A Randomized Controlled Trial on Functional Outcome and Effectiveness of Autologous Platelet Rich Plasma Therapy Vs Corticosteroid Injection in Early Knee Osteoarthritis
Ramesh R1, Madhan Jeyaraman2*, Kartavya Chaudhari2, Sabarish K2, Likhith D2 and Preethi Selvaraj3
1Professor, Department of Orthopaedics, JJM Medical College, Karnataka
2Junior Resident, Department of Orthopaedics, JJM Medical College, Karnataka
3 Assistant Professor, Department of Community Medicine, Shri Sathya Sai Medical College and Research Institute, Tamilnadu
Submission: January 29, 2019; Published: February 19, 2019
*Corresponding author: Madhan Jeyaraman, Junior Resident, Department of Orthopaedics, JJM Medical College, Davangere, Karnataka, India
How to cite this article: Ramesh R, Madhan J, Kartavya C, Sabarisk K, Likhith D, et al. A Randomized Controlled Trial on Functional Outcome and Effectiveness of Autologous Platelet Rich Plasma Therapy Vs Corticosteroid Injection in Early Knee Osteoarthritis. Nov Tech Arthritis Bone Res. 2019; 3(4): 555617. DOI: 10.19080/NTAB.2019.03.555617
Abstract
Background: Hyaline cartilage enables the friction free joint movements and has limited intrinsic healing potential because it is avascular and has few specialized cells with a low mitotic activity. Once the cartilage is injured, it gradually degenerates, leading to osteoarthritis. In osteoarthritis, there is an imbalance between the rate of cartilage degeneration and rate of repair. Platelet rich plasma offers a greater advantage by inducing IL-1Ra to maintain joint homeostasis and rejuvenation of degenerated cartilage.
Objectives: To evaluate the efficacy and the functional outcome of autologous platelet rich plasma therapy and corticosteroid injection in patients with early knee osteoarthritis.
Methods: After excluding the patients who failed to satisfy the study protocol, the remaining 337 patients are divided into two groups namely group A (n=173) who receive autologous PRP injection and group B (n=164) who receive intra-articular corticosteroid injections. Both the group participants are followed up pre-procedurally on day 0 and post-procedurally at the end of 1st, 6th and 12th month for pain relief and range of movements of knee. The improvements in pain and range of movements are charted in terms of VAS, WOMAC and KOOS scoring system.
Results: The statistical analysis were done for 147 patients in group A and 131 patients in group B. The patients who received platelet rich plasma therapy showed improved range of movements by the end of 1st month follow up. The group who receive platelet rich plasma therapy show an excellent functional improvement by the end of one year which is statistically significant with p value < 0.001.
Conclusion: The autologous platelet rich plasma therapy is considered superior to for early knee osteoarthritis as it provides growth factors for cartilage rejuvenation which has very limited regenerative potential.
Keywords: Osteoarthritis; Platelet rich plasma; Corticosteroid; WOMAC; KOOS; VAS
Introduction
Hyaline cartilage enables the friction free joint movements and protects the underlying bone from excessive load and trauma by dissipating the forces produced during movement. The cartilage has limited intrinsic healing potential because it is avascular and has few specialized cells with a low mitotic activity. Once the cartilage is injured, it gradually degenerates, leading to osteoarthritis. The increasing number of patients with symptomatic OA will continue to place an increasingly large economic burden on global health care systems [1].
Osteoarthritis (OA) of knee, also called as osteoarthrosis, is a chronic, degenerative joint disease characterized by gradual loss of hyaline cartilage resulting in formation of bony spurs, subchondral sclerosis and cysts at the margins of the joints. Bilateral OA knee (5%) is more common than unilateral OA knee (2%). Biochemically, there is an imbalance between rate of cartilage degeneration with rate of repair. Osteoarthritis (OA) of the knee is the most common degenerative condition which is associated with pain and morbidity [2].
Due to wide range of research in the field of regenerative orthopedics, platelet rich plasma has become a viable, biological and natural healing enhancer and pave a way towards a positive health and improve the quality of life in patients with early osteoarthritis knee. Platelet rich plasma, once activated, degrades the α granules which releases the growth factors. These growth factors induce intracellular signaling which leads to a biological response of cellular proliferation, differentiation and migration. PRP induces the formation of interleukin 1 receptor antagonist which reduces the pain and improves the functional quality of life with early knee osteoarthritis [3].
Objectives
To evaluate the efficacy and the functional outcome of autologous platelet rich injection over intra-articular steroid injection in patients with early knee osteoarthritis.
Materials and Methods
a) Health care setup - Tertiary care hospital.
b) Setting - JJM Medical College, Davangere, Karnataka.
c) Duration of the study - 2016 to 2018.
d) Type of the study - Randomized controlled trial.
e) Sampling technique - Convenient sampling.
f) Level of evidence - Level II.
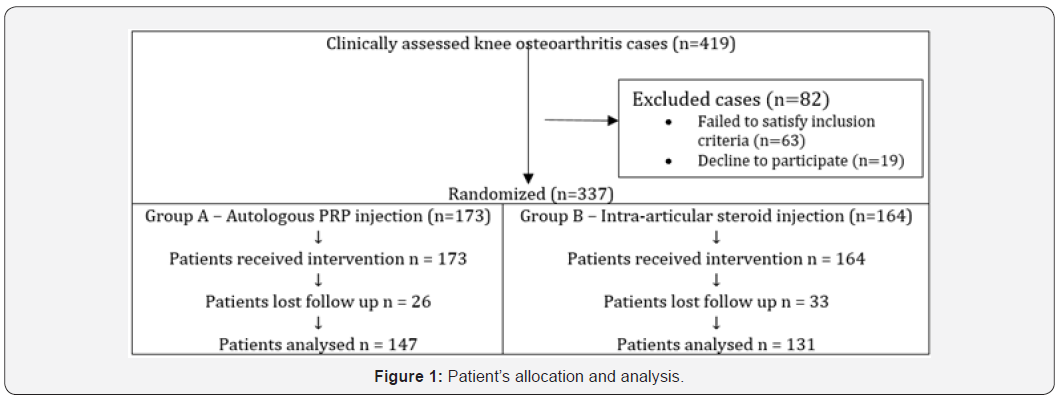
A randomized controlled trial was conducted in 419 cases of osteoarthritis of knee in JJM Medical College, Davangere, from 2016 to 2018. A total of 419 patients of osteoarthritis of knee are clinically identified and 63 patients are excluded from the study who failed to satisfy the inclusion criteria and 19 patients declined to participate the study. The remaining 337 cases were randomized into two groups namely group A (n=173) who receive autologous platelet rich plasma injection and group B (n=164) who receive intra-articular steroid injection (Figure 1) for the patients with early knee osteoarthritis as per our study protocol.
Inclusion Criteria
a) Patients with age between 30 – 80 years of both sex
b) Patients with radiological osteoarthritic knees (Kellgren Lawrence grade 1 & 2 based on x ray findings)
c) Patients with severe pain and under anti-inflammatory treatment without improvement > 3 months
d) Patients who have given consent for treatment as per our protocol
e) Regular visits in the out-patient department
Exclusion Criteria
a) Patients with age less than 20 and more than 80 years of both sex.
b) Patients with advanced osteoarthritis (Kellgren Lawrence grade 3 & 4 based on x ray findings).
c) Patients with h/o prior corticosteroid injection at treatment site within 3 months of duration
d) Patients with rheumatoid arthritis, inflammatory arthritis or polyarticular arthritis and autoimmune diseases.
e) Patients with haemoglobin < 10 gm/dL and platelet count < 105 / μL.
f) Patients with local infection at the site of the procedure, HIV, Hepatitis B or C, septicemia and other systemic metabolic disorders.
g) Patients with bleeding and other coagulation disorders.
h) Patients refusal for PRP treatment as per our protocol.
After getting IEC clearance from the institute and informed written consent from the patients enrolled in our study, they are subjected for thorough clinical examination to rule out the other causes of stiff and painful knee syndrome. The baseline investigations such as complete hemogram, ESR, CRP, renal function tests, random blood glucose, serological testing for HIV 1 & 2 and Hbs Ag and radiographic analysis of affected knee joint in standing position are done.
Preparation of Platelet Rich Plasma
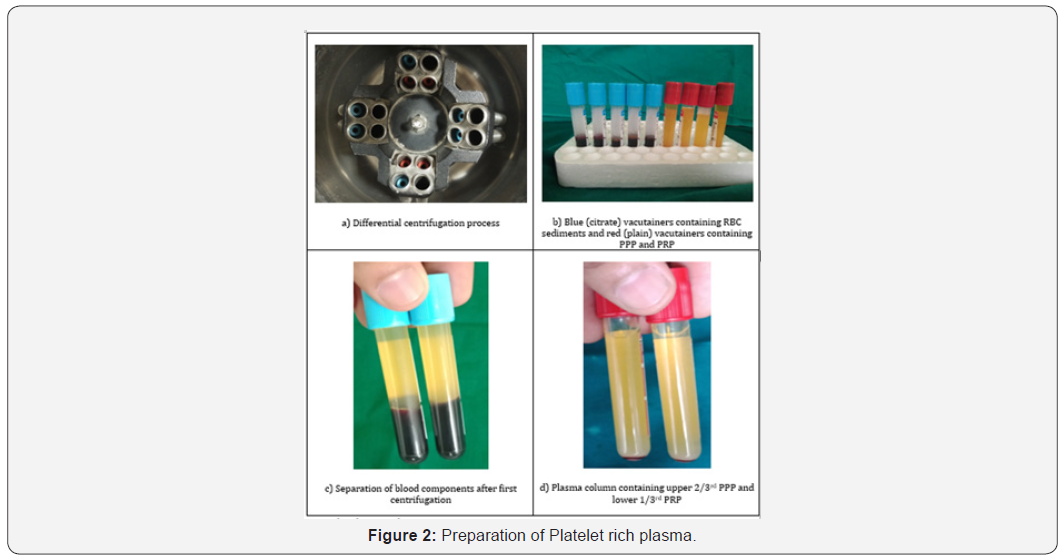
After explaining the procedure to the patients in vernacular language, PRP solution is prepared by a method of double centrifugation process called differential centrifugation technique. 20 cc of venous blood is withdrawn in 3.8% sodium citrate vacutainers and subjected for 1st centrifugation called soft spin at a rate of 3000 rpm for 10 minutes. Then the plasma is separated into the plain vacutainers and subjected for 2nd centrifugation called hard spin at a rate of 5000 rpm for 10 minutes. The resultant solution column in the vacutainer contain upper 2/3rd platelet poor plasma and lower 1/3rd platelet rich plasma. Every 20 cc of venous blood yield 3 – 4 ml of platelet rich plasma solution. Before injecting PRP solution, add 10% of calcium chloride (Ca2+ = 0.22 mEq) to PRP solution in the ratio of 1:10 [2-4] (Figure 2).
Procedural Protocol
In both the groups, the knee joints were approached from anteriorly either through medial or lateral joint line after flexing the knee for about 60°. The patients who got enrolled in group A (n = 173) and group B (n = 164) were treated with two doses of 3 – 4 ml of autologous platelet rich plasma injection and two doses of 40 mg of triamcinolone injection respectively under ultrasound guidance after securing all sterile precautions. The first dose of injections in each group were given on day 0 and the second dose of injections were given after an interval of 4 weeks of first dose. After the procedure, sterile dressing and crepe bandage were applied. After 10 minutes of post procedure in both the groups, a gentle knee mobilization exercises were done for equal distribution of injected solutions into the joint space. The patients were trained for home based active quadriceps and knee strengthening programme.
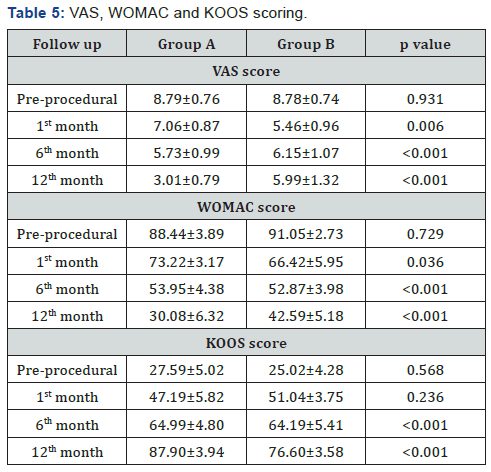
All the patients were advised to bear weight immediately after the appropriate injections and the pain was combated with paracetamol. The patients were followed up for pain and range of movements in accordance with VAS, KOOS and WOMAC scoring system on (pre-procedure) day 0 and (post-procedure) at the end of 1st, 6th and 12th month. All the recorded data were subjected for statistical analysis with Mann–Whitney U test, Chi square test and p value.
Statistical Analysis
The statistical analysis was done with Statistical Package for Social Sciences (SPSS) software (Version 20). To determine whether PRP and corticosteroid influenced outcome variables, repeated measures ANOVA tests were conducted to compare pre-procedure and post-procedure scores at the end of 1st, 6th and 12th month follow-up scores for the VAS, WOMAC and KOOS scores for each group. An alpha level of p < 0.05 was used to determine statistical significance.
Results
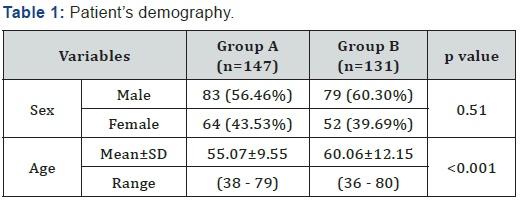
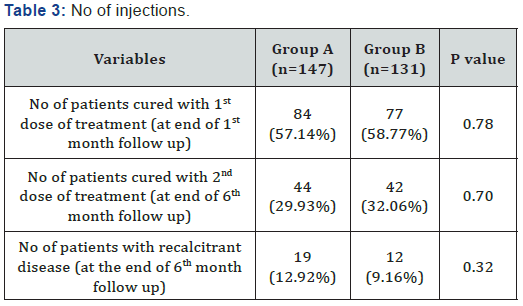
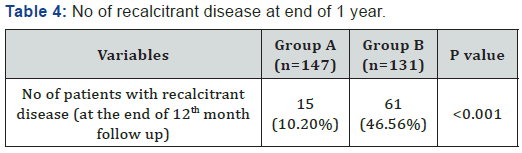
After excluding the drop outs after initiation of appropriate treatment, the patients who were willing to complete the study, were considered for statistical analysis. The statistical analysis with repeated measures ANOVA test and P value were derived from IBM SSPS statistics for Windows, Version 20.0, IBM Corp, Chicago, IL (Tables 1-4).
Group A – Autologous PRP group (n = 173)
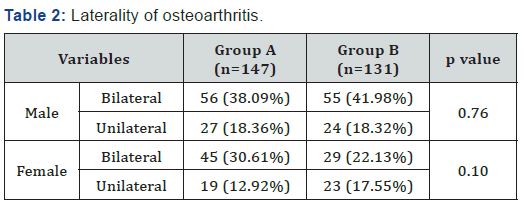
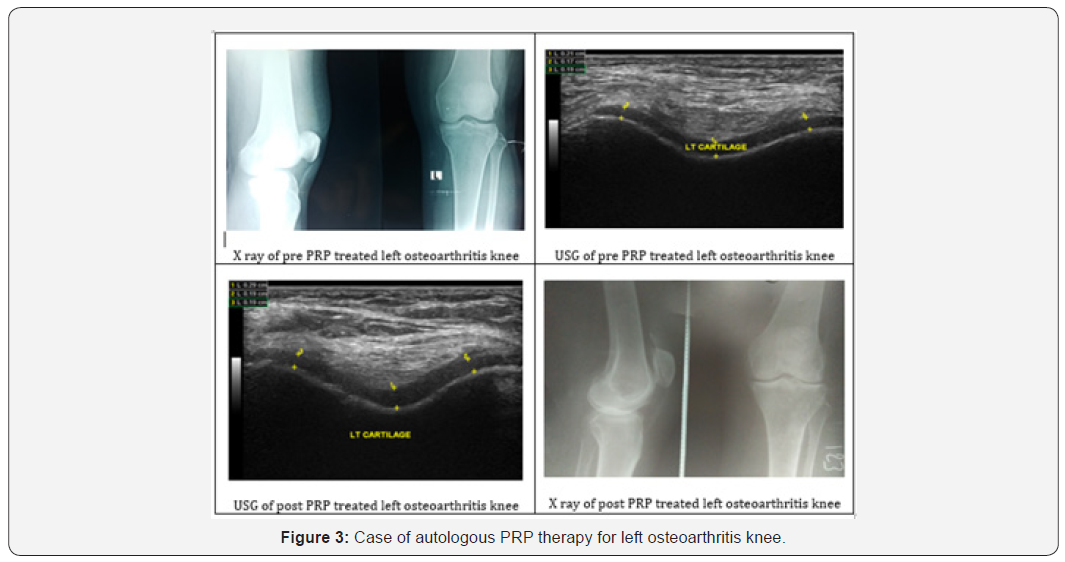
Out of 173 patients, 26 patients lost follow up. Hence the statistical analysis was done for 147 patients. Out of 147 cases, 83 (56.46%) were males and 64 (43.53%) were females. The age ranged from minimum of 38 years to maximum of 79 years. The mean age of patients in group A is 55.07±9.55. Among 83 males, 56 (38.09%) patients had unilateral involvement and 27 (18.36%) patients had bilateral involvement. Among 64 females, 45 (30.61%) patients had bilateral involvement and 19 (12.92%) patients had unilateral involvement (Figure 3).
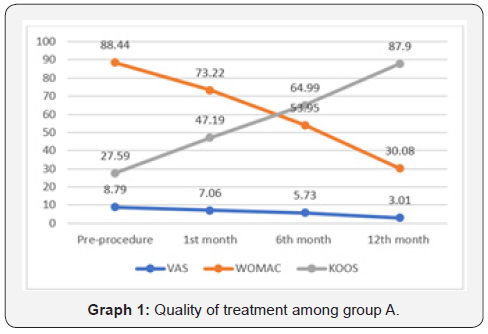
The mean pre-procedural range of knee movements were 70 degree flexion, 0 degree extension, 5 degree internal rotation and 10 degree external rotation. The mean pre-procedural VAS, WOMAC and KOOS scores were 8.79±0.76, 88.44±3.89 and 27.59±5.02 respectively. At the end of 6th month, the mean VAS, WOMAC and KOOS scores improved to 5.73±0.99, 53.95±4.38 and 64.99±4.80 respectively. By the end of 1 year, there were a significant improvement in the mean VAS (3.01±0.79), WOMAC (30.08±6.32) and KOOS (87.90±3.94) scores. The mean range of movements at the end of 1 year were 130 degree flexion, 10 degree extension, 15 degree internal rotation and 35 degree external rotation.
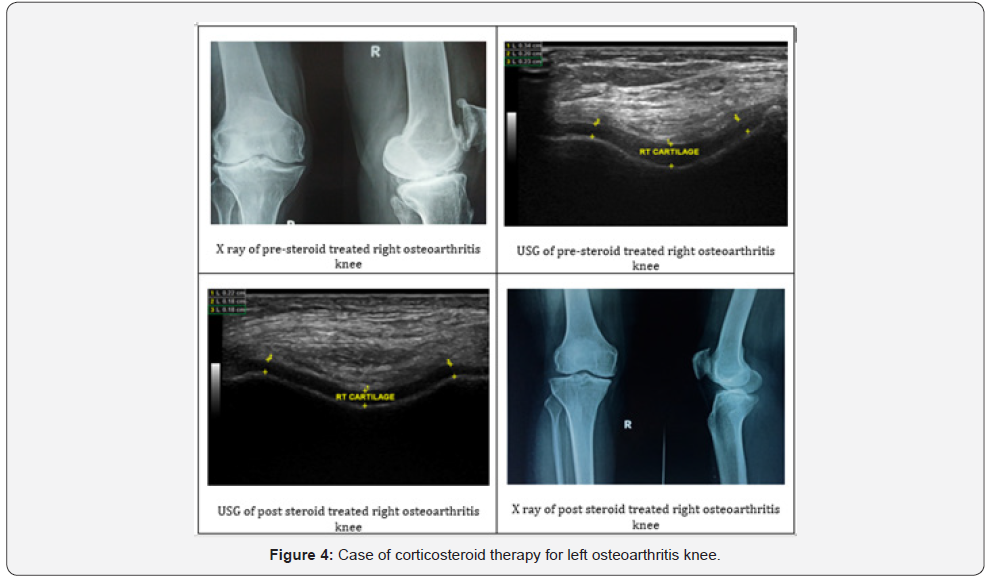
Group B – Corticosteroid group (n = 164)
Out of 164 patients, 33 patients lost follow up. Hence the statistical analysis was done for 131 patients. Out of 131 cases, 79 (60.30%) were males and 52 (39.69%) were females. The age ranged from minimum of 36 years to maximum of 80 years. The mean age of patients in group B is 60.06±12.15. Among 79 males, 55 (41.98%) patients had unilateral involvement and 24 (18.32%) patients had bilateral involvement. Among 52 females, 29 (21.13%) patients had bilateral involvement and 23 (17.55%) patients had unilateral involvement.
The mean pre-procedural range of knee movements were 60 degree flexion, 0 degree extension, 5 degree internal rotation and 10 degree external rotation. The mean pre-procedural VAS, WOMAC and KOOS scores were 8.78±0.74, 91.05±2.73 and 25.02±4.28 respectively. At the end of 6th month, the mean VAS, WOMAC and KOOS scores improved to 6.15±1.07, 52.87±3.98 and 64.19±5.41 respectively. By the end of 1 year, there were a significant improvement in the mean VAS (5.99±1.32), WOMAC (42.59±5.18) and KOOS (76.60±3.58) scores. The mean range of movements at the end of 1 year were 90 degree flexion, 5 degree extension, 10 degree internal rotation and 10 degree external rotation.
Statistical Analysis
At the end of 12th month follow up, the functional scorings of VAS, WOMAC and KOOS scores among both the groups drastically improved from baseline which proved statistically significant (p < 0.001) (Figure 4) (Table 5).
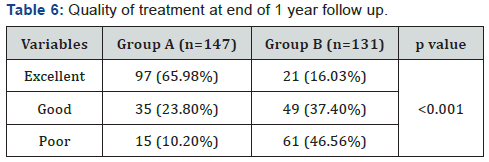
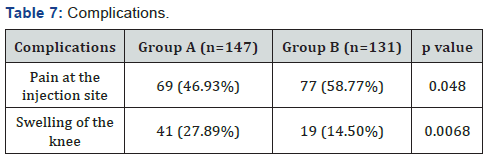
Functional outcome
Out of 147 patients who underwent autologous PRP injection therapy, 97 (65.98%) patients reported excellent results, 35 (23.80%) patients reported good results and 15 (10.20%) patients reported poor results. The complications reported by group A participants were pain in 69 (46.93%) patients and swelling in 41 (27.89%) patients. Out of 131 patients who underwent corticosteroid injection, 21 (16.03%) patients reported excellent results, 49 (37.40%) patients reported good results and 61 (46.56%) patients reported poor results. The complications reported by group B participants were pain in 77 (58.77%) patients and swelling in 19 (14.50%) patients (Graphs 1&2) (Tables 6&7).

Discussion
Osteoarthritis (OA) of knee is also called as osteoarthrosis, chondromalacic arthrosis, degenerative arthritis or arthritis deformans of knee. Osteoarthritis is a chronic, progressive and degenerative joint disease characterized by gradual loss of hyaline cartilage resulting in formation of bony spurs, subchondral sclerosis and cysts at the margins of the joints. Bilateral OA knee (5%) is more common than unilateral OA knee (2%). In the Framingham study, 2% of women per year developed radiographic knee OA, and 1% per year developed symptomatic knee OA, versus 1.4% and 0.7% of men, respectively.
It is hypothesized that osteoarthritis has the higher rate of cartilage degeneration than the rate of cartilage repair. OA destabilize the normal coupling of degradation and synthesis of articular cartilage chondrocytes and extracellular matrix, and subchondral bone. OA has a strong and significant evidence that chondrocytes may transduce mechanical signals into biochemical responses through various intracellular and intercellular signaling pathways, including activation of second messenger pathways such as cyclic AMP (cAMP), inositol trisphosphate, or calcium ion [3]. OA is manifested by morphologic, biochemical, molecular, and biomechanical changes of both cells and matrix which lead to a softening, fibrillation, ulceration, loss of articular cartilage, sclerosis and eburnation of subchondral bone, osteophytes and subchondral cysts.
Biochemical and Biomolecular Changes in Osteoarthritis
Cartilage degeneration at the articular surface occur in the form of fibrillation. Splits are initially parallel to the articular surface; later, they vertically penetrate the damaged cartilage, eventually reaching subchondral bone. The initial lesion in osteoarthritis is the swelling of articular cartilage with enhanced synthesis of matrix with an increased content of aggrecan followed by a phase of increased matrix turnover, with net depletion of principal matrix components. Finally, severe damage to and loss of the collagen network is observed [3].
Proteinases of Osteoarthritis Cartilage
In OA, there is increased expression of matrix metalloproteinases (MMPs) such as MMP-1, MMP-3, MMP-13 & MMP-28 and downregulation of ADAMTS-4 and 5 (a disintegrin and metalloproteinase with thrombospondin motifs). In established OA of the knee, the synthesis of type II collagen and aggrecan are simultaneously increased markedly [4-5].
Regulation of Cartilage Matrix Degradation
Degradation products of matrix molecules may themselves stimulate degradation through chondrocyte and synovial cell receptor-mediated activation, forming a chronic cycle. Fibronectin is produced in increased amounts in OA cartilage whose degradation is the strong stimulator in establishing positive feedback generation of proteolysis. Cellular responses in OA cartilage involve the production of cytokines such as interleukin (IL)-l, which are known to stimulate degradation and also play an essential autocrine and paracrine role in fibronectin fragment-mediated degradation. In OA, there is increased expression of IL-1 on the chondrocyte receptors [6].
The pathologic changes in cartilage matrix structure induces an imbalance resulting from mechanical loading and cytokine and growth factor signaling, which leads to changing gene expression of matrix macromolecules, signaling molecules, and enzymes.(6) Activities of these MMPs are regulated not only at the levels of transcriptional activation, translation, and extracellular proenzyme activation, but also extracellularly at the level of inhibition by tissue inhibitors of metalloproteinases (TIMPs). In OA, there is a deficiency of TIMP activity favoring excessive proteolysis. TIMP-3, which is the only TIMP that can bind to extracellular matrix, is capable of inhibiting aggrecan degradation in hyaline cartilage. Its expression is upregulated in OA cartilage whereas TIMP-1 and -4 are downregulated [6-8].
Changes in Cartilage Matrix Protein Content
The early damage to the more superficial matrix in early OA is accompanied by an increased content of biglycan and decorin and aggrecan in the mid and deep zones of the matrix [9]. This accompanies the marked increase in the synthesis of type II procollagen in these deeper zones of matrix. There is a marked loss of type II collagen, starting in the more superficial cartilage. There is limited expression and synthesis of type III collagen. Increase in type VI collagen and its filamentous structure result in pericellular remodeling which reflects the loss of mechanical properties of the pericellular matrix [10].
Regulation of Cartilage Matrix Assembly in OA
Cytokines such as IL-1 can inhibit matrix synthesis whereas IGF-1 can suppress this inhibition. IGF-1 and mRNA levels are increased in OA articular tissue. IGF-1 can decrease the degradation and inhibition of synthesis induced by IL-1. IGF-1 release from chondrocytes is stimulated by IL-1. OA chondrocytes are hyporesponsive to IGF-1 which is excessively restricted by IGF binding proteins, which are also upregulated by cytokines such as IL-1. Proteases can also cleave these binding proteins, regulating their activity [11-12].
Changes of matrix degradation and calcification in Osteoarthritis
In OA, apoptosis reappears in the degenerated OA cartilage. There is also a marked increase in expression of type II collagen which are also a feature of the shift to hypertrophy in the growth plate by parathyroid hormone related peptide (PTHrP) [13]. In the partially calcified OA cartilage, there is a reactivation of endochondral ossification characterized by upregulation of type X collagen expression and duplication or replication of the tidemark, separating this zone from uncalcified cartilage. Vascular invasion from subchondral bone is reinitiated, resembling that seen in endochondral ossification. More than 90% of OA subjects show evidence for limited calcification of articular cartilages; there is also a high incidence of hydroxyapatite crystals in joint fluids [14].
Role of platelet rich plasma in OA
Platelet rich plasma contains a huge quantities of growth factors in small volume of platelet-plasma solution. The mechanism of PRP behind OA is due to the binding of growth factor to target cell receptor induces a signal transduction mechanism which produces a biological response for chemotaxis, cell proliferation and osteoblastic differentiation [15]. The molecular basis of platelet rich plasma is due to increased HGF and TNF-α activity by disrupting NF-κB-transactivating activity [16]. The half-life of growth factors is from minutes to hours. About 70% of growth factors are released from α granules of platelets within 10 minutes of the injection. These growth factors rejuvenate the diseased and degenerated tissues.
The platelet rich plasma act as a minimally invasive procedure which bridges the gap between pharmacological treatment and surgical treatment for osteoarthritis. It provides a strong and positive balance between pro-apoptotic and anti-apoptotic molecules, pro-inflammatory and anti-inflammatory cytokines & pro-angiogenic and anti-angiogenic factors for rejuvenation of degenerated cartilaginous tissues. Once PRP is activated, plasma fibrinogen polymerizes into a 3D fibrin scaffold, which contains heparan sulphate binding domains for growth factors, cytokines, chemokines, ECM components, cell adhesion molecules and acute phase proteins. This biodegradable 3D scaffold provides plastic-elastic stiffness and generates growth factors for cell proliferation, differentiation and migration. Once injected into the joint, 3D scaffold is converted into a viscous and malleable structure and further fibrinolysis begins and sustained release of growth factors occurs [17-18].
The growth factors rejuvenate the cartilage by producing IL-1Ra and other anti-apoptotic, anti-inflammatory and proangiogenic factors. The platelet rich plasma upregulates tissue inhibitor of metalloproteinases such as TIMPs -1, -3 and -4 by downregulating the signalling molecules of matrix metalloproteinases such as MMP-1, MMP-3, MMP-13 & MMP-28 and upregulation of ADAMTS-4 and 5 which lead to normal joint homeostasis [19].
Roffi et al [20] conducted a study on metabolism of chondrocytes and synoviocytes by freeze thaw method. They concluded decreased protein level secretion in freeze thawed PRP and increased ability to induce proliferation and production of extra cellular matrix components in chondrocytes and synoviocytes. Freeze thawed PRP has shown increased HGF expression in synoviocytes. They suggested cryopreserved PRP is a safe procedure, which preserves PRP quality and its biological activity [20].
Soo Jin Jang et al [21] studied the effectiveness of one dose of intra-articular PRP injections for early osteoarthritis in 65 patients who were evaluated at 1, 3, 6, 9 and 12 months after the procedure. They showed improvement of mean VAS score from 7.4 to 4.2 at 6 months follow up. The IKDC score showed a statistically significant outcome with p value < 0.05 [21].
Paterson et al [22] studied the effects of photo-activation of PRP and hyaluronic acid in osteroarthritis knee in 23 patients who were randomized into two groups. The use of low-level light irradiation to activate peripheral blood improve biological factors by decreasing proinflammatory cytokines (IL-2 & 6) and increasing the concentration of leucocyte-derived antiinflammatory factors (IL-1Ra). Out of 23 cases, 12 cases were randomized to the PA-PRP group and 11 cases were randomized to the HA group. The PA-PRP group demonstrated significant improvements in the VAS, KOOS Pain, KQoL Physical and KQoL Emotional subscales at 4 and 12 weeks. The PA-PRP group also significantly improved hoping and knee bends at 4 or 12 weeks. The HA group showed improvements on only the KOOS Function subscale at 12 weeks. There were no significant between-group differences at either time-point. They concluded that photoactivated PRP may provide a safe and effective novel treatment for knee OA [22].
In our study, the ultrasound evaluation of cartilage thickness increases post procedure in the group who received autologous platelet rich plasma therapy than who received corticosteroid injections. MRI scan of knee joint is the most sensitive and specific in assessing the thickness of cartilage. Here in this article, we compared autologous platelet rich plasma therapy and corticosteroid injection as the treatment modality for the patients with early knee osteoarthritis. The patients who received platelet rich plasma therapy showed improved range of movements by the end of 1st month follow up. Our study shows platelet rich plasma therapy for early knee osteoarthritis is superior with p value < 0.001 for VAS, WOMAC and KOOS score which is statistically significant than corticosteroid injection. Autologous PRP injection is 89.78% effective in patients with early knee osteoarthritis. The dose response relationship curve in autologous PRP for treating early knee osteoarthritis follow a sigmoid shaped kinetics.
Limitations
a) The dose and frequency of PRP have to be standardized.
b) The amount of growth factors injected to be quantified.
c) MRI scan of knee joint has to be documented before and after the procedure to view the cartilage thickness.
Further Research
To date, doxycycline is the only molecule that can regulate collagenase activities in vitro, control the progression of experimental OA, and be used without serious side effects in the treatment of knee OA [23]. In view of potency and upregulation in OA, IGF-1 is considered more potent growth factor which can renew matrix assembly and control degradation. The role of recombinant IGF-1 in OA has to be figured out and studied [24].
Conclusion
The autologous platelet rich plasma therapy is considered superior to corticosteroid injection for early knee osteoarthritis as platelet rich plasma injection provides growth factors for cartilage rejuvenation which has very limited regenerative potential. Platelet rich plasma therapy has become the biological novel agent in reducing pain and inflammation, rejuvenation of degenerated cartilage and improves the range of movements and quality of life in a long-term sequela in patients with early knee osteoarthritis.
References
- Martino MM, Briquez PS, Guc E, et al. (2014) Growth factors engineered for super-affinity to the extracellular matrix enhance tissue healing. Science 343(6173): 885-888.
- Rachita Dhurat, Sukesh MS (2014) Principles and Methods of Preparation of Platelet Rich Plasma: A Review and Author's Perspective. J Cutan Aesthet Surg 7(4):189-197.
- Engler AJ, Sen S, Sweeney HL, Discher DE (2006) Matrix elasticity directs stem cell lineage specification. Cell 126(4): 677-689.
- Sánchez M, Fiz N, Guadilla J, et al. (2014) Intraosseous Infiltration of Platelet-Rich Plasma for Severe Knee Osteoarthritis. Arthroscopy Techniques 3(6): e713-7.
- Anitua E, Zalduendo MM, Prado R, Alkhraisat MH, Orive G, et al. (2015) Morphogen and proinflammatory cytokine release kinetics from PRGF-Endoret fibrin scaffolds: evaluation of the effect of leukocyte inclusion. Journal of biomedical materials research 103(3):1011-1020.
- Mary B Goldring (2012) Articular cartilage degradation in osteoarthritis. HSS J 8(1): 7-9.
- Woessner JF (1991) Matrix metalloproteinases and their inhibitors in connective tissue remodeling. FASEB J 5(8): 2145-2154.
- Pelletier JP, DiBattista JA, Roughley P, McCollum R, Martel-Pelletier J, et al. (1993) Cytokines and inflammation in cartilage degradation. Rheum Dis Clin North Am 19(3): 545-568.
- Garniro P, Rousseau JC, Delmas PD (2000) Molecular basis and clinical use of biochemical markers of bone, cartilage, and synovium in joint diseases. Arthritis Rheum 43(5): 953-968.
- Caterson B, Flannery CR, Hughes CE, Little CB (2000) Mechanisms involved in cartilage proteoglycan catabolism. Matrix Biol 19(4): 333-344.
- Hang Fang, Lisi Huang, Ian Welch, Chris Norley, David W Holdsworth, et al. (2018) Early Changes of Articular Cartilage and Subchondral Bone in The DMM Mouse Model of Osteoarthritis. Scientific reports 8: 2855.
- Cugat R, Carrillo JM, Serra I, Soler C (2006) Articular cartilage defects reconstruction by plasma rich growth factors. In: Zansi S, Brittberg M, Marcacci M, eds. Basic Science, Clinical Repair and Reconstruction of Articular Cartilage Defects: Current Status and Prospects. Bologna, Italy: Timeo Edotore 801-807.
- Gobbi A, Bathan L (2009) Biological approaches for cartilage repair. J Knee Surg 22(1): 36-44.
- Hunter W (1995) On the structure and diseases of articulating cartilage 1743. Philos Trans R Soc Lond B Biol Sci 317: 3-6.
- Andia I, Maffulli N (2013) Platelet-rich plasma for managing pain and inflammation in osteoarthritis. Nat Rev Rheumatol 9(12): 721-730.
- Bendinelli P, Matteucci E, Dogliotti G, et al. (2010) Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: mechanisms of NF-κB inhibition via HGF. J Cell Physiol 225(3): 757-766.
- Gaissmaier C, Fritz J, Krackhardt T, Flesch I, Aicher WK, et al. (2005) Effect of human platelet supernatant on proliferation and matrix synthesis of human articular chondrocytes in monolayer and three-dimensional alginate cultures. Biomaterials 26(14):1953-1960.
- Eduardo Anitua, Ramon Cugat, Mikel Sanchez (2018) Platelet rich plasma in orthopaedics and sports medicine, Switzerland, Springer 7:125-136.
- Eduardo Anitua, Ramon Cugat, Mikel Sanchez (2018) Platelet rich plasma in orthopaedics and sports medicine, Switzerland, Springer 9:163-173.
- Roffi A, Filardo G, Assirelli E, et al. (2014) Does platelet-rich plasma freeze-thawing influence growth factor release and their effects on chondrocytes and synoviocytes? Biomed Res Int 692913.
- Soo Jin Jang, Jae Do Kim, Seong Sook Cha (2012) Platelet rich plasma (PRP) injections as an effective treatment for early osteoarthritis. Eur J Ortop Surg Traumatol 23(5): 573-580.
- Paterson L Kade, Nicholls M, Bennell KL, Bates Dan (2016) Intra-articular injection of photo-activated platelet-rich plasma in patients with knee osteoarthritis: a double-blind, randomized controlled pilot study. BMC Musculoskeletal Disorders 17: 67.
- Nüesch E, Rutjes AWS, Trelle S, Reichenbach S, Jüni P (2009) Doxycycline for osteoarthritis of the knee or hip (Review). The Cochrane Collaboration. The Cochrane Library 4: 1-26.
- Wei FY, Lee JK, Wei L, Qu F, Zhang JZ, et al. (2017) Correlation of insulin-like growth factor 1 and osteoarthritic cartilage degradation: a spontaneous osteoarthritis in guinea-pig. Eur Rev Med Pharmacol Sci 21(20): 4493-4500.






























