Excision of Enlarged Bursa While Undergoing Total Knee Arthroplasty
Olivia J Bono*, Tiffany M Feltman and James V Bono
Department of Orthopedic Surgery, New England Baptist Hospital, Boston, MA
Submission: June 01, 2018; Published: June 13, 2018
*Corresponding author: Olivia J Bono, Department of Orthopedic Surgery, New England Baptist Hospital, Boston, MA.
How to cite this article: Olivia J B, Tiffany M F, James V B. Excision of Enlarged Bursa While Undergoing Total Knee Arthroplasty. Nov Tech Arthritis Bone Res. 2018; 3(1): 555602. DOI: 10.19080/NTAB.2018.03.555602
Abstract
Total Knee Arthroplasty (TKA) is a long-recognized surgery for treatment of end stage osteoarthritis caused by many different factors. This procedure is one that is well known and well utilized. A predicament arises when the patient is also complaining of another issue associated with his operative leg. In this unique case, the patient had a large, painful bursa on the operative leg. This case report will show the complications that can occur when performing both procedures at the same time.
Introduction
Joint replacement surgery can be simple or complex. Additional procedures can be required at the time of the index arthroplasty such as removal of hardware, decompression of a Baker’s cyst, or excision of a prepatellar bursa. The surgeon must decide to stage the two procedures or to perform them simultaneously. Simultaneous surgery has the advantage of one anesthesia and rehabilitation. Staged procedures may be considered when the cumulative time of both surgeries is considered excessive, or if the ability of a skin incision to heal is in question. With hardware removal, bone defects are encountered which render the patient susceptible to periprosthetic fracture. It is advisable in certain cases to delay subsequent joint replacement until these stress risers are normalized.
Case Report
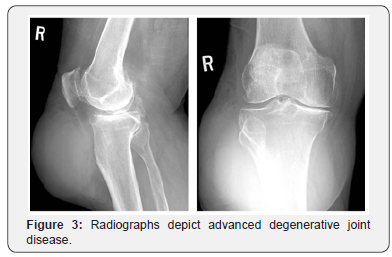
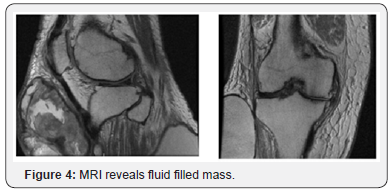
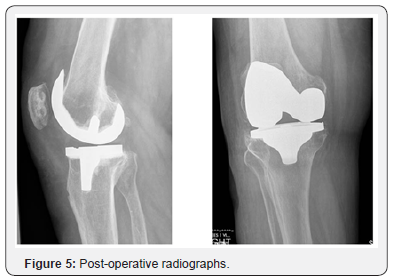
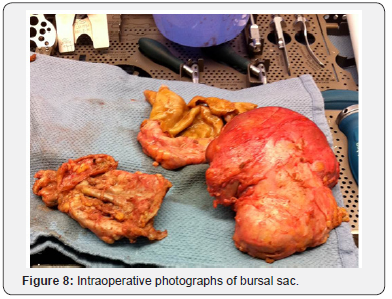
A 74yr male with a past medical history of osteoarthritis bilateral shoulders, coronary artery disease, congestive heart failure with cardiomyopathy, hypertension, peptic ulcer disease, gastric reflux, type 2 diabetes mellitus, gout and varicose veins presented with chronic right knee pain with associated subcutaneous bursa on his right leg that had been progressively increasing in size for 8-9 years (Figures 1-4). As the bursa could be decompressed entirely from an anterior midline incision, it was decided by the surgeon that the bursa would be removed at the same time as the total knee arthroplasty. The patient underwent excision of a massive subcutaneous bursa found over the anterolateral and posterolateral aspect of the leg (Figures 5-8) utilizing a midline incision, following which a total knee arthroplasty was performed using a medial parapatellar arthrotomy. The tourniquet was inflated during the procedure and was released before closure with a tourniquet time of 110 minutes. The wound was closed in layers over four 1/8th inch hemovac drains (2 placed in the joint and 2 placed in the bursal cavity).




Postoperatively the patient was sent to PACU and then to the floor. There were no major issues throughout his hospital stay. His incision throughout his hospital stay remained unremarkable. There was no erythema, drainage, or evidence of wound complication. His dressing was changed daily. Drains were removed on P.O.D #2. He was then discharged to a rehab facility on P.O.D #3 and remained on adjusted dose Coumadin for 4 weeks for DVT prophylaxis. After a lunch tray fell onto his knee at the rehab facility on POD #9, the patient noted swelling of the right leg, and he was transferred to New England Baptist Hospital (Figures 9-12). His exam revealed a large, firm soft tissue mass and swelling approximately 20 x 15 cm over his right proximal lateral leg. There was an area of ecchymotic darkened skin and a 5 cm dark bulla over the center of the ecchymosis. The mass was firm and tender upon palpation. There was also a 1 cm area of duskiness over the mid-lateral aspect of the incision. There was no drainage noted from the incision. The patient’s labs upon admission were unremarkable and a bedside aspiration was done in attempt to decompress the hematoma. However, only 2cc bloody fluid was obtained. Silvadene dressing changes were initiated.



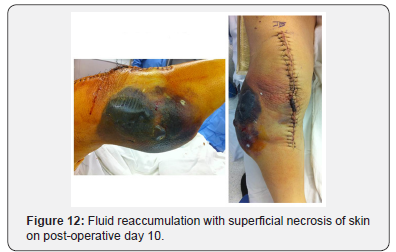
On P.O.D. #10, the patient was taken to operating room for exploration and evacuation of the hematoma. The hematoma was 10-12 cm in diameter. An incision was made on the lateral portion of the hematoma measuring 4-5 cm (Figure 13). The hematoma was decompressed, and the fascia was closed and covered with gel foam. Two Jackson-Pratt drains were placed, and the incision was closed. Post-operatively the patient had twice a day dressing changes with Silvadene. The drains were removed on P.O.D. #15. Upon discharge on P.O.D. #20, the incision was well approximated, and the sutures were removed. The wound at the middle portion remained bruised and skin slightly macerated, but without erythema or drainage. The middle and lateral aspect of the knee is with a darker discoloration. The patient slowly healed the necrotic areas (Figures 14-17) without needing any further surgical intervention.





Discussion
The patient presented with two diagnoses: osteoarthritis of the knee and a massive subcutaneous bursa. There were two surgical options considered: one simultaneous procedure or two staged procedures. After discussion with the patient, simultaneous bursal excision and total knee arthroplasty was undertaken from a single midline incision. Despite the use of deep and superficial drains, a massive hematoma developed which resulted in pressure necrosis of the skin. Although the hematoma was unanticipated, the amount of dead space was considerable, and the risk of hematoma was underestimated. After a thorough literature search, no paper on this complication has been described. The vascular supply to the skin around the anterior knee is from the descending branch of the lateral circumflex, the genicular branches from the popliteal artery, and the anterior tibial recurrent artery. Perforators from these vessels travel through the fascia to form an anastomotic ring. As the vastus medialis extends more distally than the vastus lateralis, this provides the medial side more muscle coverage and less chance of vascular disruption than the lateral aspect of the knee as it is more dependent on the subdermal plexus [1].
Vascular disruption of the lateral portion of the wound is seen most frequently with lateral release when performed during total knee arthroplasty for patellar tracking. If the superolateral geniculate vessels are divided, this can have a profound effect on postoperative wound discoloration and can decrease the viability of the lateral skin edges [2]. Another approach to this patient would have been to use multiple incisions: one to excise the bursa and a separate incision to perform the knee replacement, while maintaining at least a 7 cm skin bridge between incisions. A separate lateral incision in this patient could have potentially caused a further decrease in the vascularity of the prepatellar skin, especially in light of his diabetes which is associated with a higher incidence of wound complications [3,4]. In retrospect, we would recommend a staged approach to total knee arthroplasty with an associated massive subcutaneous bursa. The bursa can be approached through a midline incision, excised in its entirely, and closed over drains with a compressive dressing for several weeks. After complete healing of the wound (6-12 weeks), total knee arthroplasty can be performed in a routine manner through the same midline incision.
References
- Garbedian S, Sternheim A, Backstein D (2011) Wound Healing Problems in Total Knee Arthroplasty. Orthopedics 34(9): 516-518.
- Johnson DP, Eastwood DM (1992) Lateral Patellar Release in Knee Arthroplasty: Effects on Wound Healing. J Arthroplasty 7: 427-431.
- Galat DD, Mc Govern SC, Larson DR, et al (2009) Surgical Treatment of Early Wound Complications Following Primary Total Knee Arthroplasty. J Bone Joint Surg Am 9(1): 48-54
- England SP, Stern SH, Insall JN, et al (1990) Total Knee Arthroplasty in Diabetes Mellitus. Clin Orthop Relat Res 260:130-134.






























