the management of chronic spinal pain [1,4].
Dexamethasone has been recently emerged as beneficial drug in this setting, corresponding to particulate steroids, although the associated systemic effects have not been fully explained. However, the recent trials demonstrated the substantial effectiveness of dexamethasone, a nonparticulate corticosteroid preparation for epidural injections in patients of low back pain with or without radiculopathy, with heightened safety profile than particulate steroids [5]. In this retrospective observational study, we aim to compare clinical efficacy of Dexamethasone vs Triamcinolone in the management of chronic neck, shoulder, and arm pain due to herniated intervertebral disc in the cervical region.
Methodology
After obtaining due approval from Pain clinic of India, Mumbai and written informed consent from the patients, a retrospective observational study of 1 year follow up was performed in 100 patients of either sex complaining of chronic neck pain with signs of cervical radiculopathy. Patients were divided into 2 groups of 50 each. Those in Group A received Injection Dexamethasone sodium phosphate 12mg and in Group B received Injection Triamcinolone acetonide 40mg in the cervical epidural space under fluoroscopy guidance. The inclusion criteria for CESI were:
• Patients aged 25 to 60 years older with neck or back pain with radiculopathy with Visual Analog Score [VAS] score ≥5) for more than 3 months duration.
• Nerve root compression or spinal canal stenosis identified using magnetic resonance imaging (MRI of cervical spine)
• failure of medical and physical therapy for >2 weeks.
Patients with the rapidly progressing neurological deficit, spine surgery in past, chronic use of steroid or anticoagulant medications, his impairment, prognosticated contrast agents, and history of spinal injection in the past 3 months; cognitive impairment, pregnant and nursing mothers; patients with local or systemic infection; and patients with comorbidities (i.e., uncontrolled hypertension, diabetes mellitus, ischemic heart disease, and haematological diseases, etc.,) were excluded from the study. All the eligible patients were assessed at least 1 week prior to the procedure. Their preprocedural NRS was noted, and they were advised a standard treatment protocol for pain management, i.e., fixed-dose combination of oral tramadol 37.5 mg and paracetamol 325 mg with a minimum interval of 6 hours between two doses.
The CESIs were performed in accordance with International Spine Interventional Society guidelines. On arrival to the procedure room, appropriate monitors were attached, and intravenous line was secured [6]. The patient was placed in the prone position on the C-arm compatible table and supported by a pillow under the chest to give neck extension. Vertebral level for injection is between epidural space of C7-T1 identified under Carm. After sterile preparation of the area and infiltration of skin with local anaesthetic (xylocaine 2%) was given. 18 G Touhy’s epidural needle was used with hanging drop technique as it is an exquisitely sensitive indication of epidural space entry in the cervical region. As the needle is advanced into the desired epidural space, negative pressure within sucks a drop of fluid into the epidural space.
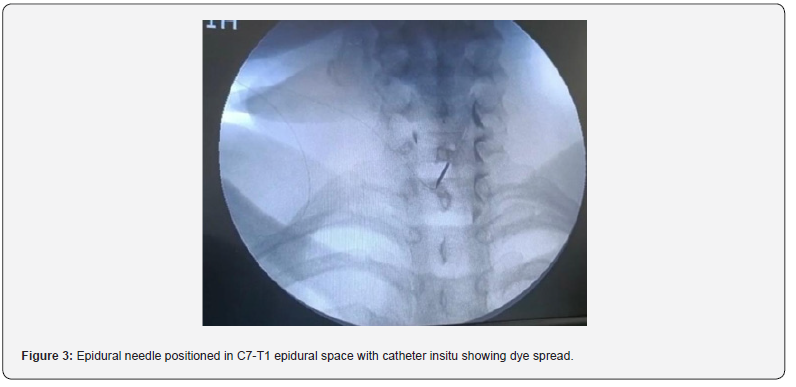
Fluoroscopic images are taken throughout, usually AP and lateral views. Once the needle enters epidural space then, 0.5-1 ml of non-ionic contrast agent was administered under real-time fluoroscopy to confirm the flow of injectate to the target area and absence of vascular or subdural or subarachnoid spread (Figure 2). Once the correct placement of the needle was confirmed under real-time fluoroscopy, patients received the allocated steroid preparations as total 5 ml solution (Figure 3).
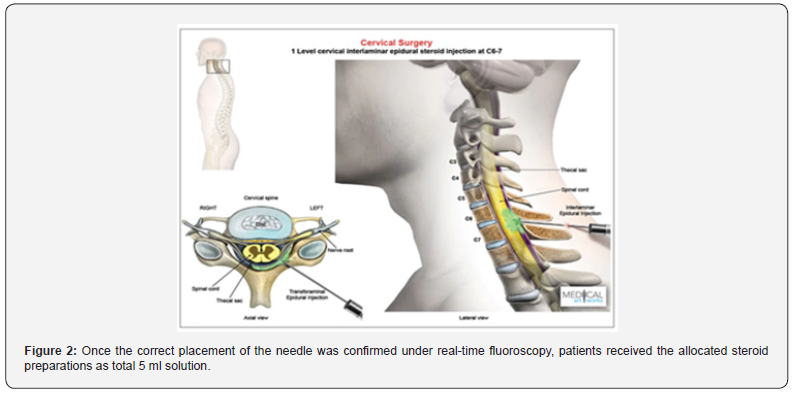
Patients in Group A received 12 mg (3 ml) of dexamethasone sodium phosphate (Dexona, 4 mg per ml, Zydus Cadila Healthcare Ltd. [Alidac], India) diluted in 1 ml of Injection Bupivacaine 0.25% and 1 ml of normal saline. while those in Group B received triamcinolone acetonide 40 mg (Kenacort, 40 mg per ml, Abott Healthcare Pvt. Ltd., India) diluted in 1 ml of Injection Bupivacaine 0.25% and 2 ml of normal saline.
All the patients were monitored for 4 h following epidural injection and subsequently followed by at the 10 days, 1 month, 3 months, 6 months, 8 months, 10 months and 1 year on telephonic conversation. The primary outcome was to measure the intensity of pain using Visual Analog score (VAS) score of 0-10 (0 = no pain, 10 = worst imaginable pain).
Results
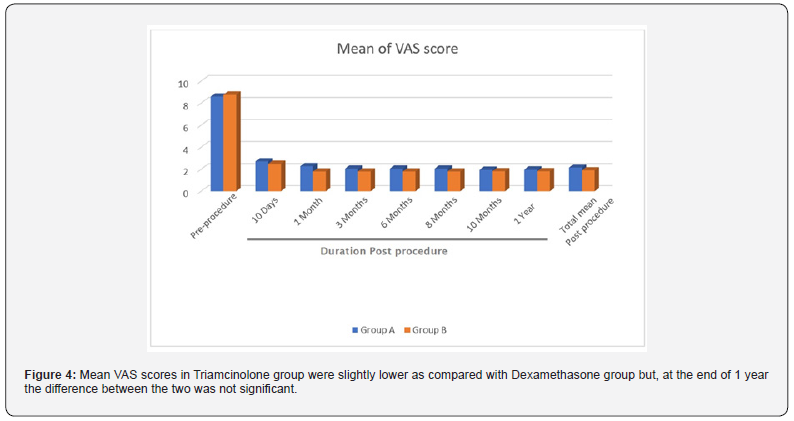
Patients in both the groups were comparable with respect to their baseline mean pain score (VAS). The mean VAS score in both the groups were significantly improved from baseline during the follow up period of 10 days, 1 month, 3 months, 6 months and then every 2 monthly up till 1 year (Table 1), (Figure 4). Mean VAS scores in Triamcinolone group were slightly lower as compared with Dexamethasone group but, at the end of 1 year the difference between the two was not significant. (Table 2) shows standard normal distribution of the VAS scores in relation to the mean preprocedure and then at specific time intervals of follow up duration (Table 2), (Figure 5).
Discussion
This is a retrospective observational study which was conducted on 100 patients of either sex having been diagnosed with cervical radiculopathy. This study showed that Cervical epidural corticosteroids provided significant benefits by reducing pain scores significantly in patients experiencing chronic neck pain secondary to cervical radiculopathy. However, the relief in neck and shoulder pain was greater with group who received Inj. Triamcinolone in cervical epidural space on subsequent initial follow ups but at the end of 1 year of follow up there was not clinically and statistically significant difference found in pain relief between both the groups. P value of the above-mentioned quantitative data was 0.76 which is > 0.05. Hence it can be stated that there is no statistically significant difference in the efficacy of both the drugs used in cervical epidural injection.
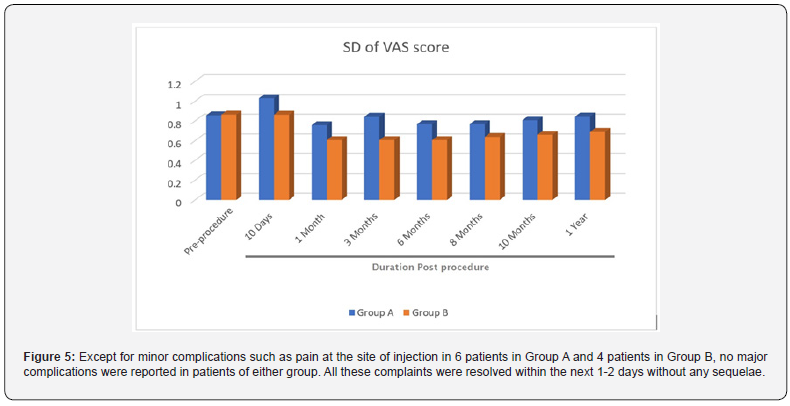
Although this study was not a randomized controlled trial, it does corroborate a growing body of literature that supports cervical TFESI as an effective procedure in the management of radicular pain. The patients in this study experienced no serious adverse effects and had mean reductions in pain score of 1.90 and 2.16 after treatment with triamcinolone and dexamethasone, respectively. Although no serious complications were seen in the population of this study, not all patients who undergo these procedures experience this level of benefit because severe sequelae have been documented in a minority of cases involving cervical TFESI. In the 2004 review, Rathmell et al [7] reported one case of fatal spinal cord infarction caused due to local injection of iotrolan, bupivacaine, and triamcinolone. The same article mentioned 15 other cases that resulted in severe neurologic sequelae. Similarly, Scanlon et al [8].
Conducted a separate review and found 6 cases of spinal cord infarct, 1 brainstem infarct, 6 cases of severe spinal cord injury, and 15 cases of serious neurologic deficits. The study also included a cross-sectional survey of United States members of the American Pain Society that collected 78 more reports of complications including 30 brain/spinal cord infarcts and 13 fatalities. Of these, the specific corticosteroid in use was reported in 28 cases and included 22 cases using methylprednisolone (79%), 3 cases with betamethasone (11%), and 3 cases involving triamcinolone (11%). Dexamethasone was not reported to be associated with severe neurologic sequelae in this report, and a recent search of the literature indicates that this continues to hold true. The idea that many of the complications of ESI may be caused by the particulate nature of injected glucocorticoids has been explored by several groups.
Tiso et al. [9] tested this hypothesis and reported that triamcinolone and methylprednisolone tended to coalesce into aggregates exceeding 100 Km, with the potential to easily occlude arterioles and even arteries. Similarly, Derby et al [10]. reported that triamcinolone acetonide and betamethasone sodium phosphate particles were often larger than red blood cells and exhibited frequent aggregation. The same study showed dexamethasone sodium phosphate particles to be approximately ten times smaller than red blood cells, without a tendency to aggregate even when mixed with an anaesthetic and contrast dye. Despite the apparent safety benefits, widespread use of dexamethasone has been hindered by questions raised regarding its efficacy in comparison with particulate steroids.
In the similar study with an objective to determine whether there is a basis for promoting a theoretically safer nonparticulate corticosteroid preparation done by Dreyfuss P, et al [11] (30 subjects) found that both study groups were showing statistically and clinically significant improvements in pain at 4 weeks where 60% of patients receiving Dexamethasone and 67% of patients receiving Triamcinolone showed 50% improvement in pain score. Although the effectiveness of dexamethasone was slightly less than that of triamcinolone, but the difference was neither statistically nor clinically significant. They also stated that a theoretically safer non-particulate agent seems to be a valid alternative to particulate agents for cervical epidural with less hazards.
In a retrospective cohort study conducted from February 2005 to January 2010 by Shakir A, et al [12] Compared the pain score reduction using triamcinolone vs. dexamethasone in cervical transforaminal epidural steroid injections (TFESI) using 441 patients as their subject. They used Inj. Triamcinolone (40 mg) in 220 subjects and Inj. Dexamethasone (15 mg) in 221 subjects with mean reduction in pain score of 2.33 points and 2.38 points on a scale of 10. Because this study was conducted retrospectively, dosing of the medications at the time of injection could not be made equivalent because these had been originally set with patient benefit as the priority. The result is that the doses of dexamethasone (15 mg) and triamcinolone (40 mg) were not equivalent because dexamethasone is approximately five times more potent than triamcinolone [13].
At their centre, 40 mg of triamcinolone had been the treatment dose for cervical TFESI. Instead of using an equivalent dose of 8 mg of dexamethasone, 15 mg was used to increase potency and increase the likelihood of benefit. They concluded that the mean reduction in pain score in total of 441 patients diagnosed with cervical radiculopathy treated with TFESI was independent of the type of corticosteroid used. They also mentioned that Triamcinolone has a half-life of 12Y36 hrs compared with 36Y72 hrs for dexamethasone [14]. After 1 month of metabolism and excretion they were effectively removed from the body and longterm pain relief was likely driven by the pathology rather than the medication used. Triamcinolone (40 mg) and dexamethasone (15 mg) produced similar benefits as assessed by the patient’s self-reported pain scores. They found no evidence of a significant difference in efficacy between dexamethasone and triamcinolone in the treatment of cervical radiculopathy by TFESI.
One more similar study comparable to our study conducted by Lee et al. [15] (159 subjects) support dexamethasone as a noninferior alternative to triamcinolone, with a theoretical safety benefit. They reported the effectiveness in 69.4% patients and 80.4% patients treated with dexamethasone and triamcinolone, respectively with no statistically significant difference. Though it has been seen that CESI is an effective modality in cases of cervical radiculopathy; physician’s before considering a CESI, must always assess and verify that patient’s pain had persisted at least for six to eight weeks, and the patient has had failed conservative management. One also must pay attention to the fact that patients does not have progressively worsening neurologic deficits [16- 20].
Conclusion
The need for prospective randomized controlled trials regarding use of TFESI and cervical interlaminar epidural injection in the treatment of cervical radiculopathies continues. Based on the results, this retrospective study with sample size of 100 strengthens the existing evidence that dexamethasone can produce equivalent short-term as well as long term pain relief to triamcinolone for the treatment of cervical radiculopathy. Although more research studies should be done to prove that Dexamethasone can be used an effective alternative to Triamcinolone with lesser side effects.
References
- Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, et al. (2007) Epidural steroids in the management of chronic spinal pain: A systematic review. Pain Physician 10(1): 185-212.
- Sitzman BT (2003) Epidural Injections. In: Fenton D, editor. Image-Guided Spine Intervention. Philadelphia: Saunders 100-101.
- Benoist M, Boulu P, Hayem G (2012) Epidural steroid injections in the management of low-back pain with radiculopathy: An update of their efficacy and safety. Eur Spine J 21(2): 204- 213.
- Tauheed N, Usmani H, Siddiqui AH (2014) A comparison of the analgesic efficacy of transforaminal methylprednisolone alone and with low doses of clonidine in lumbo-sacral radiculopathy. Saudi J Anaesth 8: 51- 58.
- El Yahchouchi C, Geske JR, Carter RE, Diehn FE, Wald JT, et al. (2013) The noninferiority of the nonparticulate steroid dexamethasone vs. the particulate steroids betamethasone and triamcinolone in lumbar transforaminal epidural steroid injections. Pain Med 14(11): 1650-1657.
- Bogduk N (2004) Practice Guidelines for Spinal Diagnostic Procedures. San Francisco, CA: International Spine Intervention Society.
- Rathmell JP, Aprill C, Bogduk N (2004) Cervical transforaminal injection of steroids. Anesthesiology 100: 1595- 1600.
- Scanlon GC, Moeller-Bertram T, Romanowsky SM, Mark S Wallace (2007) Cervical transforaminal epidural steroid injections: More dangerous than we think? Spine 32(11): 1249-1256.
- Tiso RL, Cutler T, Catania JA, Joseph A Catania, Karen Whalen (2004) Adverse central nervous system sequelae after selective transforaminal block: The role of corticosteroids. Spine J 4(4): 468- 474.
- Derby R, Lee SH, Date ES, Chang-Hyung Lee (2008) Size and aggregation of corticosteroids used for epidural injections. Pain Med 9(2): 227-234.
- Dreyfuss P, Baker R, Bogduk N (2006) Comparative effectiveness of cervical transforaminal injections with particulate and nonparticulate corticosteroid preparations for cervical radicular pain. Pain Med 7(3): 237-242.
- Shakir A, Ma V, Mehta B (2013) Comparison of pain score reduction using triamcinolone vs. dexamethasone in cervical transforaminal epidural steroid injections. Am J Phys Med Rehabil 92: 768- 775.
- MacMahon PJ, Eustace SJ, Kavanagh EC (2009) Injectable corticosteroid and local anesthetic preparations: A review for radiologists. Radiology 252(3): 647-661.
- Sitzman BT (2003) Pharmacologic properties of common glucocorticoids used in spine injections, in Fenton DS, Czervionke LF (eds): Image-Guided Spine Intervention. Philadelphia, PA, Elsevierp 291.
- Lee JW, Park KW, Chung SK, Jin S Yeom, Ki-Jeong Kim, et al. (2009) Cervical transforaminal epidural steroid injection for the management of cervical radiculopathy: A comparative study of particulate versus non-particulate steroids. Skeletal Radiol 38(11): 1077-1082.
- Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brainb 117 (2):325-335.
- Sampath P, Bendebba M, Davis JD, Ducker T (1999) Outcome in patients with cervical radiculopathy. Prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976) 24(6): 591-597.
- Cicala RS, Thoni K, Angel JJ (1989) Long-term results of cervical epidural steroid injections. Clin J Pain 5(2): 143-145.
- Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ (2000) Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: A retrospective analysis with independent clinical review. Arch Phys Med Rehabil 81(6): 741-746.
- Bush K, Hillier S (1996) Outcome of cervical radiculopathy treated with periarticular/epidural corticosteroid injections: A prospective study with independent clinical review. Eur Spine J 5: 319-325.






























