Intramedullary Injection of Processed Autologous Bone Marrow in the Treatment of Cases with Impaired Bone Healing in Long Bones
Reynders-Frederix Peter1*, Reynders-Frederix Cristina2, Reynders-Frederix Nathalie3, Jose Saldana Diaz3 and IllésTamàs4
1Department of Orthopedics & Traumatology, University Hospitals Brussels, Belgium
2Department of Musculo-Skeletal Rehabilitation, University Hospitals Brussels, Belgium
3Department of Economics & Biostatistics, University of Calgary, Canada
4Department of Orthopedics & Traumatology, University Hospitals Brussels, Belgium
Submission: January 24, 2018; Published: February 06, 2018
*Corresponding author: Reynders Frederix Peter, Department of Orthopedics & Traumatology, University Hospitals Brussels, Brussels 1020m, Belgium; Tel: 32473361420; Email: rejmders52@hotmail.com
How to cite this article: Reynders-F P, Reynders-F C, Reynders-F N, Jose S D, IllÚsT. Intramedullary Injection of Processed Autologous Bone Marrow in the Treatment of Cases with Impaired Bone Healing in Long Bones. Nov Tech Arthritis Bone Res. 2018; 2(4) : 555594. DOI: 10.19080/NTAB.2018.02.555594
Abstract
The aim of the study was to assess the efficiency of intramedullary injected, processed, autologous bone marrow via a delivery system composed of cannulated 7.3mm screws in the treatment of delayed-union and non-union of the tibia, femur and humerus. Design: consecutive case series, we treated 63 patients. Forty bone healing problems at the tibia, twenty-one bone healing problems at the femur and two delayed bone healing at the humerus. End point of the study was the necessity of an additional therapy to accelerate bone healing. With 36 patients the bone marrow injection was used as a stand-alone therapy. In 23 patients the BMA injection was associated with an exchange stabilization of the fracture site. In four patients, autologous bone grafting (on lay grafts) was added as concomitant therapy. Forty-six patients (74%) healed. Of the 17 patients who needed an additional surgery, 15 were smokers.
When smokers were excluded, the results were even better: 88% obtained bone healing. Quantity of the total nucleated cells and osteoblastic progenitors which express alkaline phosphatase (CFU-Aps) was lower in the refractory group especially with the smokers. We concluded that the intramedullary injection, via cannulated ported screws, of processed autologous bone marrow can heal delayed- and nonunion of the tibia and femur and humerus.
Introduction
Despite the progress in our understanding how bone fracture heals, no optimal treatment with ideal results exist. The number of fractures with impaired bone healing remains constant at 10% [1]. This is partially due to the heterogeneous nature of the energy absorption during injury, the individual patient differences, co-morbidities, different degrees of patient compliance and understanding, medication use/misuse of tobacco and alcohol abuse [2]. This heterogeneous nature of osseous and per-osseous lesions make comparisons between trauma patients in clinical research very difficult. Treatment options for impaired bone healing are; exchanging the implant, bone grafting (autologous and heterologous) and low intensity pulsed ultra-sound therapy for special indications [3-5]. Since the bench mark publication of Connolly JF in 1991 renewed interests in less traumatic and biological approaches in treatment of impaired bone healing have started. Several authors claimed good clinical outcome after percutaneous injection of autologous bone marrow and bone marrow concentrate in fracture zones affected by impaired bone healing [7-9].
This technique of percutaneous injection of fluid in a nonunion side is in theory feasible but in practice rather difficult. The tri-dimensional orientation of the fracture site is often difficult to visualize on image intensifier, making entering percutaneous into the non-union site extremely hard. Also the non-union site is often filled with dense fibrous tissues which make injecting large volumes of bone marrow or bone marrow concentrate into the non-union site less reproducible. That’s why the authors changed their technique of delivering the bone marrow fluid by using ported screws placed in the metaphyseal area beneath and above the non-union site.
Material & Methods
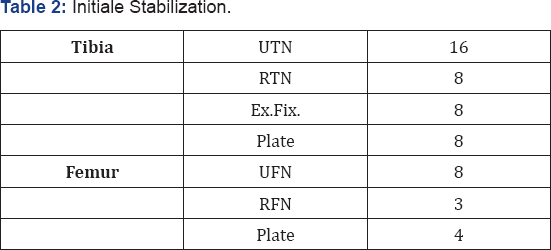
In total, 63 cases with an average age of 33 years (17-62) were included in this series: Table 1. Our definition of delayed union is bone healing which is not achieved after six months but still evolving. Non-union, is a union that is not achieved after nine months, post fracture, with no apparent evolution. In these series delayed unions without pain on weight bearings were excluded also fractures associated with a CRP more than 14 gr/L. In 35 cases, initial stabilization was intra-medullary nails. In 14 cases were plates and in 8 cases, external fixators: table 2. In 36 cases, bone - marrow concentrate was used as a standalone procedure. In 24 cases bone-marrow injection was associated with an exchange of the implant , due to stability reasons. In three cases bone-marrow injection was combined with autologous bone grafting.

Surgical technique
The technique consisted in taking > 250 cc of bone marrow through multiple small-volume aspirations from changing locations of harvest of the posterior iliac crest to avoid bone marrow dilution. The diluted (with peripheral blood) bone marrow was then collected in a sterile glass bottle with 30 ml (30.000 units) ofNa-Heparine. The recipient was sent immediately to the lab and centrifuged at 1500rpm for 10 minutes with the Cobe 2991 centrifuge cell processor (TerumoBCTHaasrode- Belgium). Mono-nuclear cell preparations were isolated with the use of Ficoll-Paque (density 1.073 g/ml; GE Healthcare Life Sciences, Uppsala, Sweden) (Figure 1). An average of 50 cc's of mono-nuclear cells were sent back and injected via ported screws of 7.3 mm (Synthes, Brussels-Belgium). The screws were placed in the epi-metaphyseal area above and below the nonunion side see Figure 2.


Total mononuclear count
The buffy coat was isolated and re-suspended in complete medium. WMEM containing IOYD fetal bovine serum ((Bio- Whittaker Alpha MEM; Lonza, Verviers, Belgium), 50 mg/ml sodium ascorbate, 1% GIBCO GlutaMAX (LifeTechnologies, Paisley, Scotland), was then incubated at 37 C° in a humidified atmosphere with 5% CO2. The number of nucleated cells in each aspirate was then counted.
Colony formation assay
A colony formation assay was used to assess the connective tissue progenitor yield from the different isolation sites. Duplicate aliquots of mono-nuclear cells were plated at low density (1.5 • 105 cells per 10-cm-diameter culture dish [ThermoFisher, Waltham, MA, USA) with 15 mL of complete medium. Cells were cultured for fourteen days, then fixed with methanol and stained with methylene blue. Cultures were harvested and stained for alkaline phosphatase (AP) on day 1, 3, and 6. The number of attached single cells was counted on day-1 slides. The number of CFU- AP was counted on days three and six.
Results
Number of nucleated cells
For the entire group of 63 patients, an average of 292 million nucleated cells were harvested per ml aspirate S.D. 122, median 280 range (202 to 356).
i. For the bone healing group: the total mononuclear cells counted were 340 million per cc aspirate S.D. 75, median 320 range (280 to 420).
ii. For the failure group: the total mononuclear cells count was 163 million per ml aspirate. S.D 95, median 123 range (75 to 260).
There was a clear difference between the two groups, but it didn't reach a significance.
Total CFU-AP per aspirate
Total CFU-APs per aspirate is the product of the total number of nucleated cells per aspirate (in millions) and the prevalence of CFU-APs per million mononuclear cells. For the entire group of 63 patients an average of 8424 CFU-APs was harvested per aspirate S.D. 9300, range -10 to 22800, median 3100).
i. For the bone healing group: the total CFU-AP's per aspirate counted was 34075 per aspirate S.D. 20512, median 29686 range (2630 to 18536).
ii. For the failure group: the total CFU-AP's per aspirate was 8665 per aspirate. S.D 2513, median 7882 range (5600 to 11523).
There was a clear difference between the two groups, which reach a great significance. p< 0.001 .
Surgical results
In the end, 17 patients out of 63 didn’t heal which comes out to be just 27%. In the failure group, 14 patients had a tobacco addiction (> one package of cigarettes a day). In the bone healing group of 46 patients, 15 smoked cigarettes every day. The average age of the total cohort was only 33 years. As a result, we did not find individuals with confounding clinical variables such as a systemic disease known to affect bone, local bone disease or previous trauma in the region of the iliac crest, serious ongoing blood loss or individuals taking medications known to affect bone metabolism (e.g., corticosteroids, thyroxin, estrogen, or chemotherapy, antibiotics). Apparently the only difference between the two groups was the tobacco use. Alcohol consumption was not to ask for.
Discussion
Although the enormous progress made in the understanding of impaired bone healing, no definite treatment of non-unions exist. Globally, 10 % of all long bone fractures will develop an impaired healing. For adequate bone healing, one needs to re-establish the biology of the fracture site (cell recruiting molecules, bone matrix, osteogenic cells & vascularity) together with sufficient stability. This concept is better known as the diamond concept of Giannoudis [10]. Unfortunately some confounding variables are present after bone trauma, which are difficult to control. One big issue is the patient with his co morbidities, medication intake, lack of compliance (use of tobacco and alcohol consumption) and misunderstanding of the treatment outcomes. Another variable which we can't control is the impact itself. The energy absorbed during the incident will dictate the tissue damage. If one considers a bone fracture as a soft tissue problem where a bone fracture happens to be, one can easily understand the mosaic of different problems encountered in the healing process of long bone fractures.
There’s a myriad of treatment options: or we need to improve the biology of the fracture site. This is often done via autologous bone grafting procedures. In cases of heavy sequesters, debridement of this necrotic tissue and reconstruction of the bone defect with autologous bone grafts, according to Masquelet's [11] technique, is often needed. Sometimes the soft tissue envelope is so scarred up that a free muscular flap is needed to create a better vascular environment for hosting the bone graft. Good results are also seen with ultra-sound therapy. This non-invasive treatment works better if there is no implant in site. The other arm of treatment approach is the techniques to improve stability.
Classically this means the exchange of the implant, often intra-medullary nail by another implant, nail. There is some evidence to support this strategy. Often this implicates the use of thicker nails and extensive reaming to "irritate" the periosteum. In some respect this exchange nailing is a combination of biological and mechanical approache of the problem. In a large series of Jiangying Ru et al. [12-15]. The authors compared one group of femoral non-unions treated by exchange nailing N=87 (ERN) with another group of N= 93 cases treated with augmentative compression plating (ACP). With augmentative compression plating, the authors put a plate onto the femur without disturbing the existing intra-medullary nail.
Their results were impressive. In the ACP, group healing was 100 % while in the ERN group, only 86% could be healed. In our study of 63 consecutive cases of tibial and femoral non-union, we used the technique which was described by Connolly JF in 1991. Although percutaneous application of autologous bone marrow grafting is appealing as an alternative to the existing open technique with negligible complications, only a few reports in literature support this less invasive technique .The efficacy of the procedure was confirmed experimentally by Paley et al. [12]. Percutaneous bone marrow grafting seems to be a simple and straight-forward technique. In our hands we found it difficult in terms of reproducibility of the technique. Finding the non-union site is not easy in absence of some fracture gap. Also injecting large (>50 ml)quantities of bone marrow in and around the nonunion site is seldom possible.
To overcome this problem Calori et al. [13] created a biochamber by pre-drilling a tunnel on image intensifying control into the non-union site, injecting the cells precisely in the target area. Also cells were injected around the non-union site in the same procedure. The authors developed a simple adjustment of the bone marrow injecting technique by delivering the bone marrow > 50 cc through two ported screws of 7.3 mm above and below the non-union site. During this procedure, we needed to block the other screw for preventing the bone marrow to escape the medullary space. Proving the patency of the medullary canal bypassing the nonunion site. Even with the intramedullary nail in place we managed easily to bypass the nail in the metaphyseal area of the long bone.
In the analysis of the total nuclear count and the osteogenic connective progenitors, we were able to make a fair distinction between the smoking and non-smoking group. Interestingly in the smoker's cohort of the healed group, no differences were seen with the other cases in this healed cohort. So perhaps other confounders play a major role in the healing personality of these fractures. A serious limitation of this study was the lack of data on alcohol consumption. We know from the recent work of Keaton Patel [14], and coworkers working with mice, that alcohol produces a acetaldehyde which can lead to permanent genetic damage in the DNA of stem cells. In conclusion; this series shows the interesting results of injecting large quantities of processed bone marrow via a novel delivering system. Inour series we saw less results in the pre-dominant group of smokers (73%) versus 88% in the non-smoking group.
However taking into consideration that in the group of 14 smokers in the healed cohort there was no difference in total mononuclear count, nor CTP-AP's. We expect other factors to play a major role in the failure of the bone marrow injections technique.
References
- Tzioupis C, Giannoudis PV (2007) Prevalence of long-bone non-unions.Injury 38 (Suppl 2): S3-S9.
- Giannoudis PV, Calori GM, Begue T, Schmidmaier G (2013) Bone regeneration strategies: current trends but what the future holds? Injury 44 (Suppl 1): S1-2.
- Trafton PG (1998) Tibial Shaft Fractures. In Skeletal Trauma vol23. p. 2187-2293.
- Einhorn TA (1995) Enhancement of fracture-healing. J Bone Joint Surg Am 77: 940-956.
- Leighton R, Watson JT, Giannoudis P, Papakostidis C, Harrison A, et al. (2017) Healing of fracture non-unions treated with low-intensity pulsed ultrasound (LIPUS). A systematic review and meta-analysis. Injury 48(7): 1339-1347.
- Connolly JF, Guse R, Tiedeman J, Dehne R (1991) Autologous marrow injection as a substitute for operative grafting of tibialnonunions. Clin Orthop Relat Res 259-270.
- Muschler GF, Boehm C, Easley K (1997) Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am 79: 1699-1709.
- Hernigou P, Mathieu G, Poignard A, Manicom O, Beaujean F, et al. (2006) Percutaneous autologous bone-marrow grafting for nonunions: surgical technique. J Bone Joint Surg Am 88 (Suppl 1): 322-327.
- Matheus Guimaräes JA et al. (2014) Injury Int J Care Injured 45 S5 S7-S13.
- Giannoudis PV, Ahmad MA, Mineo GV, Tosounidis TI, Calori GM, et al. (2013) Subtrochanteric Fracture Non-unions with implant failure managed with the "Diamond Concept”. Injury 44 (Suppl.1) : S76-81.
- Klaue K, Masquelet AC, Perren S, Knothe U, Anton C (2009) Bone Regeneration in long-bone defects; tissue compartmentalization?In vivo study on bone defects in sheep. Injury 40: S4, S95-S102.
- Paley D, Young MC, Wiley AM, Fornasier VL, Jackson RW (1986) Percutaneous bone marrow grafting of fractures and bonydefects. An experimental study in rabbits. Clin Orthop Relat Res Pp. 300-312.
- Calori GM, Giannoudis PV (2011) Enhancement of fracture healing with the diamond concept: the role of the biological chamber.Injury 42: 1191-1193.
- Juan I. Garaycoechea et al. (2018) Nature.
- Jiangying Ru et al. Personal Communications.






























