Is it too late to Fix Now? Management of PCL Avulsion Injuries with Late Presentation/Non-Union
Banerjee S1*, Sharma PK2*, Singh K1 and Elhence A1
1Department of Orthopaedics, All India Institute of Medical Sciences, India
2Department of Pharmacology, All India Institute of Medical Sciences, India
Submission: July 19, 2017; Published: July 31, 2017
*Corresponding author: Pramod Kumar Sharma, Sumit Banerjee, Department of Pharmacology and Orthopaedics, All India Institute of Medical Sciences, Jodhpur, India, Tel: 9910895314, 8003996894, Email: banerjees@aiimsjodhpur.edu.in, pramod309@gmail.com
How to cite this article: Banerjee S, Sharma PK, Singh K, Elhence A. Is it too late to Fix Now? Management of PCL Avulsion Injuries with Late Presentation/Non-Union. Nov Tech Arthritis Bone Res. 2017; 1(4) : 555570 DOI: 10.19080/NTAB.2017.01.555570
Abstract
Purpose: Delayed presentation of PCL avulsion injuries can pose a therapeutic problem. Through this study we aim to share our experience in managing PCL avulsion fractures presenting late to the orthopaedic department. The study also aims to analyze the published literature for such cases.
Methods: In this study 4 cases with PCL avulsion injuries were operated upon after a mean 14.25 months (3-36 months] of injury. They underwent open reduction and internal fixation (ORIF] with cannulated screws using the Burk and Schaeffer approach to expose the fracture.The patients were assessed for union and pain using VAS and functional outcome using Lysholm score. A literature search was conducted to search for published literature on the topic and results discussed.
Results: All patients achieved bony union and had improved pain scores. There was vast improvement in functional outcome scores as assessed by Lysholm score. Only 3 reported studies were found in literature search on the subject; all these studies have advocated ORIF with cannulated screws for delayed PCL avulsion fractures and reported favourable outcomes.
Conclusions: ORIF with cannulated screws for PCL avulsion injuries presenting late/ nonunion provides satisfactory results and is a reliable and advisable management strategy for these patients.
Keywords: PCL avulsion; Duration from injury; ORIF
Introduction
Posterior Cruciate ligament (PCL) injuries account for nearly 20% of knee injuries [1]. PCL avulsion fractures from its tibial insertion site are uncommon & are often missed [2]. However with increased patient awareness and improved diagnostic procedures; the number of PCL avulsion injuries presenting to an orthopaedic clinic have increased [3]. The role of PCL in stabilization of knee cannot be overemphasized [4,5]. It is the major stabilizer of the knee joint posteriorly [6].
The mechanism of injury is usually vehicular accidents specially dashboard injury with a flexed knee 1. In sports related injuries acute forced hyperextension of knee may lead to such fractures [7]. Patients presenting early, present with pain, swelling & deep tenderness in popliteal fossa & have a positive posterior drawer test. Untreated or missed PCL avulsion fractures usually present with anterior knee pain aggravated by activity, difficulty climbing stairs, knee swelling and occasionally instability [8].
While both conservative and operative management for PCL injuries have their proponents [9-11]; the common area of consensus is PCL avulsion fractures where early surgical fixation has been recommended [12]. The major knowledge gap is regarding surgical fixation of PCL avulsion fractures with delayed presentation/non union. Search of literature in Pubmed and Google Scholar, on surgical fixation in chronic/missed PCL avulsion fractures injuries yields only three articles further asserting the fact that there hasn’t been much documentation regarding such cases. It also points towards the lack of any consensus in management for the same. The purpose of this article is to review the literature and share our experience in management of these injuries.
Material and Methods
Literature search: A comprehensive and structured search was conducted for published literature assessing surgical management of PCL avulsion fractures with late/ delayed presentation/ missed diagnosis/ delayed/ non union. The search was performed electronically on the following databases- MEDLINE (PubMed) (June 2017), EMBASE (2017 week 26), Google Scholar. Data base specific abbreviations, limiters and Boolean operators were used to combine the specific search terms to yield the results. No language restrictions were applied for the search process. Only studies with human subjects were included.
The search yielded only 3 articles about delayed surgical management of PCL avulsion fractures. First one dated back to 1979 when Take hilko Torshu published indications and results of delayed surgical repair of these fractures in CORR [13]. A case report was published in 2006 by Jung et al. [14]. More recently a study was published by Rohit Singla et al in Journal of Orthopaedic surgery in [15].
Case series
Between May 2016 & Feb 2017 3 men & 1 women aged 25 to 36 years (mean 28.5 years) presented to the orthopedics outpatient department with complaints of knee pain, and variable posterior knee instability with symptoms lasting for more than two months and the initial injury older than 2 months. The mechanism of injury was RTA in 3 (75%) and fall from height in 1 case. They presented to the clinic after a mean delay of 14.25 (range, 3-36) months. In 2 cases the diagnosis was missed at the time of initial injury and in the other 2 a conservative approach was used for the management of these injuries [16].
Clinical examination comprised of Lachman test, anterior & posterior drawer test, valgus & varus stress testing at 00 & 300, dial test, active quadriceps test and pivot shift test. Standard orthogonal radiographs anteroposterior & lateral at 300 knee flexion were taken along with MR imaging.
Pre‐operative physiotherapy was commenced in all the four cases. Pre-operative Lysholm scores were calculated at the time of counselling and informed consent was taken for surgery.
Operative technique
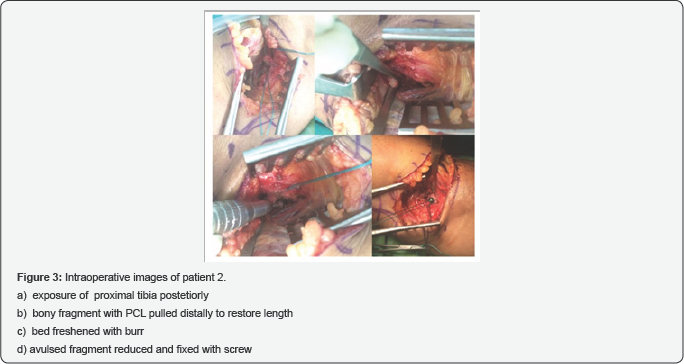
All the patients underwent surgery in regional anesthesia (spinal). The patient was put in prone position and apneumatic tourniquet was applied to the thigh to minimize bleeding into the operating field. The fracture was approached using an "L" shaped incision (Burke and Schaeffer approach) [17] with the vertical arm medially and distally and the horizontal arm of the incision marked parallel and slightly proximal to the joint line, marked using the fluoroscopy. The interval between the medial border of medial gastronomies and semi membrane osus muscle was developed. After dissecting the medial border of the medial gastrocnemius, the muscle was retracted laterally to expose the posterior joint capsule. The fracture fragment and bed was universally found to be sclerosed and was freshened using an electrical burr until cancellous bone was evident. The PCL tendon was freed from the fibrous tissue and through an ethibond suture was pulled distally to restore length and tension in the ligament. The fracture was then reduced; reduction checked under C-arm and was fixed using partially threaded cannulated cancellous screws (4mm dia.) with washer as distal as possible in PCL fossa. One of the cases (case 3) had a very large fragment and required 2 screws for adequate fixation. The wound was closed after deflating tourniquet and obtaining hemostasis.
Postoperatively the knee was immobilized in 300 flexion in a knee brace for 2 weeks and encouraged to do SLR and ankle exercises. A check dressing was done at 48 hours and IV antibiotics were stopped if the dressing was healthy. At 2 weeks, the slab and sutures were removed. The patients were then placed in a ROM brace with restriction of extension to 30 degrees. They were allowed to touch mobilization with crutches along with isotonic quadriceps and hamstring exercises. Full weight bearing was allowed after 8-10 weeks. Union was defined as absence of pain, stable knee, full weight bearing walking without any support and radiological union. The patients were followed up at 2,6 weeks and then at 3,6 and 12 months. Standard AP and Lateral Knee X-rays were ordered at 6 weeks, 3 months and 6 months post-operatively.
Patient satisfaction was assessed using Visual Analogue scale (VAS) and Lysholm scores. Pre operative and post operative knee range of movement, Lysholm scores and VAS scores were recorded at the time of initial counselling and then at 3 and 6 months postoperatively. These scores were tabulated and compared.
Results
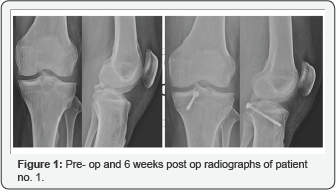
The mean follow-up period was 8(range, 4-12) months. All patients achieved union at mean 12(range, 10-14) weeks. VAS scores reduced from mean 6(range, 5-7) to mean 1(range, 0-2) at 6 weeks postoperatively. None of the patients required regular analgesia in the post operative period beyond the first week. The range of movement (ROM) improved from mean 96.60 to 113.30. Full extension was achieved in all patients while 1 patient had restriction of terminal flexion at 3 months post operatively. All which improved to no laxity in 3 cases and grade I laxity in 1 4 patients had grade III posterior drawer test pre-operatively case. There were no wound complications (Figure 1‐3).
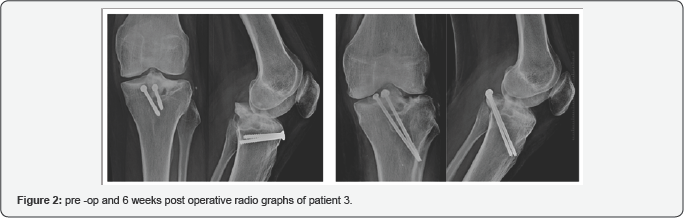
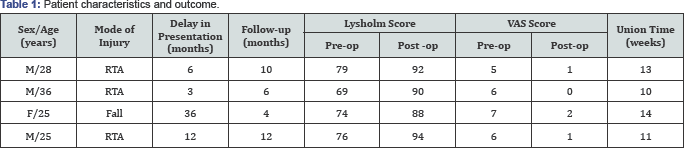
Lysholm scores preoperatively ranged from 69 to 79 (mean 74.5). This improved to a mean postoperative Lysholm score of 91(range 88‐94). All the patients were back to their pre‐injury level of activities after 6 months of surgery except one patient who is still to complete her 6 month follow-up Table 1.
Discussion
As is evident from the results of the literature search, there is a paucity of documented studies on delayed fixation/ management of non-union PCL avulsion fracture. Only 3 studies have been documented all of which are small case series/ case report. This can be attributed to the following factors.
Firstly the incidence of isolated PCL injuries is less as compared to ACL injuries and more specifically PCL avulsion injuries account for a small subset of PCL injuries [17,18]. This leads to a few studies being available about the prognosis and management of these injuries.
Secondly, the symptoms following PCL injuries are not as characteristic as following ACL injury. Posterior instability is not the major or common symptom instead patients have anterior knee pain, difficulty with stairs and pain on prolonged activities [19]. This often results in the patients presenting late / injuries being missed [20]
ORIF for Acute PCL avulsion fractures is generally advised and has been documented widely to be successful [21]. However there is no consensus on whether ORIF is advisable in delayed cases 15. The studies extracted from the literature search all commented towards this information gap.
However the literature available, albeit little showed that ORIF was performed for cases with delayed fixation/ non union. In our experience we manage PCL avulsion Injuries whether acute or delayed using ORIF with cannulated screws. Singla reported good union rates and acceptable functional outcome following ORIF for delayed PCL avulsion fractures. All but one of their patients achieved union. Jung et al too reported union in their case. In our series too all patients achieved union, indicating that delayed presentation doesn't impede the chances of union.
Singla et al. [15] used cancellous bone grafting, we didn't feel the need to do so as after freshening the bony bed/ fragment with a burr, healthy cancellous contact was achieved. We do however feel that using a high speed burr to remove the sclerotic bone is imperative to achieve a good cancellous surface and helpful in achieving union. One of our patients had residual posterior laxity on testing but no functional disability. Residual posterior laxity has been reported in studies following PCL avulsion fractures [15,22]. This has been attributed to ligament tear/ intra substance injury to the PCL. We too concur to the fact that in presence of actual ligament injury, a PCL reconstruction would be the advised treatment. We however didn’t find any intra substance injury/ partial tear of PCL in our cases. Posterior laxity also doesn’t correlate well with functional outcome as has been reported in literature [23]. We therefore believe that residual posterior laxity on testing; in absence of functional debility shouldn't be counted as a negative result of PCL Avulsion fixation.
Traditionally the direct posterior approach (Abbott and carpenter] has been described for PCL avulsion fixation. This approach through the popliteal fossa is quite close to the neuro vascular bundle and hence carries higher risk of neurovascular injury and also adds to operating time. We prefer the Modified L incision (Burk and Schaeffer) as it involves minimal dissection and avoids the neuro vascular bundle which is protected by the gastrocnemius muscle. This approach now seems to be the preferred method of choice for PCL avulsion fixations and has been reported in many studies [3,15,22].
We used the Lysholm score to assess the functional outcome in patients following surgery. This is in concurrence with other studies published on this injury. It is a very objective and useful score to assess knee function and has been validated in literature [24]. All our patients had improvement in their lysholm scores with a mean improvement of 16.5 (range 13-21) after surgery. This is similar to the study by Singla et al where thay reported improvement of Lysholm score from a mean of 82 to 92 postoperatively. We had some limitations to our study. Its low sample size ruled out any statistical analysis. The follow-up period is not long enough to evaluate the long term functional outcome.
Conclusion
PCL avulsion injuries are frequently missed or present late with non-union. They can cause considerable functional impairment in patients and warrant surgical management. Open Reduction and Internal Fixation with cannulated screws in cases of delayed PCL avulsion fixation yields good union rates and functional outcome and is a reliable option in these patients.
Conflict of Interest Statement
The authors certify that they have no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/ licensing arrangements, etc] that might pose a conflict of interest in connection with the submitted article.
References
- Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ (2003] Epidemiology of posterior cruciate ligament injuries. Archives of orthopaedic and trauma surgery 123(4): 186-191.
- Sergio PR, Martha MM (2007] surgical treatment of avulsion fractures of the knee PCL tibial insertion: experience with 21 cases. Acta ortop bras 15( 5 ]: 272-275.
- Kohli S, Vishwakarma N, Chauhan S, Salgotra K (2017] Functional evaluation of fixation for PCL bony avulsion fractures using Burk and Schaffer's approach. International Journal of Orthopaedics 3(1): 735739.
- Trickey EL (1968] Rupture of the posterior cruciate ligament of the knee. J Bone Joint Surg Br 50: 334-341.
- Hughston JC (1954) The posterior cruciate ligament in knee joint stability. J Bone Joint Surg Am 54: 1045-1046.
- Van Dommelen BA, Fowler PJ (1989] Anatomy of posterior cruciate ligament A review. Am J Sports Med 17: 24-29.
- Janousek AT, Jones DG, Clatworthy M, Higgins LD, Fu FH (1999] Posterior cruciate ligament injuries of the knee joint. Sports Med 28(6): 429-441.
- Margheritini F, Mariani P (2003] Diagnostic evaluation of posterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 11(5): 282-288.
- Shelbourne KD, Muthukaruppan Y (2005) Subjective results of nono- peratively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy 21(4): 457-461.
- Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT (2007) The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J 3(2): 137-146.
- Sekiya JK, Whiddon DR, Zehms CT (2008) A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am 90(8): 1621-1627.
- O'Donogue DH (1950) Surgical treatment of fresh injuries to major ligaments of knee. J Bone Joint Surg Am 32 A(4): 721-738.
- Torisu T (1979) Avulsion fracture of the tibial attachment of the posterior cruciate ligament. Indications and results of delayed repair Clin Orthop Relat Res 143: 107-114.
- Jung TM, Höher J, Weiler A (2006) Screw fixation of a 4 1/2-year-old PCL avulsion injury. Knee Surg Sports Traumatol Arthrosc 14(5): 469-472.
- Singla R, Devgan A, Gogna P, Batra A (2014) Fixation of delayed union or nonunion posterior cruciate ligament avulsion fractures. J Orthop Surg (Hong Kong) 22(1): 70-74.
- Burks RT, Schaffer JT (1990) A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res 254: 216-219.
- Miyasaka K, Daniel D, Stone M (1991) The incidence of knee ligament injuries in the general population. Am J Knee Surg 4: 3-8.
- Fanelli GC, Beck JD, Edson CJ (2010] Current concepts review: the posterior cruciate ligament. J Knee Surg 23(2): 61-72.
- Veltri DM, Deng XH, Torzilli PA, Warren RF, Maynard MJ (1995] The role of cruciate and posterolateral ligaments in stability of the knee. A biomechanical study. Am J Sports Med 23(4): 436-443.
- Margheritini F, Mariani P (2003] Diagnostic evaluation of posterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 11(5): 282-288.
- Nicandri GT, Klineberg EO, Wahl CJ, Mills WJ (2008) Treatment of posterior cruciate ligament tibial avulsion fractures through a modified open posterior approach: operative technique and 12 to 48 month outcomes. J Orthop Trauma 22(5): 317-324.
- Bali K, Prabhakar S, Saini U, Dhillon MS (2012) Open reduction and internal fixation of isolated PCL fossa avulsion fractures. Knee Surg Sports Traumatol Arthrosc 20(2): 315-321.
- Shelbourne KD, Muthukaruppan Y (2005) Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy 21(4): 457-461.
- Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004] Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am 86 A(6): 1139-1145.






























