The Original Method for Planning of Surgeries for Bowlegs Correction
Pavel Kulesh1 and Leonid Solomin2,3*
1St. Jeorge City Hosp, Orthopedic department, St. Petersburg, Russia
2Vreden Russian Research Orthopedic Institute, St. Petersburg, Russia
3St. Petersburg State University, St. Petersburg, Russia
Submission: July 21, 2017; Published: July 26, 2017
*Corresponding author: Leonid Solomin, Department of orthopedic, St. Petersburg State University, Russia, Email: solomin.leonid@gmail.com
How to cite this article: Kulesh P, Solomin L. The Original Method for Planning of Surgeries for Bowlegs Correction. Nov Tech Arthritis Bone Res. 2017; 003 1(4): 555566 DOI: 10.19080/NTAB.2017.01.555566
Abstract
The authors developed the method for preoperative planning of surgeries for bowlegs correction by using of standing long-films. The method (Patent of the Russian Federation 2547252] based on visualization of the soft tissues contour and contours of the long bones. It combines the advantages of planning by using roentgenograms and planning by using photographs. The method allows predetermining the mutual position of the bone fragments, providing the required shape of the legs, the influence of the operation to the mechanic of the joints due to a change in the relationship of the reference lines and angles. To realize the goal, the thematic literature data were used. The schemes and formulas for calculating the magnitude of different types of manipulations (angulation-valgisation, translation-medialisation, elongation- distraction] for achieving the optimal shape of the legs were taking into consideration. The roentgenograms of 25 patients operated by authors for legs shape correction in 2009-2013 and the roentgenograms of 36 patients operated by other doctors in 2007-2010 were applied for advice. The method was tested in 16 cases.
Keywords: Bowlegs; Shape of legs; Tibia osteotomy; Planning of osteotomy; Deformity of shank.
Introduction
The high tibia osteotomy has become widespread for treatment of metaphysical and epi‐metaphyseal deformities of the shank [1‐11]. However, even its technically correct execution does not guarantee the achieving of “ideal” shape of the legs, accepted in the plastic surgery.
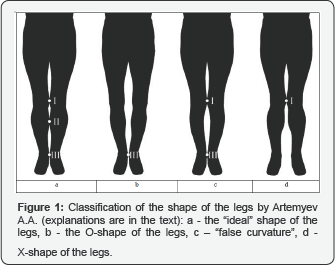
The most widely used classification of the shape of the legs was suggested by AA Artemyev [6]. According to that, were distinguished the “ideal” shape of the legs, O-shape, X-shape and “false curvature” (Figure 1]. In case of “ideal” shape, the legs adjoin in three points located on the medial contours of both limbs. Point I is located at the level of distal metaepiphysis of the femurs, point Il-at the level of the border between the upper third and intermediate third of the diaphysis of the tibias, point Ill-at the level of the distal metaepiphysis of the tibias. The “ideal” shape implies the presence of three spindle-shaped gaps between the medial contours of the legs, bordered by the crotch, adjoining knee joints, soft tissues in the upper thirds of the shins and by the ankles. O-shape of the legs implies that the legs adjoin at point III only, in case of the X-shaped legs at point I, “false curvature” at points I and III. It is possible to determine the type of shape using photographs or long-films.
In case of “false curvature”, the cruroplastic with silicone implants is required. In case of O-or X‐shape of legs, osteotomies and osteosynthesis should be performed. External fixation has the advantage: it allows “to perform correction of the shape of the legs taking into account the wishes of the patient and in cooperation with him” (cited from Artemyev AA] [6]. They generally perform the tibia osteotomy at the level of the proximal metaepiphysis or the upper third of the diaphysis. Correction they usually perform gradually in postoperative period. To reach an "ideal" shape of legs besides valgisation, are necessary medialisation and distraction [1‐6,12‐14].
The known variants of preoperative planning for genu varum treatment can be divided in "orthopedic" and "aesthetic" For "orthopedic" variants, the Reference Lines and Angles (RLA), determined from the roentgenograms, are taken as a basis [5,11]. For example, Miniaci A [10] takes into consideration the anatomical or mechanical tibia‐femoral angle; for Lobenhoffer P, Fujisawa Y & Coventry MB [7‐9] the most important criterion for planning is the deviation of the mechanical axis of the leg (MAD). Orlyansky V [8]. In addition to MAD takes into account the magnitude of the Mechanical Medial Proximal Tibia Angle (MMPTA). Other authors in addition to MAD and MMPTA take into account the value of the Mechanical Lateral Distal Tibia Angle (MLDTA). They carry out the planning of correction by using applications or software by rotating the contour of the distal fragment of the tibia to the position that provides the correct values of the RLA. However, the prediction of the shape (contour)of the legs after correction is not possible by these planning options because of using the skiagrams (contours) of femoral and tibia bones.
The specific software was developed for "aesthetic" planning. These programs are based on using of photos of the patient's legs [2,12]. Some of these programs are available on the Internet (http://legscorrection.ru and http://www.plastio. ru). Performing the planning, user marks the "reference points" on the medial contour of the shins at the level of the osteotomy. He marks centers of hip joints and ankle joints too. The result of the planning is a picture of deformed contour of the patient's legs. The silhouette of every leg is bent to combine the "reference points". The points corresponding to the centers of the hip joints and ankle joints retain previous positions. These methods of planning are visual, but provides not high accuracy. It is possible to determine approximately the centers of joints and the level of osteotomy according to the photo of the legs. Nonconformity of the shape of the legs after treatment to preoperative planning may cause the need of repeated surgery [2,5]. The impossibility of investigating RLA does not allow assessing the influence of the surgery on the mechanics of the joints [5,11].
Thus, it should be noted that at present there is no method of preoperative planning that allows to predict the shape of the legs after the correctional osteotomy, the mutual positions of the bones fragments and the values of the RLA (MAD, mTFA, mLDFA, mMPTA, mLDTA).
a. Purpose of the study
To develop a method for preoperative planning of bowlegs correction providing the possibility to predict the shape of legs and values of RLA after correction.
Material and Methods
Information about the bones fragments movements to perform manipulations for the legs shape correction (valgisation, medialisation, distraction) were obtained from the literature [2‐4,6‐11,12‐15]. The schemes and formulas for calculating the magnitude of valgisation and medialisation for achieving the "ideal" shape of the legs were studied [3,14]. The roentgenograms of 25 patients operated by authors for legs shape correction in 2009‐2013 and the roentgenograms of 36 patients operated by other doctors in 2007‐2010 were applied for advice.
Results
To perform the preoperative planning according the developed method [16] the surgeon should use graphics software. It should provide options for vector and raster graphics processing by layer‐to‐layer mode.
On a digitized standing long‐film of the legs examine the values of the RLA, mark the medial and lateral contours of the legs. Marking the contours of the legs on the roentgenogram is not difficult: the air is a contrast substance with low atomic weight, is used in x‐ray diagnostics to contrast soft tissues as oxygen and carbon dioxide [17].
Draw the line through the middle of the pubic symphysis perpendicular to the bispinal line (line #1). Draw the lines #2 on the levels of the future osteotomies of the tibias (2.5‐3 cm distally from the tuberosities of the tibias [2,4]) perpendicular to the anatomical axes of the proximal third of the diaphysis (Figure 2a). Note the points on the long‐film for the right leg and the left leg:
- The center of the head of the femur.
- The most prominent point of the medial contour of the femur at the level of the distal metaepiphysis ("point I" according to Artemiev AA [6], Figure 1).
- The point of intersection of the medial contour of the shank and the line #2.
- The most prominent point of the medial contour of the shank on the upper or middle third of the tibia ("point II" according to Artemiev AA [6], Figure 1).
- The point of intersection of the lateral cortex of the tibia and line #2.
- The most proximal point of the proximal tibia-fibula joint (the point of intersection of the cortexes of the tibia and fibula bones).
- The intersection point of the line EF and the edge of the roentgenogram.
- The most prominent point of the medial contour of the tibia at the level of the distal met epiphysis of the tibia
- The most distal point of the distal tibia-fibula joint.
- The top of the lateral malleolus.
- The intersection point of the line EF and the edge of the roentgenogram.
Draw the line through the center of the pubic symphysis and point H (line #3). For each leg mark 3 complexes. The complex I is bordered by the upper edge of the radiograph, the right/left edge of the radiograph, the interval GE, the interval EC, the medial contour of the upper third of the shin and the medial contour of the femur, line #3. Complex II is bordered by the intervals CE, EI, IK, the lower edge of the roentgenogram, the line #3 up to the point H, the medial contour of the shank up to the point C. Complex III is bordered by the interval EG, the right/left edge of the roentgenogram, the lower edge of the roentgenogram, the intervals KI and IE (Figure 2a).
Using the options of the graphics software, rotate simultaneous three complexes for each leg around the points A till points B adjoin to the line #1 (Figure 2b).
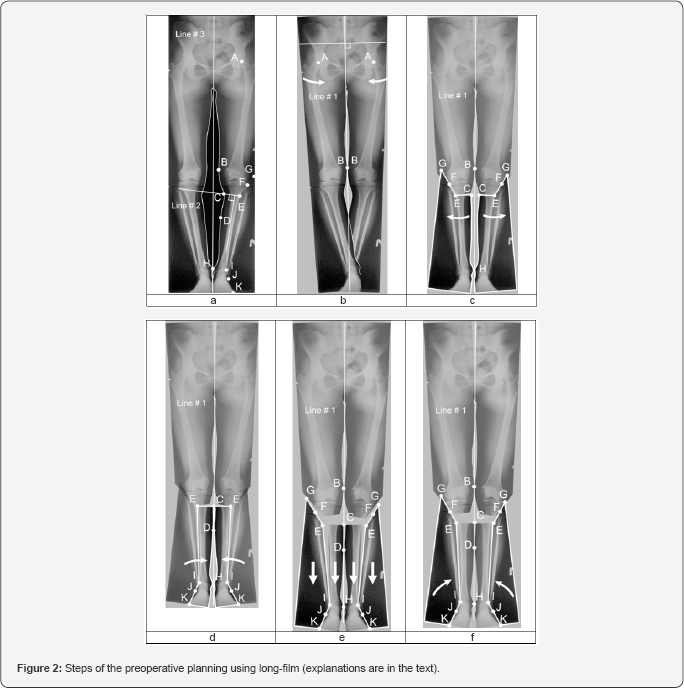
Simulate the valgisations of the distal fragments of the tibias [2,3,6] by simultaneous rotation of the complexes II and III around the points E till points H adjoin to the line #1 (the magnitudes of the angles of rotation of the complexes are equal to the magnitudes of the planning valgisations) (Figure 2c). After that, if points D adjoin to the line #1, make a decision that valgisation is enough to achieve an "ideal" shape of legs. If points D do not adjoin to the line #1 after simulating of valgisation, the resulting shape of the legs corresponds to the "false curvature". The width of the gap between the medial contours of the shanks reflects the amount of curvature.
If the correction of "false curvature" is necessary, perform the second stage: simulate the medialisation of the distal fragments of the tibias [2,3,6,14] by rotating the complexes II around the points I till the points D adjoin to the line #1 (Figure 2d). The distances between the positions of the points C before rotation and after is equal to the magnitude of the planned medialisation. The shanks become wider on the distance from point E of complex III to point E of complex II.
If the shanks after medialisation seem too wide to the patient, simulate the moving down of the fibulas [3, 6,18] by moving distally complexes II and III (Figure 2e). After that ‐rotate the complexes III around points I until points F adjoin lateral cortexes of the tibias. If the patient insists on keeping the same widths of the shanks as before surgery, simulate the moving down of the fibulas until the points E of the complexes II adjoin to points E of the complexes III (Figure 2f).
The result of preoperative planning is the picture of the shape of the legs after correction and mutual locations of bones fragments to provide that shape. After that, measure the magnitude of the necessary valgisation, medialisation and distraction to obtain the desired shape of the legs and investigate RLA corresponding to planned variant of correction.
a. Clinical case
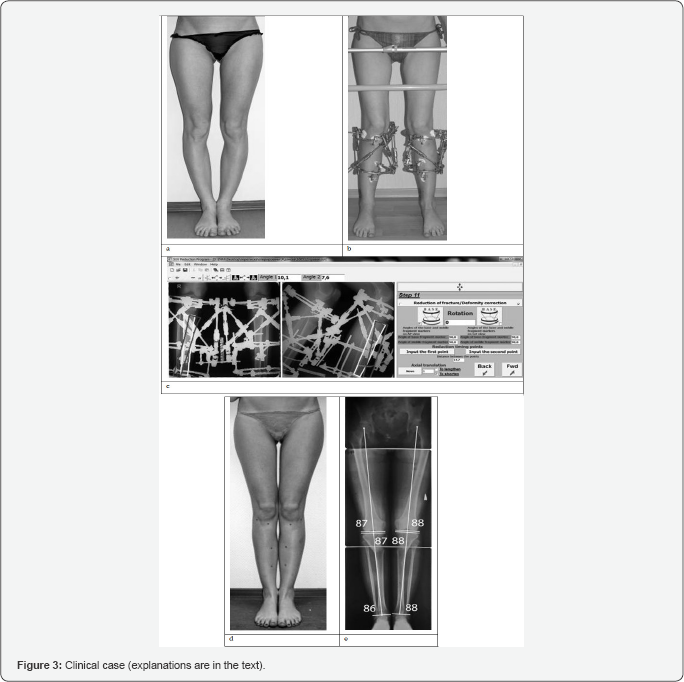
The female 23 y.o. came to Vreden Russian Research Institute of Traumatology and Orthopedics on February 14, 2012. She was unhappy with her legs shape (Figure 3a), having complaint of bowlegs without pain (O‐shaped legs). Pathological changes of hip, knee, and ankle joints using physical and ultrasound examination and MRI were not revealed.
Preoperational planning was performed according to the original method. It was found that achieving an "ideal" shape of legs by valgisations is not possible (Figure 2c). That is why were simulated valgisation (right ‐3°, left *#8208;6°) and medialisation (right‐10mm, left ‐12mm). According to the planning, after these procedures the shanks will become 10mm wider (Figure 2d). When modeling the moving down of the fibulas, it was found that for keeping the initial width of the shanks the distraction on 4 cm is needed (Figure 2e). The patient refused the lengthening on 4cm because of long treatment period. She insisted on lengthening on 1, 5cm.
The surgery of both tibias osteotomies and external fixation was performed on February 15, 2012. To simplify the correction, software based Ortho‐SUV Frames (http://ortho‐suv.org) were applied [5] (Figure 3b & 3c). The use of these units provides precise, one‐step gradual deformity correction. It was performed according to preoperative planning in 71 days. The fixation period took 89 days. After that frames were removed (Figure 3d). The achieved shape of the legs corresponds to the "ideal" and completely corresponds to the patient's requests (Figure 3d). The values of the RLA are shown at (Figure 3e).
Discussion
The original method of planning were applied in 16 cases. The analyses demonstrates that in 13 cases (84%) the shape of the legs after correction was equal to preoperative planning. At the same time, it was established that the method has specific for "orthopedic" and "aesthetic" types of planning disadvantage. Simulating of torsion of the distal fragments of the tibias is impossible. We believe that this problem will be solved by application of software for three-dimensional modeling.
Conclusion
The developed method of preoperative planning for bowlegs correction makes it possible to determine the mutual positions of bones fragments that provide the required shape of the legs, as well as the influence of the operation to the mechanic of the joints due to changes in the relationship of reference lines and angles. A detailed study will be devoted to an in‐depth analysis of the application of this method and its comparison with alternative versions.
Summary
Authors worked out the method of preoperative planning of bowlegs correction. It is based on the application of standing long-films. It combines advantages of preoperative planning using photographs and long‐film radiograms by visualization of lower limbs shape and bones contours. It allows predetermining positions of the bone fragments, providing the necessary shape and relationship of the reference lines and angles. The method was applied in 16 cases.
References
- Bagirov AB, Rudkovsky AA, Kafanov AV (2002) Aesthetic orthopedics of the shins Kremlovskaya meditsina. Clinical Herald 4: 50-52.
- Kaplunov OA, Kaplunov AG, Shevtsov VI (2010) Cosmetic correction of the shape and length of the legs. M GEOTAR Media p. 160.
- Marker NA (2009) Prediction of tactics and the result of orthopedic cosmetic correction of tibial deformity [dis candhoney Sciences]. Kurgan, FGU RNC of the WTO Acad GA Ilizarova.
- Novikov KI (2008) Operative lengthening of limbs in patients with low and subjectively low growth by the method of controlled transosseous osteosynthesis: author's abstract. Dis Dr med Sciences Kurgan, p. 34.
- Solomin LN (2015) Fundamentals of transosseous osteosynthesis. Pererab. And add, (1st ed) BINOM T.
- AA Artemyev (2008) Aesthetic and reconstructive surgery of the lower extremities / ed. M GEOTAR-Media 248 p. (Library of a specialist doctor, orthopedics, surgery).
- Coventry MB, Ilstrup DM, Wallrichs SL (1993) Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 75(2): 196-201.
- Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin Noth Am 10(3): 585-608.
- Lobenhoffer P, Agneskirchner JD, Gala M (2007) Kniegelenknahe Osteotomien. Thieme 161.
- Miniaci A, Ballmer FT, Ballmer PM, Jakob RP (1989) Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res 246: 250-259.
- Paley D (2003) Principles of deformation correction. Springer-Verlag 806, New York, USA.
- Egorov MF, Chernov AP, Nekrasov MS (2000) Orthopedic cosmetology. pp. 192.
- Ilizarov GA, Shevtsov VI, Shatokhin VD (1981) Results of operative thickening, modeling of the form and elongation of the shin (in outpatient conditions). Orthopedics, traumatology and prosthetics 10: 23-26.
- Orlyansky V, Golovakha M, Shvabus R (2009] Corrective osteotomy in the knee joint area. ^HinponepoBCbK: Thresholds 159.
- Barinov AS, Vorobiev AA, Zaitsev SS (2010) Cosmetic aspects of operative correction of dysplastic varus deformities of lower limbs.
- Sergeev PV, Sviridov NK, Shimanovskiy NL (1980) Radiopaedics. pp. 239.
- A method for pre-operative planning of corrective osteotomies of the shin bones to correct the O-shape of the legs: a. from. N 2547252 Ros Federation.
- A method for correcting the shape of the shin using transosseous osteosynthesis and a rod-screw for its implementation: a from No. 2480176 Ros Federation.






























