Granular Cell Tumor
Sravanthi Nandavaram*, Amish Shah and BirendraSah
Division of Pulmonary Critical Care, SUNY Upstate Medical University, USA
Submission: March 15, 2017; Published: April 20, 2017
*Corresponding author: SravanthiNandavaram, 50 Presidential plaza, Apt 2106, Syracuse, NY 13202, USA, Tel: 315 350 7332; Email: drsnandavaram@gmail.com
How to cite this article: Sravanthi N, Amish S, BirendraS. Granular Cell Tumor. J Tumor Med Prev. 2017; 1(1): 555553. DOI: 10.19080/JTMP.2017.01.555553
Abstract
Introduction: Granular cell tumors are rare neoplasms, which can be either benign or malignant. They are often discovered as incidental findings on imaging.
Case: 34-year-old smoker, with complaints of fever, chills; malaise was found to have a posterior mediastenal mass on chest imaging. EBUS guided FNA of the mediastenal mass revealed histopathologic features consistent with benign granular cell tumor. Patient underwent thoracotomy and required right lower bi-lobectomy and re implantation of the right upper bronchus to the trachea, as mass was adherent o the right main stem bronchus.
Discussion: Granular cell tumors are rare slow growing neoplasms, also known as Abrikosoff tumors, commonly present in the fourth to sixth decade of life. They are of Schwann cell origin and can involve any organ of the body. GCT's are characterized with pathologic features of homogenous cells containing abundant eosinophilic granular cytoplasm with periodic acid Schiff (PAS) positive and diastase resistant granules. GCT's can be classified into benign, atypical and malignant GCT's based on the histologic criteria and Ki-67 index. For benign and atypical granular cell tumors, wide local excision with clear margins is curative. Malignant granular cell tumors often require adjuvant radiotherapy in addition to the local surgical excision.
Keywords: Granular; Neoplasm; Benign; Schwann; Tumor
Abbreviations: CT: Computed Tomography; EBUS: Endobronchial Ultrasound; FNA: Fine Needle Aspiration; GCT: Granular Cell Tumor; TTF1: Thyroid Transcription Factor 1; PAS: Periodic Acid Schiff stain
Introduction
Granular cell tumors are rare, slow growing neoplasms, which commonly present in the fourth to sixth decade of life. They are of Schwann cell origin and can involve any organ of the body. Diagnosis is based on histopathologic features of homogenous cells with abundant eosinophilic granular cytoplasm.
Here we present a case of incidental posterior mediastenal mass in a young man, diagnosed as benign granular cell tumor via EBUS guided FNA. Surgical removal was attained via right thoracotomy however was complicated as it was adherent to the right main stem bronchus and required en-bloc right lower bilobectomy and re-implantation of the right upper bronchus to the trachea.
Case
34-year-old male, active smoker, with medical history significant for obstructive sleep apnea presented with complaints of fever, malaise and headache. Patient reported a raccoon bite two days prior to the symptoms starting. He did not report any cough, shortness of breath or unintentional weight loss, or sick contact. He denied any history suggestive of photophobia, hydrophobia or laryngeal spasms. He works as a mechanic, denied any significant occupational exposures. Denied any recreational drug use. Denied any recent history of travel or human sick contact.
Physical exam was significant for pinpoint erythematous area on left side of the neck at the site of raccoon bite. Finger tips had multiple superficial cuts. Rest of the physical exam was benign. Complete blood count and basic metabolic panel were within normal limits. Lumbar puncture was performed and the chemistries, cell count were within normal limits. He received rabies post-exposure prophylaxis.
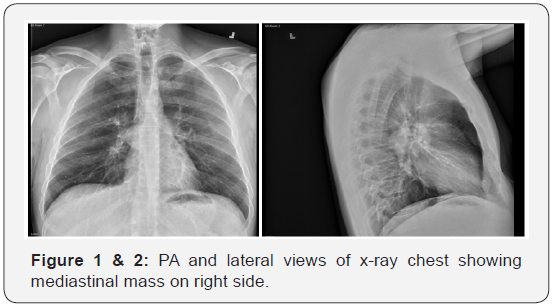
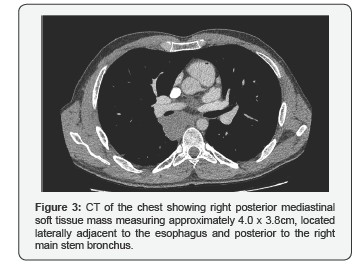
As a part of infectious work up for fever, chest x ray was done which revealed a mediastinal mass. CT Chest showed posterior mediastinal soft tissue mass adjacent to the esophagus and posterior to the right main stem bronchus. EBUS did not show any bronchial or esophageal involvement of the tumor. EBUS Guided FNA of the mediastinal mass was performed. FNA Cytopathology revealed numerous bland cells with eccentric nuclei and abundant eosinophilic granular cytoplasm. Immunostains were positive for S100, CD68 and negative for TTF-1. PAS with and without diastase shows diastase resistant granules (Figure 1,2 & 3).
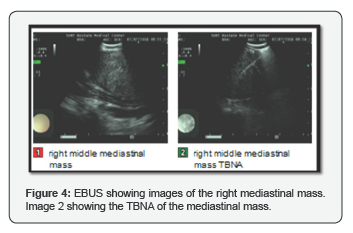
Patient subsequently underwent right thoracotomy for resection of right mediastinal mass. The tumor was easily resected off the esophagus but was adherent to the right main stem bronchus and required en-bloc right lower bi-lobectomy and re-implantation of the right upper bronchus to the trachea. The resected mass showed homogenous bland cells with granular eosinophilic cytoplasm and eccentric nuclei. No mitotic activity is seen. The margins were negative and there was no evidence of lymph-vascular invasion. The tumor cells showed a similar histologic appearance to those seen in the cytology specimen. Immunohistochemistry showed cytoplasmic expression of S-100. PAS with diastase shows strong granular staining of the cytoplasm. MyoD-1 is negative. The tumor cells did not demonstrate atypical features that can be associated with malignant behavior in granular cell tumors including pleomorphism, spindle cells, prominent nucleoli, necrosis, and mitoses greater than two per 10 high power fields. The lymph nodes 10R, 11R did not show any evidence of tumor involvement (Figure 4).
Discussion
Granular cell tumors (GCT) also known as Abrikosoff tumor are rare, slow growing neoplasms. They were first described by Abrikosoff in 1926 and hence the name Abrikosoff tumor [1]. Originally these tumors were thought to be of smooth muscle origin. Subsequently in 1962, immunohistochemistry and ultrastructural studies revealed that these tumors are of Schwann cell origin [2]. Granular cell tumors can involve any organ of the body, with the most common sites of involvement being head and neck region, skin and soft tissues [3].
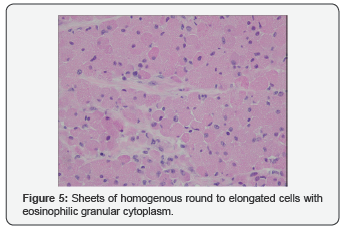
Granular cell tumors commonly present in the fourth to sixth decade, but can appear at any age [3]. Given the slow and indolent course of these tumors, the patients are usually asymptomatic on presentation and often discovered as an incidental finding on imaging studies [4]. Presence of sheets and cords of large, polygonal, round, or elongated cells containing abundant eosinophilic granular cytoplasm with periodic acid Schiff (PAS) positive and diastase resistant granules is the characteristic histological feature of GCT's. [5,6] These round eosiniophilic granules surrounded by a light halo are termed as pustule ovoid bodies of Milian. GCT's express S-100 protein, CD 68 and vimentin. GCT that does not express S100 protein, but show reactivity for CD68,NK1C3, CD10, and a1-antitrypsin are termed as non-neural GCT (Figure 5).
GCT's can be classified into benign, atypical and malignant GCT's based on the histologic criteria and Ki-67 index. Ki-67 is a marker of cell proliferation. Based on the Ki-67 index, GCT's can be differentiated into benign GCT (<5%), atypical GCT (5-10%) and malignant GCT (10-50%) [7].
Based on the six histologic features of nuclear pleomorphism, tumor cell spindling, vesicular nuclei with large nucleoli, increased nuclear: cytoplasmic ratio, necrosis, and mitotic rate, GCT's can be classified as malignant if they have 3 or more of these features, atypical with the presence of 1 or 2 features and benign GCT in the absence of these features [5-9].
Malignant granular cell tumors constitute about less than 2% of granular cell tumors [5]. These malignant granular cell tumors are characterized by rapid growth, likely to recur and have the potential to metastasize, with the lungs, lymph nodes and bones being the most common sites of metastasis. It's the evidence of atypia, with marked increased cellularity, prominent spindle or pleomorphic cells, a high Nuclear: Cytoplasmic ratio, prominent nucleoli, increased mitotic activity, and focal or extensive tumor necrosis, which differentiate the malignant GCT from benign GCT. Large tumor size, deep soft tissue location, necrosis, and distant metastasis are commonly seen with malignant GCT's [6-9]. Invasion of adjacent structures is not a criterion for GCT to be malignant. In the series of Fanburg-Smith et al. [6] patients with benign or atypical histology had a benign clinical course without metastases. However local recurrence was detected patients with atypical GCT. The size of the primary tumor, older the patient age, and the presence of metastases, Ki-67 values >10% and p53 immuno reactivity are considered as the poor prognostic factors. Given the rarity of these tumors, there are no large clinical trials or long term follow-up studies or oncology treatment protocols and most of the data stems from case reports and case series. For benign and atypical granular cell tumors, wide local excision with clear margins is curative. Malignant granular cell tumors often require adjuvant radiotherapy in addition to the local surgical excision [3-6,8]. There have been reports of malignant cases of granular cell tumors with lung metastasis, which were treated with adjuvant radiotherapy and chemotherapy. Malignant GCT's are associated with P1K3CA gene alteration raising the possibility of role of targeted inhibitors (such as P13K/AKT/mTOR inhibitors) in malignant GCT's with such specific gene alterations [6,7]. Irrespective of the histological type of the granular cell tumor, patients should be followed up for recurrence and metastasis.
Conflict of Interest
The authors SravanthiNandavaram, Amish Shah and BirendraSah, certify that we have no affiliations with or involvement in any organization or entity with any financial interest in subject matter discussed in this manuscript.
References
- Montojo J, Echarri R, Santana A, Micó A, Gamboa J, et al. (1999) A multifocal granular-cell tumor of the upper airways. Acta Otorrhinolaringol Esp 50(6): 498-501.
- Garín L, Barona R, Basterra J, Armengot M, Alemany P, et al. (1992) Granular cell tumor (Abrikosoff's tumor). A review and our experience. An Otorrinolaringol Ibero Am 19(3): 249-264.
- Kamal SA, Othman EO (1998) Granular cell tumor of the larynx. J Laryngol Otol 112(1): 83-85.
- Torrijos-Aguilar A, Alegre-de Miquel V, Pitarch-Bort G, Mercader-García P, Fortea-Baixauli JM (2009) Cutaneous granular cell tumor: a clinical and pathologic analysis of 34 cases. Actas Dermosifiliogr 100(2): 126132.
- Rekhi B, Jambhekar NA (2010) Morphologic spectrum, immunohistochemical analysis, and clinical features of a series of granular cell tumors of soft tissues: a study from a tertiary referral center. Ann Diag Pathol 14(3): 162-167.
- Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG (1998) Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol 22(7): 779-794.
- Machado I, Cruz J, Lavernia J, Llombart-Bosch A (2016) Solitary, multiple, benign, atypical, or malignant: the "Granular Cell Tumor” puzzle. Virchows Arch 468(5): 527-538.
- Bitar M, AlAfif KA, Fatani MI (2011) Granular Cell Tumor: Case Report. Journal of the Saudi Society of Dermatology & Dermatologic Surgery 15(1): 25-27.






























