Imaging Study of a Meniscal Transplant: A Novel Technique
Khizer Razak1, Surbhi Gupta2 and GL Meena3*
Department of Radiodiagnosis, SP Medical College, India
Submission: November 13, 2017; Published: December 06, 2017
*Corresponding author: GL Meena, Department of Radiodiagnosis, Sardar Patel Medical college, Bikaner, Rajasthan, India, Email: meenabkn@yahoo.co.in
How to cite this article: Khizer R, Surbhi G, GL Meena. Imaging Study of a Meniscal Transplant: A Novel Technique. Nov Tech Arthritis Bone Res. 2017; 2(3) : 555587. DOI: 10.19080/NTAB.2017.02.555587.
Abstract
Aim & Objectives: The meniscal transplant has been proposed for the symptomatic relief of young patients with meniscal pathology and to prevent the risk of early joint degeneration. We review the indications, techniques and complications of this procedure and describe the most important radiological findings.
Material & Methods: We retrospectively reviewed the meniscus transplants performed at Dept. of Radio diagnosis P.B.M hospital, Bikaner, with a minimum follow-up of 1 year using adiography, magnetic resonance and / or MR arthrography. The results of 10 patients with an average age of 34.5 years (21-45) were analyzed [1].
Conclusion: The radiologist must know the surgical technique of meniscal transplantation and be familiar with the normal findings of posttransplant imaging in MRI for the accurateevaluation of these patients and recognize the signs of probable complications. It is very important to correlate the morphological alterations with the patient’s clinic.
Keywords: Meniscus; Imaging; MR; Technique
Introduction
The main indications of meniscal transplantation are limited to patients <50 years old and with:
a. Postmeniscectomy symptoms.
b. Unicompartmental pain that does not improve with conservative treatment, which makes it impossible to carry out the activities that the patient usually performed and without other relevant pathological findings.
c. Meniscal injury associated with another pathology (ACL insufficiency, malalignment, signs of joint instability).
The ideal candidate for a meniscal transplant would be a young patient under 45 years of age, with stable knee and athlete with a history of meniscectomy.
The contraindications are the following:
a. Pre-existing inflammatory arthritis (RA)
b. Degenerative, postinfectious or metabolic joint disease.
c. Obesity
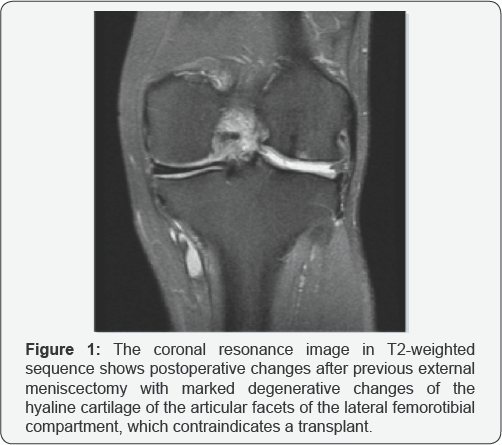
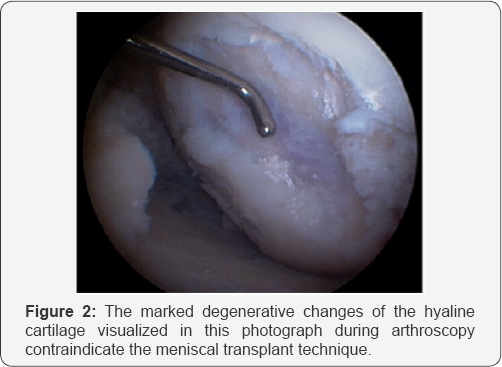
d. Major cartilage damage (advanced joint degeneration (Outerbridge> 2) (Figures 1 & 2).
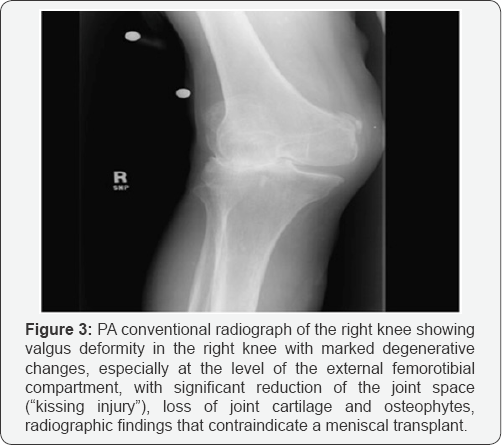
e. Changes grade III-IV of Fairbank in tibia and femur (lesions "in kiss") (Figure 3).
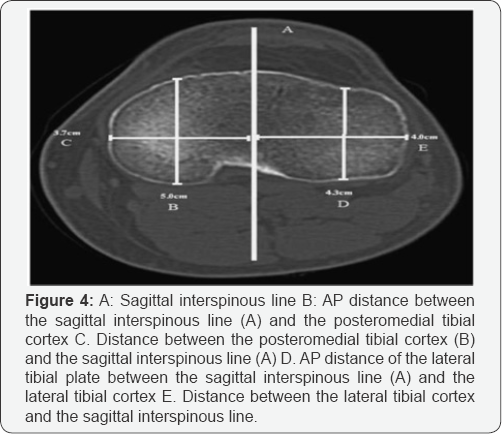
For the presurgical measurement of the meniscal graft, the simple radiograph has been shown to be the most accurate method (Figure 4).
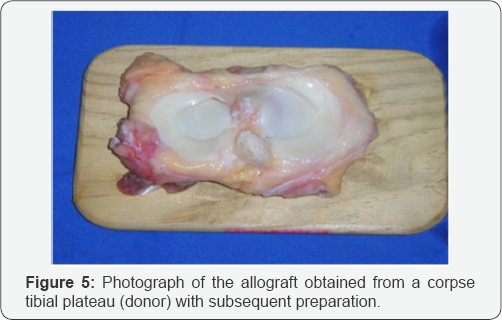
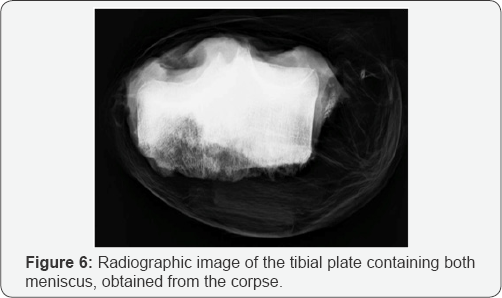
The allograft is obtained from the tibial plate of the corpse (Figure 5 & 6), it is kept frozen at -80°, thus maintaining the collagen but the donor cells are destroyed (they remain almost acellular, which conditions a minimum risk of immunological rejection).
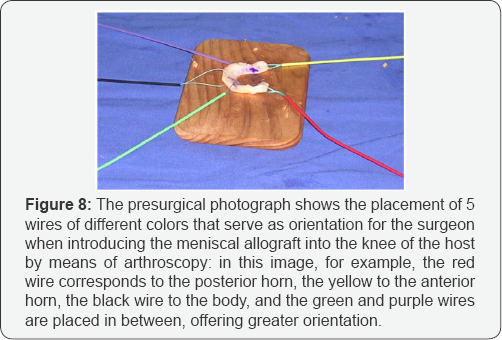
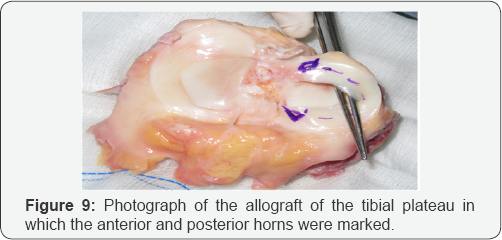
Given the limited visualization of the surgical field offered by arthroscopy, the preparation of the allograft requires a precise location in the space to facilitate the orientation of the surgeon: with cable markings of different colours (Figure 7) and identifying the anterior and posterior horns (Figures 7 & 8), we proceed to the preparation of the allograft for its correct localization during the procedure (Figures 8 & 9).

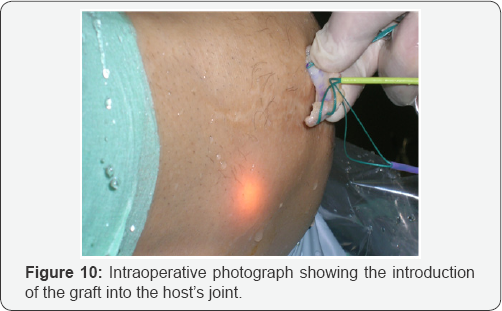
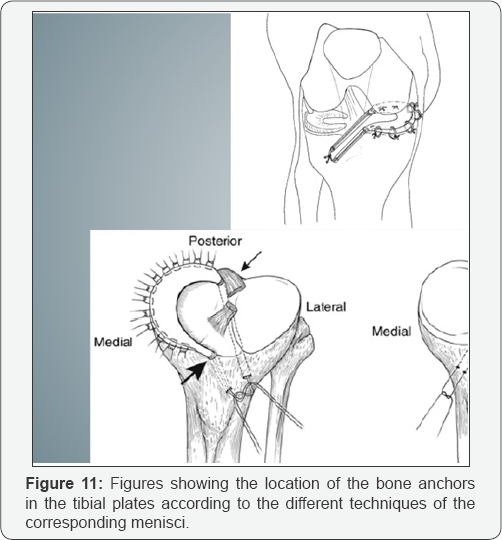
The graft bed should be properly prepared to facilitate healing. Debridement of the meniscal remnant and scar tissue is performed. In the periphery, the meniscus is sutured to the capsule. The meniscal transplant is performed arthroscopically (Figure 10) assisted with small cutaneous injections (<12mm). The standard techniques are based on the solid bony fixation of the meniscal horns (Figure 11).
There are different methods for the two meniscus allowing a correct anatomical location of the meniscal horns:
i. For the internal meniscus the method with double bone pill is used; Tunnels are drilled at the corresponding anatomical sites of the recipient's meniscal horns, and the bone pellets are inserted into the host bone with sutures passed through the tunnels that are tied around an anterior bridge of tibial bone.
ii. However, given the proximity of the horns of the lateral meniscus, the "keyhole" technique is used, in which a graft is placed that has a bony bridge connecting the anterior and posterior horns. This block of bone, or bridge, conforms and adapts to a similar tunnel ("keyhole") carved into the anterolateral plateau of the recipient.
The maintenance of the natural insertion of the meniscus [2] to the bone reduces the risk of extrusion of the graft towards the medial and lateral leak, which leads to its failure. Also, the native inserts allow a correct mobility of the meniscus.
Material & Methods
We retrospectively reviewed the meniscus transplants performed at Dept. of Radio diagnosis P.B.M hospital, Bikaner with a minimum follow-up of 1 year using radiography, magnetic resonance and / or MR arthrography. The results of 10 patients with an average age of 34.5 years (21-45) were analyzed.
Results
The 10 patients have been treated successfully and none of them has presented affectation of the joint space 5 years after the transplant. If the indications are respected and with a correct procedure, the clinical results are good in 90% of the cases [3].
As imaging tests are used
i. Conventional radiography
ii. Magnetic resonance or arthro-CT
iii. Direct visualization by arthroscopy.
The following radiological findings must be taken into account:
Normal (not to be confused with pathological findings):
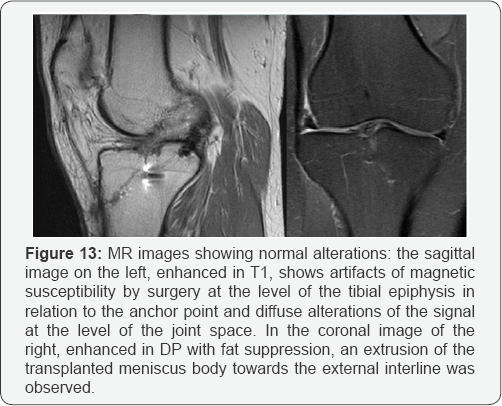
i. The presence of mild signal hyperintensity (Figure 12) and a certain degree of extrusion of the transplanted meniscus (Figure 13) should be considered normal and should be distinguished from disinsertion.
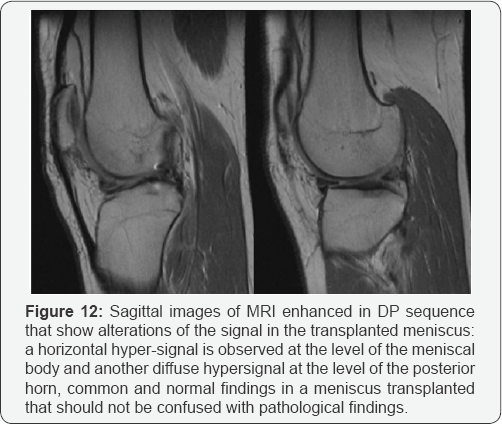
ii. Slight irregularities of the free edge of the transplanted meniscus [4].
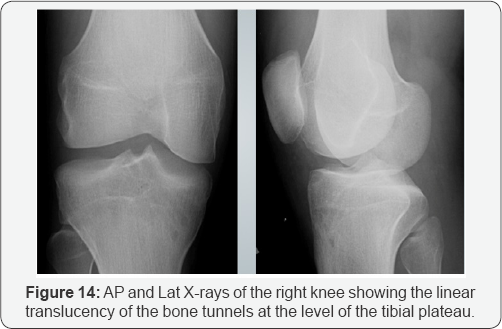
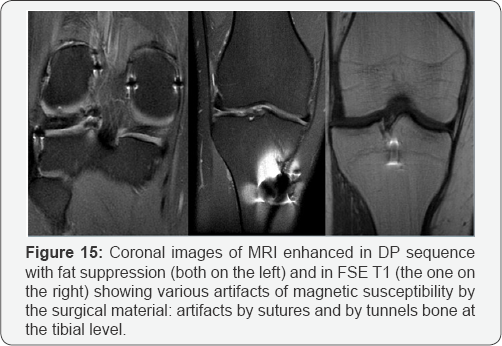
iii. Expected postoperative changes (Figure 14) and micrometallic artifacts due to surgery (Figure 15).
Complications to rule out radiologically are:
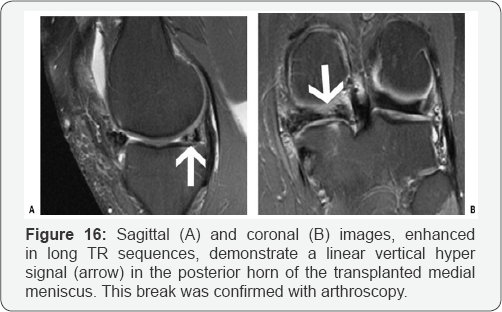
i. New meniscal tear (Figure 16)
ii. Size reduction (meniscal degeneration)
iii. Arthrofibrosis
iv. Hematoma
v. Infection.
Conclusion
The radiologist must know the surgical technique of meniscal transplantation and be familiar with the normal findings of posttransplant imaging in MRI for the accurate evaluation of these patients and recognize the signs of probable complications. It is very important to correlate the morphological alterations with the patient's clinic.
The allogeneic meniscal transplant is a novel and complex therapeutic alternative that requires a good multidisciplinary collaboration and that with an appropriate selection of patients shows good results in the medium term in the series that we present. However, we will have to wait for the long-term results [5,6].
References
- Angela G Gopez, Eoin C Kavanagh (2006) MR Imaging of the Postoperative Meniscus: Repair, Resection, and Replacement. Semin Musculoskelet Radiol 10(3): 229-240.
- Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, et al. (1995) Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy 11(4): 386-394.
- Veltri DM, Warren RG, Wickiewicz TL, O'Brien SJ (1994) Current status of meniscal transplantation. Clin Orthop Relat Res 303: 44-45.
- Garrett JC, Aichroth PC, Canon WD, Patel DV (1997) Meniscal transplantation. In Knee Surgery. Current Practice. Kolln deutscher Arzteverlag. Faven, New York, USA, 1992: 95-103.
- Cameron JC, Saha S (1997) Meniscal allograft transplantation for unicompartmental arthritis of the knee. Adv Orthop Surg 21: 91-92.
- Jon K Sekiya, Christopher I, Ellingson MD (2006) Meniscal Allograft Transplantation. J Am Acad Orthop Surg 14: 164-174.






























