Laser Therapy and Osteoarthritis Disability: An Update of an Unresolved Topic
Ray Marks*
Department of Health and Behavior Studies Teachers College, Columbia University and Department of Health and Physical Education, Gerontological Studies and Services, York College, CUNY, New York, USA
Submission: November 11, 2017; Published: December 01, 2017
*Corresponding author: DR. Ray Marks, Department of Health and Behavior Studies, Teachers College, Box 114, 525 West 120th Street, New York, USA, Tel: 212-606-1211; Fax: 212-678-8259; Email: rm226@columbia.edu; rmarks@york.cuny.edu
How to cite this article: Ray M. Laser Therapy and Osteoarthritis Disability: An Update of an Unresolved Topic. Nov Tech Arthritis Bone Res. 2017; 2(2) : 555585. DOI: 10.19080/NTAB.2017.02.555585.
Abstract
Laser therapy, initially reported to be extremely successful in Russia and Eastern Europe has been used for some time with no definitive consensus on its utility. The present review extends the search for research on this topic beyond 1998 when a prior analysis was done. The aim was to examine the support for continuing to research this topic. To arrive at a salient set of conclusions and research recommendations all relevant controlled clinical trials and related basic research published in English-language publications between 1980-2017 were examined. Employing the PUBMED, Scopus, Web of Science, and Academic Search Complete data bases available experimental studies tend to continue to support current findings of post-treatment clinical improvements in symptoms associated with osteoarthritis, including pain, mobility, and function, with few adverse effects. It is concluded that despite prior conclusions that laser therapy is no better than placebo, the current data base affords a much more positive view from a diverse body of related research. Moreover, laser therapy in its various forms can be expected to offer some advantages to the osteoarthritic patient relative to other forms of treatment, or can supplement treatments, thereby raising their effectiveness. Hence the idea that laser therapy may be helpful in postponing joint replacement surgery seems worthy of more attention.
Keywords: Articular cartilage; Efficacy; High intensity laser; Inflammation; Intervention; Low-level laser therapy; Osteoarthritis; Pain
Introduction
Osteoarthritis, the most prevalent joint disease, continues to cause immense physical challenges to the affected individual, as well as enormous economic and social costs. Predominantly affecting the articular cartilage lining of synovial joints [1] recent work in this realm has shown the entire joint including the subjacent bone, the joint capsule and its synovial lining, plus the ligaments supporting the joint, along with the surrounding muscles are all implicated in its progressive pathology and oftentimes periods of intractable pain [2]. Hence therapies that can not only minimize pain, but can also target the multiple biological changes found in osteoarthritic cartilage, as well as those occurring in the surrounding bones, muscles, synovia, and ligaments can be regarded as being highly desirable. Among the various approaches that can potentially intervene positively in reversing or ameliorating some of this associated pathology has been low level laser therapy, and more recently high intensity laser therapy [3].
In particular, the ability of laser light interventions to assist in reducing capsular thickening, inflammation and accompanying adverse bone and muscle alterations, which has been demonstrated in preclinical studies, appears very promising for potentially alleviating the signs and symptoms of osteoarthritis joint pathology, as well as for optimizing cartilage integrity [1,3]. In a disease where even the presence of any decreased willingness to move [4] may inhibit any potential cartilage repair mechanisms and add to its dissolution or vulnerability, the application of a non-invasive form of therapy, such as laser therapy, might not only prove highly beneficial, but could have far-reaching beneficial quality of life implications, among others.
Yet, despite decades of promising research, this physical modality remains unlisted among the multiple evidence-based guidelines for treating osteoarthritis recently outlined by Martel-Pelletier et al. [2]. Moreover, even though laser therapy has been shown efficient means of reducing pain and disability that does not impact cartilage or other body systems adversely [5,6] the clinical efficacy of laser therapy has been disputed and its benefits have been attributed to its strong placebo effect, among others. This confusion, which was reflected in a report conducted almost 20 years ago appears highly important to resolve not only because the lack of clarity clearly has a negative bearing on opportunities for potentially ameliorating osteoarthritis symptoms in some cases, an area in great need of advancement, but is clearly somewhat due to the challenges in synthesizing the available data or deriving conclusions from isolated rather than all available data sources. It also shows clinicians may need to firstly become more familiar with the laboratory studies in any area such as laser, and begin to apply some of the understandings from basic research to advance the clinical field of endeavor in this area.
Indeed, a plethora of preclinical laser oriented studies, that have used animal models of osteoarthritis support a variety of favorable bio-stimulatory effects of laser light on osteoarthritic joint tissues. These include, but are not limited to, the stimulation of specific cell organelles and membranes in subcutaneous tissues at a molecular level, including favorable alterations of membrane potential and enzyme activity [7], phagocytosis, neurotransmitter release, and collagen, protein and ribonucleic acid (RNA) synthesis [8], plus synthesis of intercellular cartilage matrix without evidence of increased matrix catabolism [9]. In addition, laser therapy appears to produce a profound analgesic effect, and can impact favorably on microcirculation and cartilage regeneration processes [3,10].
In theory, alone, therefore, these isolated or interactive biological effects can be expected to result in reductions in clinical pain levels, while aiding tissue repair, enhancing the resolution of inflammation and swelling, and promoting collagen synthesis and/or enhanced chondrocyte activity. Furthermore, pain relief may occur as result of direct stimulation of peripheral nerves, as well as an increase in serotonin metabolism, the activation of endogenous opioid receptors [11], or a decrease in the amplitude of electrically evoked potentials. Pain relief following laser therapy may also be expected consequent to any enhanced neural repair, a reduction in prostaglandin synthesis, an improvement of local circulation and bone healing effects [12].
To examine the current status of this form of therapy, articles documenting studies of patient outcomes following either continuous or pulsed low level laser treatment of an osteoarthritic joint, especially those published after 2015 were examined. This was to ascertain if any conflicting data have been forthcoming following the very negative conclusion of Huang et al. in 2014 [13] concerning laser therapy and its clinical efficacy in osteoarthritis treatment that has clearly impacted the recommended use of this modality quite markedly, and has since been criticized.
Methods
To obtain the desired data, PUBMED, Web of Science, Scopus, and Academic Search Complete data bases 19802017 were employed. The key terms used were lasers and osteoarthritis, laser therapy and osteoarthritis. Available data were downloaded and examined if they met criteria-of being full length English language publications, and focused on some aspect of laser intervention in experimental models such as the rat, or rabbit, or clinical samples of osteoarthritis. All forms of laser and osteoarthritis were deemed acceptable, and most studies reviewed were controlled trials or prospective studies. Studies on laser surgery were excluded.
Results
In terms of the years of interest, PUBMED yielded- 77 articles that were related to osteoarthritis and lasers, regardless of year, when considering the years 1980-2017; there were 199 articles when the key words osteoarthritis and laser therapy were applied for the same time period, [99 were related to low level laser therapy; 9 were specifically related to high intensity laser therapy]. Web of Science combined data bases housed 1067 articles pertaining to osteoarthritis and lasers as of October 25, 2017, and 476 articles listed under the terms osteoarthritis and laser therapy. Scopus lists 734 articles using the terms osteoarthritis and lasers, and 321 with the terms osteoarthritis and laser therapy.
These data had to be reviewed carefully to examine if they did indeed focus on the topic at hand, and those that were deemed suitably related were categorized as preclinical laboratory studies that utilized experimental models or cellular oriented methods of varying substrates, and clinical studies, including studies of laser applications to the hand, knee, hip, spine, and temporomandibular joints affected by osteoarthritis. The article presented here does not however discriminate the types of laser used in available studies, and does not examine the use of laser surgery. These include low power helium neon laser, infrared laser, pulsed Nd YAG laser, carbon dioxide lasers, Holmium: YAG lasers and Gallium-Arsenide lasers.
Studies that were deemed relevant were those that examined the outcomes of any form of laser intervention in the context of osteoarthritis or an acceptable animal model of this disease, especially those from 2015-2017. Clinical studies reviewed in prior meta-analyses were not comprehensively reviewed or included, along with conference reports and non-peer reviewed data. Outcomes examined were unrestricted, and included pain, inflammation, and function. Given the challenges of conducting meta-analyses in this realm, only a narrative overview of the prevailing trends in this area was undertaken.
Laboratory Study Finding
Although animal models of osteoarthritis may be suspect, and most cannot be confirmed as mirroring the actual in vivo osteoarthritis disease process at all successfully, several have shown interesting effects on pain and inflammation, key problems in the clinical context of osteoarthritis. While preclinical study results can vary dependent on the dosages of laser applied [14,15], or dosage combinations [16], Wang et al. [17] found applications of low-level laser of at least six weeks duration applied to a rabbit osteoarthritis model to positively influence pain and inflammation. In another study, Milares et al. [18] who conducted a multi-group comparison study of different experimental model rats subjected to an aquatic and low-level laser therapy, this group also showed laser therapy to be efficacious both as regards joint degenerative modifications as well as inflammatory mediators. After dividing 40 rats into four groups, a knee osteoarthritis and no treatment group; an osteoarthritis plus exercise group; an osteoarthritis plus low- level laser group; and osteoarthritis plus both interventions, laser therapy was performed at three points of contact on either side of the knee four weeks after surgery, for a period of eight weeks, three times a week. Results showed both the exercise and laser treated groups had better tissue organization, and less structural damage. The exercise and the laser-exercise combinations showed reduced expression of inflammatory markers, as well as a statistically significant lower matrix metalloprotease-13 inflammatory marker level. Assis et al. [19] too found that low-level laser therapy impacted the degenerative process in the rat model of knee osteoarthritis. The results were comparable to those attained by exercise or a combination of exercise and laser.
In another study, De Oliviera et al. [20] similarly examined the effects of photobiomodulation therapy on inflammation and pain using rats subjected to hyperalgesia who were divided randomly into three groups-a control group, an osteoarthritis group and an osteoarthritis and laser group. The laser therapy used a wavelength of 808nm, an power output of 50mW, an energy level for each point of 4 Joules. Post hoc comparisons were made between exposures lasting 6, 24, and 48h within each group, and between the control, injury, and laser groups. Findings showed, the hyperalgesia, which was present at 6, 24, and 48h after the injury was reduced after the application. As well, the application promoted cytokine attenuation and bradykin in receptor (B1 and B2) changes in the experimental period. The authors concluded that photo bio-modulation therapy promoted the reduction of proinflammatory cytokines, and reduced the gene and protein expression of the bradykinin receptors B1 and B2, as well increasing the stimulus response threshold to pressure in their experimental model of acute osteoarthritis.
Micheli et al. [21] who evaluated the pain relieving possibilities of photobiomodulation therapy in a rat model by testing two near infrared (NIR) laser systems, with differing power outputs, laser therapy found the intervention provided immediate relief of chronic articular or neuropathic pain. In this study, some rats were subjected to intra-articular injection of sodium monoiodoacetate and complete Freund's adjuvant, while others underwent compressive neuropathy by means of chronically injuring and constricting the sciatic nerve. In both models, NIR laser (MLS-Mphi, ASA S.r.l., Vicenza, Italy) was started 14 days after injury, and applied once daily on 13 occasions. In the injection treated model, the authors found an anti-hyperalgesic effect of laser that began 5 min after treatment and vanished after 60min. The subsequent applications produced like results. In the chronic sciatic nerve crush model, laser efficacy started 5 min after treatment and disappeared after 180 min. In rats that underwent crush injury, two additional treatment protocols with different power outputs were also tested using a new experimental device called Multiwave Locked System laser. Both protocols reduced mechanical hyperalgesia and hindlimb weight bearing alterations for up to 60 min after treatment with a higher efficacy recorded for the animals treated using the higher power output. Results supported those of Alves et al. [11] and Carlos et al. [22] who found near infrared light applications reduced knee inflammation significantly in a rat model of osteoarthritis.
Although not all studies show favorable effects [23,24], the conclusion reached by Pfander et al. [25] and Bayat et al. [26] seems justified. Namely, that laser applications can have modifiable effects on experimental simulations of osteoarthritis, including reductions in the extent of articular cartilage degeneration [27], and improvements in cartilage integrity [27]. According to Tomazini et al. [28] who studied a papain induced rat model of osteoarthritis, photobiomodulation or laser therapy was observed to be more effective in allaying the disease progression than exercise or non steroidal anti inflammatory drugs, and effectively improved the inflammatory conditions observed in osteoarthritis. Other salient findings from controlled laboratory studies are shown in Table 1.
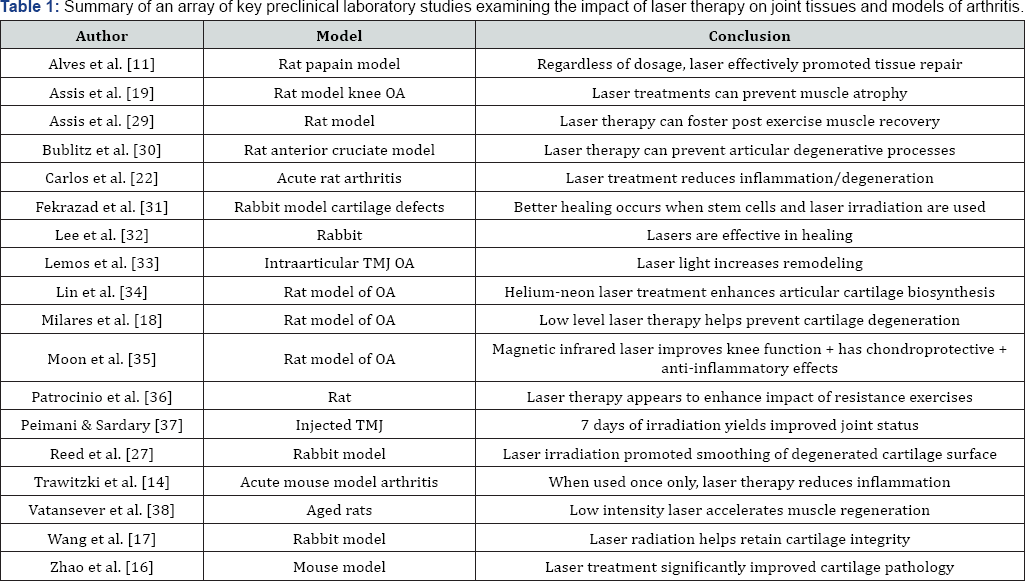
Abbreviations: OA= Osteoarthritis; TMJ= Temporomandibular joint Contemporary Clinical Findings
Contemporary Clinical Findings
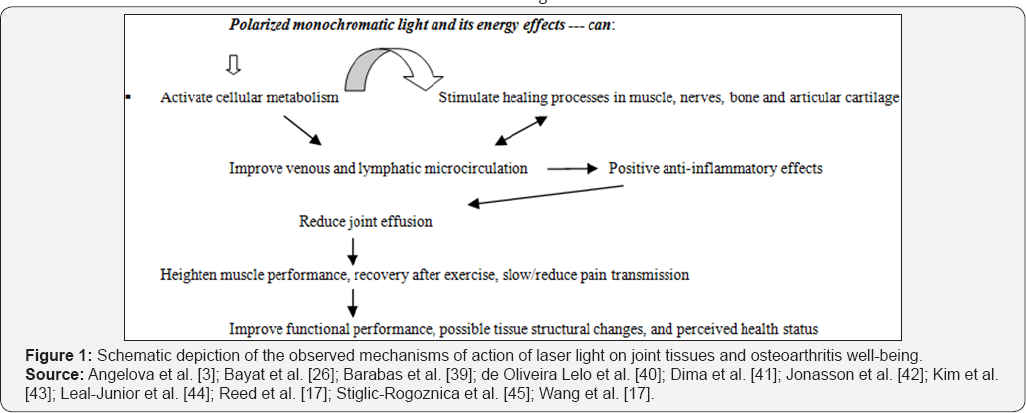
Figure 1 In addition to several very positive study outcomes reported over the past 25 years, such as that by Tam [46], where patients suffering from osteoarthritis and other related conditions improved substantively, often postponing the need for surgery, there are clearly several current randomized placebo controlled clinical trials and others that have examined the efficacy of laser intervention among various osteoarthritis samples with favorable results. These generally favorable outcomes tend to support several early studies reported by Marks [12], plus the more recent observations of Nakamura et al. [47] who subjected 35 outpatients with pain attributable to osteoarthritis to low level laser therapy and found the therapy reduced the chronic pain experience quite considerably over the time frame of the study, as did da Rosa et al. [48] for 96 knee osteoarthritis cases. A similar observation by Soleimanpour et al. [49] in a prospective descriptive study confirmed low level laser therapy yielded appreciable pain improvements in 18 cases with osteoarthritis of the knee, as did Yurtkuran et al. [50] in a double blinded randomized controlled study. Noticeable improvements in osteoarthritis of the cervical spine after two laser applications as detailed by Monteforte et al. [51] further supports the view that laser radiation therapy can effectively reduce osteoarthritis pain, immediately after treatment and for a prolonged period. Baltzer et al. [52] also found low level laser safe, and efficacious for treating Bouchard's and Heberden's osteoarthritis of the hand even after as little as five treatments. As well, the benefits in pain and swelling and increased range of motion lasted for eight weeks.
In another more recent controlled study, Helianthi et al. [53] found similar positive results in pain relief after laser acupuncture was applied to geriatric knee osteoarthritis cases. This group randomized 62 patients into an active laser versus a placebo laser group, and stimulated acupuncture points around the knee on 10 occasions, twice a week and evaluation followed after four treatment sessions, nine sessions, and for two weeks after the intervention ceased. Improvements occurred at all time points to a greater degree than in the control condition.
Low level laser applications also generated positive benefits on health status and muscle activation in elderly women with knee osteoarthritis. The results were reasonably comparable to those achieved with neuromuscular electrical stimulation. Instead of a control group, a control period was used, where no intervention was applied. This approach helped de Oliveira Melo et al. [40] to show that the post intervention effects reflected the interventions used. In another study, 100 elderly patients with bilateral tricompartmental knee osteoarthritis randomized to receive low-level laser and conventional therapy or conventional therapy were followed for six years. Results showed those who received the additional laser therapy did not require joint replacements, with one exception, whereas nine in the conventional treatment group required surgery [54].
S et al. [10] who attempted to examine both the analgesic as well as the biochemical effects of low level laser therapy for people with chronic osteoarthritis similarly showed the therapy was efficient in reducing pain as well as in improving cartilage thickness. In this study, 34 subjects were allocated to an active or placebo group. The active group received laser to 8 different points of the joint 3 days per week for 4 weeks at 1.5 J for 60 s each, and the skin contact method resulted in a total dose of 12 J of energy per session. The control group had minimal emission of energy applied to the same points. Outcomes assessed at 4 and 8 weeks after treatment showed improvements occurred at 4 and 8 weeks to a greater extent than those in the control group. The results at 4 and 8 weeks were derived from clinical tests and biochemical and radiographic assays. At baseline the groups were shown to be comparable, but after treatment the active group were experiencing significantly less pain and had improved cartilage indicators compared to controls [10]. In addition to its pain relieving benefits, which may be prolonged if laser is combined with strengthening exercises [55], laser therapy may promote spinal mobility in persons with lower back osteoarthritis [56], as well as jaw mobility in cases of temporomandibular osteoarthritis [57].
Other data show that laser therapy added to exercise training can produce a stronger positive effect on wellbeing than exercise alone, a finding not unlike that of Assis et al. [19,29] who examined an experimental model of knee osteoarthritis along with the effects of exercise training and laser therapy. This study finding by Youssef et al. [58] was especially intriguing because it was conducted on older subjects with knee osteoarthritis, often an age group resistant to exercise interventions, and positive outcomes. After allocating subjects to one of three groups, all groups exercised, but only two groups received active laser therapy. While all groups improved their pain scores, the group that received a laser dose of 6J/cm2 with a total dose of 48 did best. Additional benefits found by Assis et al. [19] were post stimulation benefits in muscle cross-sectional areas and less impact on the degenerative processes related to muscle atrophy in an experimental model. Another interesting observation made by Alfredo et al. [55] is that low-level laser applied before exercise can significantly reduce the level of analgesic consumption both after treatment for up to six months. These findings were comparable to those of Zou et al. [59] who found increases in synovial fluid ghrelin levels to increase following laser therapy applied to primary knee osteoarthritis patients, which was deemed a positive finding, thus supporting a strong possibility that laser therapy has significant treatment benefits when applied to an osteoarthritic joint as discussed by Marini et al. [57].
Further research has shown, positive bone healing benefits attributable to low level laser therapy in the case of maxillofacial bone defects, [60], while Alayat et al. [61] have shown high intensity laser therapy when combined with exercise and glucosamine therapy can be more potent than the control intervention and glucosamine and exercise alone for men with knee joint osteoarthritis. Angelova and Ilieva [3] similarly concluded high intensity laser therapy applied over seven treatments to persons with clinical and radiographic knee osteoarthritis reduces pain significantly and immediately and also improves function during walking tests when compared to sham laser. Similar findings were reported by Kim et al. [43] who applied high intensity laser three times per week for four weeks to adults with painful knee osteoarthritis. In cases where patients cannot take medication, results of de Carli et al. [62] suggest laser therapy can provide significant relief of osteoarthritic pain. See Table 2 for a summary of selected current placebo controlled studies and their outcomes.
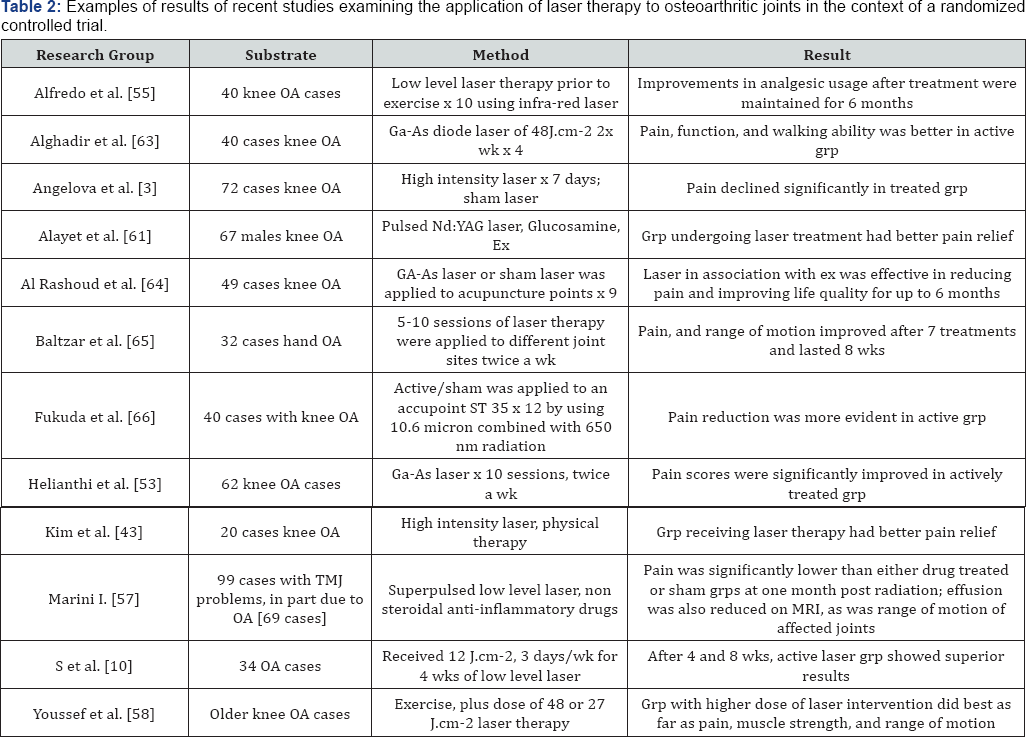
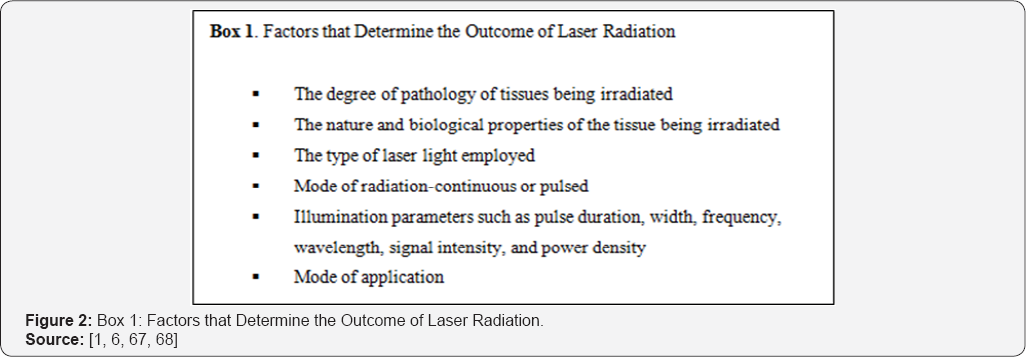
Factors affecting the outcome of laser therapy are highlighted in Figure 2. Differences in laser intensity are that high intensity laser increases the depth of penetration and can be used for shorter periods than low intensity laser to produce favorable anti-inflammatory, and pain effects [3]. Other factors are type of laser light used such as helium neon- or gallium arsenide. The biological effects of laser radiation include thermal, mechanical, electrical, photochemical, and biostimulatory or photochemical effects as outlined in Figure 1.
Discussion
Osteoarthritis, a prevalent disabling disease causes immense suffering. Since no known cure exists for osteoarthritis, a search for safe forms of therapy to alleviate the inevitable distress and disability that accompanies this progressive disease has prevailed for some time. The present analysis concerning the use of laser therapy for remediating osteoarthritis disability was undertaken due to the ambiguous findings of some prior systematic reviews on this topic, but not others. In this regard, in terms of favorable pain and healing outcomes post-laser irradiation, we did not come across many current equivocal findings for the years 2015-2017, when compared to previous recent work or that attempted almost 25 years ago [10,69]. That is, most current studies, regardless of whether they are experimental or clinical, appear to strengthen the case for applying laser therapy in efforts to ameliorate one or more symptoms of osteoarthritis independent of any associated placebo effect, or mode of application [70]. This was also the recent observation of Baltzer et al. [52] who conducted an analysis of low level laser therapy applications for rheumatic conditions, as well as Dima et al. [41] who focused on reviewing the chronic pain impact of low level laser therapeutic effects in cases of osteoarthritis. Indeed, regardless of whether the recent studies have been purely experimental or have been clinical, or whether high intensity or low intensity laser is used, a reader cannot fail to be impressed with the enormous potential for laser therapy to improve osteoarthritis disability rapidly, safely, and significantly. Moreover, in studies that used disparate treatment methods and outcome measures, and assessed the application of laser irradiation to osteoarthritis of differing joints and patients with disease durations with various methodologies, the therapy generally shows statistically significant beneficial results that exceed results of placebo applications or other therapies, and these results appear to be reasonably sustainable.
Importantly, not only do several current clinical studies demonstrate beneficial effects of laser for reducing pain [71], regardless of whether these are considered important or not to discuss in the context of updating osteoarthritis clinical literature [72] but several positive muscle-related structural and physiological benefits are demonstrated, and even patients with rheumatic diseases unresponsive to non steroid therapy have shown post laser therapy improvements [73]. As well, both low power laser irradiation therapy, or high power laser therapy applied to the tender areas or sites of nerves surrounding the painful osteoarthritic joint, or combined with ultrasound also appears to afford considerable pain relief [74], and consistent with laboratory evidence, laser therapy seems effective for repairing moderate cartilage lesions among young patients [75], and relieving post-operative orthopedic pain [76].
This series of positive findings are hence somewhat at odds with those of Huang et al. [13] who failed to support a role for low level laser applications for people with osteoarthritis based on a very limited number of selected studies that underwent a systematic review. However, among the multiple limiting issues observed in the design of the studies examined are sample size issues, blinding, contamination, and measurement issues. The aggregation of these diverse data sets, along with a failure to include studies that have shown benefits and others must also be questioned. Moreover, among selected studies, factors potentially affecting laser outcomes were discrepant modes of delivery, application durations, inclusion criteria, pre-treatment pain levels, disparate use of pain medications across groups, disparate outcome assessment tools and procedures, and extent of pathology, among other factors. Unfortunately, the fact remains that despite other reviews of this topic that are more positive, the meta-analysis conducted by Huang et al. [13] and research outlining negative results [77] has clearly influenced practitioner recommendations quite negatively. This is distressing to those who seek to help their osteoarthritis patients to cope more readily with their challenges because no viable form of conservative management that has so much potential to ameliorate multiple aspects of osteoarthritis concurrently and to do this safely has emerged in more than 20 years. Meanwhile, the numbers of affected persons suffering from osteoarthritis worldwide has grown exponentially.
However, as outlined by Ip [54] if we consider the very noteworthy positive findings of late that do prevail in both the experimental and clinical realms, along with those that have been conducted in the past [46,78], plus laser therapy benefits that have no side-effect and that extend to persons with pharmacologically resistant knee osteoarthritis pain [79], the potential for laser therapy to alleviate osteoarthritis suffering is potentially quite vast. As argued by Cotler et al. [78], with over 40 years of research in this realm that have produced an array of positive outcomes, its acceptance as a positive alternative or stand alone clinical treatment approach for selected osteoarthritis symptoms and disease manifestations cannot be easily overlooked or ignored. As observed by Tam almost two decades ago [46], and reiterated by Cotler et al. [78], and Hamblin [80], a strong basic foundation of evidence supports a role for laser therapy in efforts to relieve pain, as well as to promote healing processes. It also has beneficial muscle effects, can impact favorably on inflammation [80], and can heighten the impact of exercise therapy significantly [81].
Indeed, even though osteoarthritis is considered progressive and irreversible, Ip [54] found lower joint replacement rates in elderly subjects with osteoarthritis exposed to laser therapy, a very resounding finding with enormous potential positive implications. Ip [54] also highlighted the distinctive biophysical and cellular benefits of laser therapy applications to affected joint tissues that might be harnessed to reduce or reverse joint damage, in contrast to standard conservative approaches that do not impact physiological processes specifically in all cases. It is also a safe modality with proven anti-inflammatory and pain- relieving effects [41,82], and its simultaneous action of pain and function along with an apparent lack of significant usage contra-indications if applied at an extremely low dose [67]. With an impact superior to exercise alone [83], an ability to improve muscle performance and accelerate recovery when applied prior to exercise [44], a positive effect when combined with exercises [19,83], favorable post radiation soft tissue ultrasound outcomes [51], and its possible cartilage regenerative properties [75], the role of laser applications in the armamentarium to counter osteoarthritis disability clearly warrants more attention, even if placebo laser seems to yield some beneficial effects as demonstrated by Alghadir et al. [63].
High intensity laser, in particular seems very promising, with superior benefits to those achieved with low level laser therapy [83], even if this line of research is still in its infancy. Other potential laser benefits include an improved ability to carry out activities of daily living and a decline in the subjective pain experience [43]. Further careful manipulation of laser light dosages, modes of application, and application duration that are designed to maximize the ability of different laser signals to influence neural and structural entities selectively, may yet yield concurrent improvements in biomechanical functioning, joint stability, and bone healing, as well as inflammation in the osteoarthritis disease process [50]. The use of more objective clinically relevant biomarkers and outcome measures that are optimally applied may also reveal highly beneficial outcomes or responses that have not been well highlighted with subjective outcome measures, while helping to improve our understanding of the mechanisms underlying the observed post laser irradiation improvements in osteoarthritic pain and function [84]. As well, employing a true untreated control group, rather than laser placebos, along with more equitable, rather than disparate intergroup attention effects [63,74,83,85], plus differing standard physical therapy co intervention protocols and others may help to unmask the true effects of laser therapy as a unique standalone safe and effective modality for treating osteoarthritis [83,86]. In addition, careful sampling, instituting a washout period of at least two weeks prior to treatment session one, such as medications and physical therapy, controlling for activity levels between treatments, and non-confounding intervention approaches are strongly indicated to establish the true efficacy of the intervention.
In this regard, Alfredo et al. [83] specifically advocate the use of more histologically-oriented long-term studies in efforts to delineate the extent of any clinically relevant post-irradiation changes in cartilage thickness and morphology, or other cellular effects that may separate sham and actively treated groups, which seems a reasonably salient suggestion. Examining the reasons for the failure of certain laser applications to achieve clinical significance despite the application of salient biochemical and biomechanical tests may also prove highly revealing. These may include, but are not limited to the application of poorly designed studies, heterogeneity in trial design [44], widely diverse samples and outcome measures, and prevailing pathologies, unknown effects of comorbid diseases, and the inadvertent inclusion of light-emitting placebo lasers. Others are ineffectual treatment dosages or wave forms, light sources, and timing that can reduce treatment effectiveness, or produce a negative result [6], differences in the devices and/or laser type used [49], lack of knowledge concerning the definitive dosage required to maximize benefits [49], and/or the possibility of spontaneous symptom resolution, among other factors.
While future studies focusing on these possible pitfalls are desirable [49], in the interim, it can be accepted that contrary to the risks inherent in pharmaceutical drugs as well as some forms of injection [5], adverse effects are not prevalent or evident among the laser intervention studies reviewed, regardless of whether low or high power laser devices are used. Further, although a theoretical understanding of the mechanism of action of a modality is unnecessary to establish benefit [83], there is a reasonable evidence base to support underlying mechanisms for pain relief and tissue repair in laser-irradiated osteoarthritic joints [81,88], such as a reduction of tissue inflammation and vasodilation [49]. Studies in analogous pain syndromes such as myofascial pain syndrome and lateral epicondylitis that reveal positive pain, function, strength and life quality effects post laser irradiation that are sustained in the long term [87-93], clearly add to the value of this treatment form and its potential.
Thus, while cognizant of the fact negative studies may not be published, we concur with Strausholm et al. [94] that the conclusion reached by Huang et al. [13] must be questioned in light of the number of positive trials that have emerged in this realm to date, as was a similar Cochrane review that was found neither robust nor valid [80]. Moreover, as Balzer et al. [52] have recently argued, sufficient evidence not only supports the use of laser therapy in a preventive capacity, but as a modality that can potentially enhance muscle strength training effects, accelerate muscle regeneration, and can produce results comparable or superior to exercise alone, all of which would be highly advantageous for pain reduction in those unable to exercise [95]. Laser therapy also safely reduces pain at rest and during movement [78], improves function in cervical osteoarthritis [96] and walking ability in cases with chronic knee osteoarthritis [63], as well as life quality over an extended period [64]. Unlike other areas of research in this field, these favorable clinical outcomes and their purported mechanisms of action are quite well supported and highlighted in a broad array of preclinical studies, regardless of application mode and duration or substrate.
Concluding Remarks
As proposed by Zharova et al. [97], it is hard to dispute the potential of laser therapy, which can be integrated into nervous and joint tissues, as an efficacious, non-invasive, safe and cost- efficient means to treat and prevent osteoarthritis-associated problems in selected cases, even if this does not apply to all cases.
However, to extend our knowledge about this promising modality, more effort by orthopedic researchers and others to examine the impact of laser therapy of different parameters for treating a variety of joints at differing disease stages, along with the use of biomechanical, radiological, and salient biochemical outcome assessment tools is strongly indicated as discussed by Momenzadeh [98]. The role of laser therapy in averting or delaying joint surgery or fostering cartilage repair or both should also be intensely explored as well. Whether laser therapy improves surgical outcomes significantly, a very poorly researched area, can also be recommended.
Ideally, to overcome the lack of consensus concerning laser irradiation and its application for the treatment of osteoarthritic joints, well organized replicate studies with identical treatment protocols conducted on groups of patients with differing prognostic characteristics, using consistent outcome measurement approaches, are especially advocated. To eliminate the possibility of evoking positive treatment effects as a result of direct cutaneous stimulation, or a human presence, a control group that receives absolutely no direct intervention should be studied. Laser output(s) should also be carefully chosen and calibrated before treatments or placebo applications are administered, and potential effects of prior or concurrent therapies should be controlled for, even if this does not necessarily occur in the clinical setting.
Efforts to ensure treatment uniformity over time, as far as treatment sites and methodology goes, as well as efforts to minimize reflection and maximize penetration of the laser beam using validated laser dosages, skin sites chosen based on MRI or ultrasound images, and verified acupuncture sites [68], and to equalize attention, will be helpful. Blinded patients and interventionists, serial baseline measures in advance of treatment applications to determine the standard error of the outcome measures used, as advocated by Domholdt [99], along with sufficient subjects assessed periodically over an extended time frame (at least six months) may help to resolve the question of whether significant laser associated improvements occur, and whether these occur immediately or as a result of latent treatment effects, or both.
Finally, utilizing reliable and valid prognostic indicators and outcome measures sensitive to anticipated physiological changes, plus efforts to carry out comparative studies of different forms of laser, at different joint sites and for different disease stages and features, on more diverse samples, is strongly advocated.
In the interim, and in accord with Chung et al. [6] it is believed the number of negative laser reports is more likely than not to decline as more knowledge about the laser parameters unfold. Gray et al. [100] further hypothesize that 'energetic' therapies, including light based treatments, will continue to be used to affect growth, differentiation and proliferation of bone and nerve, as well as for promoting healing benefits in conditions such as osteoarthritis. The synergistic effects of laser with other modalities can also be expected to broaden the scope of treatment possibilities that may have additive long-lasting temporal effects in selected cases of osteoarthritis, and should be explored and harnessed accordingly [40,44,74,81]. In addition, as outlined by Baratto et al. [67], the promising application of ultralow level laser therapy should be explored for countering osteoarthritis pathology. Another is whether laser therapy can activate endogenous opioid receptors or distant neural structures that can influence immune function and central sensitization processes favorably, which would have immense treatment implications, especially in cases that cannot undergo surgery or use anti-inflammatory drugs and others [100].
References
- Pinals RS (1996) Mechanisms of joint destruction, pain and disability in osteoarthritis. Drugs 52(3): 14-20.
- Martel-Pelletier J, Barr AJ, Cicuttini FM, Conaghan PG, Cooper C, et al. (2016) Osteoarthritis. Nat Rev Dis Primers 13(2): 16072.
- Angelova A, Ilieva EM (2016) Effectiveness of high intensity laser therapy for reduction of pain in knee osteoarthritis. Pain Res Manag 2016: 9163618.
- Threlkeld JA, Currier DP (1988) Osteoarthritis: effects on synovial joint tissues. Physical Ther 68(3): 364-370.
- Sack KE (1995) Osteoarthritis. A continuing challenge. West J Med 163(6): 579-586.
- Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, et al. (2012) The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 40(2): 516-533.
- Passarella S, Casamassima E, Molinari S, Pastore D, Quagliariello E, et al. (1984) Increase of proton electrochemical potential and ATP synthesis in rat liver mitochondria irradiated in vitro by helium-neon laser. FEBS Letters 175(1): 95-99.
- Mester E, Mester AF, Mester A (1988) The biomedical effects of laser application. Lasers Surg Med 5(1): 31-39.
- Herman JH, Khosla RC (1988) In vitro effects of Nd:YAG laser radiation on cartilage metabolism. J Rheumatol 15(12): 1818-1826.
- S GN, Kamal W, George J, Manssor E (2017) Radiological and biochemical effects (CTX-II, MMP-3, 8, and 13) of low-level laser therapy (LLLT) in chronic osteoarthritis in Al-Kharj, Saudi Arabia. Lasers Med Sci 32(2): 297-303.
- Alves AC, Vieira R, Leal-Junior E, dos Santos S, Ligeiro AP, et al. (2013) Effect of low-level laser therapy on the expression of inflammatory mediators and on neutrophils and macrophages in acute joint inflammation. Arthritis Res Ther 15(5): R116.
- Marks R, de Palma F (1999) Clinical efficacy of low power laser therapy in osteoarthritis. Physiother Res Int 4(2): 141-157.
- Huang Z, Chen J, Ma J, Shen B, Pei F, et al. (2015) Effectiveness of low- level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 23(9): 1437-1444.
- Trawitzki BF, Lilge L, de Figueiredo FAT, Macedo AP, Issa JPM (2017) Low-intensity laser therapy efficacy evaluation in mice subjected to acute arthritis condition. J Photochem Photobiol B 174: 126-132.
- Issa JPM, Trawitzki BF, Ervolino E, Macedo AP, Lilge L (2017) Low- intensity laser therapy efficacy evaluation in FVB mice subjected to acute and chronic arthritis. Lasers Med Sci 32(6): 1269-1277.
- Zhao L, Shen XY, Cao YL, Wang LZ, Deng HP, et al. (2011) Effects of laser irradiation on arthritic histopathology and heat shock protein 70 expression in C57 black mice with osteoarthritis. Zhong Xi Yi Jie He Xue Bao 9(7): 761-767.
- Wang P, Liu C, Yang X, Zhou Y, Wei X, et al. (2014) Effects of low-level laser therapy on joint pain, synovitis, anabolic, and catabolic factors in a progressive osteoarthritis rabbit model. Lasers Med Sci 29: 18751885.
- Milares LP, Assis L, Siqueira A, Claudino V, Domingos H, et al. (2016) Effectiveness of an aquatic exercise program and low-level laser therapy on articular cartilage in an experimental model of osteoarthritis in rats. Connect Tissue Res 57(5): 398-407.
- Assis L, Almeida T, Milares LP, dos Passos N, Araujo B, et al. (2015) Musculoskeletal atrophy in an experimental model of knee osteoarthritis: the effects of exercise training and low-level laser therapy. Am J Phys Med Rehabil 94(5): 609-616.
- de Oliveira VL, Silva JA, Serra AJ, Pallotta RC, da Silva EA, et al. (2017) Photobiomodulation therapy in the modulation of inflammatory mediators and bradykinin receptors in an experimental model of acute osteoarthritis. Lasers Med Sci 32(1): 87-94.
- Micheli L, Di Cesare Mannelli L, Lucarini E, Cialdai F, Vignali L, et al. (2017) Photobiomodulation therapy by NIR laser in persistent pain: an analytical study in the rat. Lasers Med Sci 32(8): 1835-1846.
- Carlos FP, de Paula Alves da Silva M, de Lemos Vasconcelos Silva Melo E, Costa MS, Zamuner SR (2014) Protective effect of low-level laser therapy (LLLT) on acute zymosan-induced arthritis. Lasers Med Sci 29(2): 757-763.
- Comunian CR, Custodio ALN, de Oliveira LJ, Dutra CEA, D'almeida Ferreira Neto M, et al. (2017) Photobiomodulation with LED and laser in repair of mandibular socket rabbit: clinical evaluation, histological, and histomorphometric. Oral Maxillofac Surg 21(2): 201-206.
- Madani AS, Ahrari F, Nasiri F, Abtahi M, Tuner J (2014) Low-level laser therapy for management of TMJ osteoarthritis. Cranio 32(1): 38-44.
- Pfander D, Jorgensen B, Rohde E, Bindig U, Muller G, et al. (2006) The influence of laser irradiation of low-power density on an experimental cartilage damage in rabbit knee-joints: an in vivo investigation considering macroscopic, histological and immuno histochemical changes. Biomed Tech (Berl) 51(3): 131-138.
- Bayat M, Virdi A, Jalalifirouzkouhi R, Rezaei F (2017) Comparison of effects of LLLT and LIPUS on fracture healing in animal models and patients: a systematic review. Prog Biophys Mol Biol pii: S0079- 6107(17)30118-9.
- Reed SC, Jackson RW, Glossop N, Randle J (1994) An in vivo study of the effect of excimer laser irradiation on degenerate rabbit articular cartilage. Arthroscopy 10(1): 78-84.
- Tomazoni SS, Leal-Junior EC, Pallotta RC, Teixeira S, de Almeida P, et al. (2017) Effects of photobiomodulation therapy, pharmacological therapy, and physical exercise as single and/or combined treatment on the inflammatory response induced by experimental osteoarthritis. Lasers Med Sci 32(1): 101-108.
- Assis L, Milares LP, Almeida T, Tim C, Magri A, et al. (2016) Aerobic exercise training and low-level laser therapy modulate inflammatory response and degenerative process in an experimental model of knee osteoarthritis in rats. Osteoarthritis Cartilage 24(1): 169-177.
- Bublitz C, Medalha C, Oliveira P, Assis L, Milares LP, et al. (2014) Low- level laser therapy prevents degenerative morphological changes in an experimental model of anterior cruciate ligament transection in rats. Lasers Med Sci 29(5): 1669-1678.
- Fekrazad R, Eslaminejad MB, Shayan AM, Kalhori KA, Abbas FM, et al. (2016) Effects of photobiomodulation and mesenchymal stem cells on articular cartilage defects in a rabbit model. Photomed Laser Surg 34(11): 543-549.
- Lee JY, Lee SU, Lim T, Choi SH (2014) Healing effects and superoxide dismutase activity of diode/Ga-As lasers in a rabbit model of osteoarthritis. In Vivo 28(6): 1101-1106.
- Lemos GA, Rissi R, de Souza Pires IL, de Oliveira LP, de Aro AA, et al. (2016) Low-level laser therapy stimulates tissue repair and reduces the extracellular matrix degradation in rats with induced arthritis in the temporomandibular joint. Lasers Med Sci 31(6): 1051-1059.
- Lin YS, Huang MH, Chai CY (2006) Effects of helium-neon laser on the mucopolysaccharide induction in experimental osteoarthritic cartilage. Osteoarthritis Cartilage 14(4): 377-383.
- Moon CH, Kwon O, Woo CH, Ahn HD, Kwon YS, et al. (2014) Therapeutic effect of irradiation of magnetic infrared laser on osteoarthritis rat model. Photochem Photobiol 90(5): 1150-1159.
- Patrocinio T, Sardim AC, Assis L, Fernandes KR, Rodrigues N, et al. (2013) Effect of low-level laser therapy (808nm) in skeletal muscle after resistance exercise training in rats. Photomed Laser Surg 31(10): 492-498.
- Peimani A, Sardary F (2014) Effect of low-level laser on healing of temporomandibular joint osteoarthritis in rats. J Dent (Tehran) 11(3): 319-327.
- Vatansever F, Rodrigues NC, Assis LL, Peviani SS, Durigan JL, et al. (2012) Low intensity laser therapy accelerates muscle regeneration in aged rats. Photonics Lasers Med 1(4): 287-297.
- Barabas K, Bakos J, Zeitler Z, Balint G, Nagy E, et al. (2014) Effects of laser treatment on the expression of cytosolic proteins in the synovium of patients with osteoarthritis. Lasers Surg Med 46(8): 644-649.
- de Oliveira Melo M, Pompeo KD, Baroni BM, Vaz MA (2016) Effects of neuromuscular electrical stimulation and low-level laser therapy on neuromuscular parameters and health status in elderly women with knee osteoarthritis: a randomized trial. J Rehabil Med 48(3): 293-299.
- Dima R, Tieppo Francio V, Towery C, Davani S (2017) Review of literature on low-level laser therapy benefits for nonpharmacological pain control in chronic pain and osteoarthritis. Altern Ther Health Med pii: AT5647.
- Jonasson TH, Zancan R, de Oliveira Azevedo L, Fonseca AC, Silva MCD, et al. (2017) Effects of low-level laser therapy and platelet concentrate on bone repair: Histological, histomorphometric, immunohistochemical, and radiographic study. J Craniomaxillofac Surg 45(11): 1846-1853.
- Kim GJ, Choi J, Lee S, Jeon C, Lee K (2016) The effects of high intensity laser therapy on pain and function in patients with knee osteoarthritis. J Phys Ther Sci 28(11): 3197-3199.
- Leal-Junior EC, Vanin AA, Miranda EF, de Carvalho Pde T, Dal Corso S, et al. (2015) Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis. Lasers Med Sci 30(2): 925-939.
- Stiglic-Rogoznica N, Stamenkovic D, Frlan-Vrgoc L, Avancini-Dobrovic V, Vrbanic TS (2011) Analgesic effect of high intensity laser therapy in knee osteoarthritis. Coll Anthropol 35 Suppl 2:183-185.
- Tam G (1999) Low power laser therapy and analgesic action. J Clin Laser Med Surg 17: 29-33.
- Nakamura T, Ebihara S, Ohkuni I, Izukura H, Harada T, Ushigome, et al. (2014) Low level laser therapy for chronic knee joint pain patients. Laser Ther 23(4): 273-277.
- da Rosa AS, dos Santos AF, da Silva MM, Facco GG, Perreira DM, et al. (2012) Effects of low-level laser therapy at wavelengths of 660 and 808 nm in experimental model of osteoarthritis. Photochem Photobiol 88(1): 161-166.
- Soleimanpour H, Gahramani K, Taheri R, Golzari SE, Safari S, et al. (2014) The effect of low-level laser therapy on knee osteoarthritis: prospective, descriptive study. Lasers Med Sci 29(5): 1695-1700.
- Yurtkuran M, Alp A, Konur S, Ozfakir S, Bingol U (2007) Laser acupuncture in knee osteoarthritis: a double-blind, randomized controlled study. Photomed Laser Surg 25(1): 14-20.
- Monteforte P, Baratto L, Molfetta L, Rovetta G (2003) Low-power laser in osteoarthritis of the cervical spine. Int J Tissue React 25(4): 131136.
- Baltzer AW, Ostapczuk MS, Stosch D (2016) Positive effects of low level laser therapy (LLLT) on Bouchard's and Heberden's osteoarthritis. Lasers Surg Med 48(5): 498-504.
- Helianthi DR, Simadibrata C, Srilestari A, Wahyudi ER, Hidayat R (2016) Pain reduction after laser acupuncture treatment in geriatric patients with knee osteoarthritis: a randomized controlled trial. Acta Med Indones 48(2): 114-1121.
- Ip D (2015) Does addition of low-level laser therapy (LLLT) in conservative care of knee arthritis successfully postpone the need for joint replacement? Lasers Med Sci 30(9): 2335-2339.
- Alfredo PP, Bjordal JM, Junior WS, Martins RABL, Stausholm MB, et al. (2017) Long-term results of a randomized, controlled, doubleblind study of low-level laser therapy before exercises in knee osteoarthritis: laser and exercises in knee osteoarthritis. Clin Rehabil 269215517723162.
- Zdrodowska B, Leszczynska-Filus M, Leszczynski R, Biaszczyk J (2015) [Comparison of the effect of laser and magnetic therapy for pain level and the range of motion of the spine of people with osteoarthritis lower back]. Pol Merkur Lekarski 38(223): 26-31.
- Marini I, Gatto MR, Bonetti GA (2010) Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain 26(7): 611616.
- Youssef EF, Muaidi QI, Shanb AA (2016) Effect of laser therapy on chronic osteoarthritis of the knee in older subjects. J Lasers Med Sci 7(2): 112-119.
- Zou YC, Deng HY, Mao Z, Zhao C, Huang J, et al. (2017) Decreased synovial fluid ghrelin levels are linked with disease severity in primary knee osteoarthritis patients and are increased following laser therapy. Clin Chim Acta 470: 64-69.
- Santinoni CD, Oliveira HF, Batista VE, Lemos CA, Verri FR (2017) Influence of low-level laser therapy on the healing of human bone maxillofacial defects: a systematic review. J Photochem Photobiol B 169: 83-89.
- Alayat MS, Aly TH, Elsayed AE, Fadil AS (2017) Efficacy of pulsed Nd:YAG laser in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci 32(3): 503-511.
- de Carli ML, Guerra MB, Nunes TB, di Matteo RC, de Luca CE, et al. (2013) Piroxicam and laser phototherapy in the treatment of TMJ arthralgia: a double-blind randomised controlled trial. J Oral Rehabil 40(3): 171-178.
- Alghadir A, Omar MT, Al-Askar AB, Al-Muteri NK (2014) Effect of low-level laser therapy in patients with chronic knee osteoarthritis: a single-blinded randomized clinical study. Lasers Med Sci 29(2): 749755.
- Al Rashoud AS, Abboud RJ, Wang W, Wigderowitz C (2014) Efficacy of low-level laser therapy applied at acupuncture points in knee osteoarthritis: a randomized double-blind comparative trial. Physiotherapy 100(3): 242-248.
- Baltzer AWA, Stosch D, Seidel F, Ostapczuk MS (2017) [Low level laser therapy: a narrative literature review on the efficacy in the treatment of rheumatic orthopaedic conditions]. Z Rheumatol 76(9):806-812.
- Fukuda VO, Fukuda TY, Guimaraes M, Shiwa S, de Lima Bdel C, Martins, et al. (2015) Short-term efficacy of low-level laser therapy in patients with knee osteoarthritis: a randomized placebo-controlled, doubleblind clinical trial. Rev Bras Ortop 46(5): 526-533.
- Baratto L, Capra R, Farinelli M, Monteforte P, Morasso P, et al. (2000) A new type of very low-power modulated laser: soft-tissue changes induced in osteoarthritic patients revealed by sonography. Int J Clin Pharmacol Res 20(1-2): 13-16.
- Gworys K, Gasztych J, Puzder A, Gworys P, Kujawa J (2012) Influence of various laser therapy methods on knee joint pain and function in patients with knee osteoarthritis. Ortop Traumatol Rehabil 14(3): 269-277.
- Vangsness CT, Ghaderi B (1993) A literature review of lasers and articular cartilage. Orthopedics 16(5): 593-598.
- Ammar TA (2014) Monochromatic infrared photo energy versus low level laser therapy in patients with knee osteoarthritis. J Lasers Med Sci 5(4): 176-182.
- Kingsley JD, Demchak T, Mathis R (2014) Low-level laser therapy as a treatment for chronic pain. Front Physiol 5: 306.
- Bennell KL, Hall M, Hinman RS (2016) Osteoarthritis year in review 2015: rehabilitation and outcomes. Osteoarthritis cartilage 24(1): 5870.
- Fulga C, Fulga IG, Predescu M (1994) Clinical study of the effect of laser therapy in rheumatic degenerative diseases. Rom J Intern Med 32(3): 227-233.
- Paolillo AR, Paolillo FR, Joao JP, Joao HA, Bagnato VS (2015) Synergic effects of ultrasound and laser on the pain relief in women with hand osteoarthritis. Lasers Med Sci 30(1): 279-286.
- Zati A, Desando G, Cavallo C, Buda R, Giannini S, et al. (2012) Treatment of human cartilage defects by means of Nd:YAG laser therapy. J Biol Regul Homeost Agents 26(4): 701-711.
- Nesioonpour S, Mokmeli S, Vojdani S, Mohtadi A, Akhondzadeh R, et al. (2014) The effect of low-level laser on postoperative pain after tibial fracture surgery: a double-blind controlled randomized clinical trial. Anesth Pain Med 4(3):e17350.
- Tascioglu F, Armagan O, Tabak Y, Corapci I, Oner C (2004) Low power laser treatment in patients with knee osteoarthritis. Swiss Med Wkly 134(17-18): 254-258.
- Cotler HB, Chow RT, Hamblin MR, Carroll J (2015) The use of low level laser therapy (lllt) for musculoskeletal pain. MOJ Orthop Rheumatol 2(5): 00068.
- Mokmeli S, Attarian H, Hosseini M, et al. (2006) Conference: 6th International Congress of the World-Association-of-Laser-Therapy. Al Watban F, Rochkind S, Roumbas A (Eds.), Proceedings of the 6th International Congress of the World Association of Laser Therapy, Limassol, Cyprus, Oct 25-28, pp: 135-138.
- Hamblin M (2013) Can osteoarthritis be treated by light. Arthritis Res Ther 15(5): 120.
- Hamblin MR (2017) Mechanisms and applications of the antiinflammatory effects of photobiomodulation. AIMS Biophys 4(3): 337361.
- Rayegani SM, Raeissadat SA, Heidari S, Moradi-Joo M (2017) Safety and effectiveness of low-level laser therapy in patients with knee osteoarthritis: a systematic review and meta-analysis. J Lasers Med Sci 8(Suppl 1): S12-S19.
- Alfredo PP, Bjordal JM, Dreyer SH, Meneses SR, Zaguetti G, et al. (2012) Efficacy of low level laser therapy associated with exercises in knee osteoarthritis: a randomized double-blind study. Clin Rehabil 26(6): 523-533.
- Gur A, Cosut A, Sarac AJ, Cevik R, Nas K, et al. (2003) Efficacy of different therapy regimes of low-power laser in painful osteoarthritis of the knee: a double-blind and randomized-controlled trial. Lasers Surg Med 33(5): 330-338.
- Ferreira de Meneses SR, Hunter DJ, Young Docko E, Pasqual Marques A (2015) Effect of low-level laser therapy (904 nm) and static stretching in patients with knee osteoarthritis: a protocol of randomised controlled trial. BMC Musculoskelet Disord 16: 252.
- Ip D, Fu NY (2015) Can combined use of low-level lasers and hyaluronic acid injections prolong the longevity of degenerative knee joints? Clin Interv Aging 10: 1255-1258.
- Bertolucci LE, Grey T (1995) Clinical analysis of mid-laser versus placebo treatment of arthralgic TMJ degenerative joints. J Craniomandibular Practice 13(1): 26-29.
- de Vasconcellos LM, Barbara MA, Deco CP, Junqueira JC, do Prado RF, et al. (2014) Healing of normal and osteopenic bone with titanium implant and low-level laser therapy (GaAlAs): a histomorphometric study in rats. Lasers Med Sci 29(2): 575-580.
- Emanet SK, Altan LI, Yurtkuran M (2010) Investigation of the effect of GaAs laser therapy on lateral epicondylitis. Photomed Laser Surg 28(3): 397-403.
- Baxter GD, Alen JM, Bell AJ, Ravey J, Diamanthopoulos C (1991) Effect of laser (830 nm) upon conduction in the median nerve. American Society for Laser Medicine and Surgery Abstracts. Lasers in Surgery and Medicine 3: 79.
- Akkurt E, Kucuksen S, Yilmaz H, Parlak S, Salli A, et al. (2016) Long term effects of high intensity laser therapy in lateral epicondylitis patients. Lasers Med Sci 31(2): 249-253.
- Altan L, Bingol U, Aykaf M, Yurtkuran M (2005) Investigation of the effect of GaAs laser therapy on cervical myofascial pain syndrome. Rheumatol Int 25(1): 23-27.
- Dundar U, Turkmen U, Toktas H, Solak O, Ulasli AM (2015) Effect of high-intensity laser therapy in the management of myofascial pain syndrome of the trapezius: a double-blind, placebo-controlled study. Lasers Med Sci 30(1): 325-332.
- Stausholm MB, Bjordal JM, Lopes-Martins RAB, Joensen J (2017) Methodological flaws in meta-analysis of low-level laser therapy in knee osteoarthritis: a letter to the editor. Osteoarthritis Cartilage 25(4): e9-e10.
- Lumpkin JJ (2007) The effect of low level laser therapy and exercise on perceived pain and activities of daily living in low back pain patients. Dissertation. Murfreesboro, Tennessee, USA.
- Gur A, Cosut A, Sarac AJ, Cevik R, Nas K, et al. (2003) Efficacy of different therapy regimes of low-power laser in painful osteoarthritis of the knee: a double-blind and randomized-controlled trial. Lasers Surg Med 33(5): 330-338.
- Zharova TA, Ivannikov SV, Tonenkov AM, Stranadko EP, Semenova LA, et al. (2016) Gonarthritis photodynamic therapy with chlorin e6 derivatives. Photodiagnosis Photodyn Ther pp. 88-93.
- Momenzadeh S (2013) Low level laser therapy for painful joints. J Lasers Med Sci 4(2): 67-69.
- Domholdt E (1993) Experimental research. In: Domholdt E (Ed.), Physical Therapy Research: Principles and Applications. WB Saunders, Philadelphia, USA, pp. 51-73.
- Gray MG, Lackey BR, Patrick EF, Gray SL, Hurley SG (2016) Multiple integrated complementary healing approaches: energetics & light for bone. Med Hypotheses 86: 18-29.






























