Non-Invasive Method of Nailing of the Distal Radius Fractures
Persoons D*
Orthopaedic Surgeon, Saverne hospital, France
Submission: February 25, 2019; Published: March 18, 2019
*Corresponding author: Persoons D, Orthopaedic Surgeon, Saverne hospital, France
How to cite this article: Persoons D. Non-Invasive Method of Nailing of the Distal Radius Fractures. J Phy Fit Treatment & Sports. 2019; 6(2): 555682. DOI:10.19080/JPFMTS.2018.05.555682
Introduction
The fracture of the distal radius is frequent [1]. It is estimated that 150,000 people sustain a distal radius fracture every year in France [2]. The simplicity, the efficiency and the low cost of the surgical procedure are decisive factors in terms of public health. Therefore, their mechanism should better be fully understood [3-5]. In order to operate on those patients with very few skin damages, an appropriate reduction is necessary before the nailing procedure. And, when the nail is placed, the material must fit to prevent any secondary collapse. Overall, if the spongious bone underwent a deep crush. But if the material is correctly adapted, it is reasonable to offer a stable and non-invasive osteosynthesis of those kinds of fractures. The radius is a long, relatively straight bone, and frequently subject to fractures because of its protective role in the event of a fall or accident. The long wires were first used during the first World War while the flexible pins were described as early as the 1950s. Several types of flexible nails dedicated to distal fractures appeared in the early 2000s. Today, there are specifically designed wires for fractures of the radial diaphysis.
Material
The Compaction Chambers
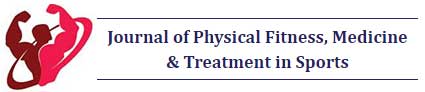
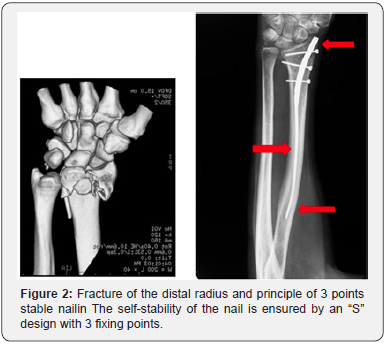
During a fall, the wrist undergoes a force of compression and flexion which causes a crush of the bony trabecular structure of the distal radius. The cortical break comes along with the flattening of the deep cancellous bone. The first principle of a closed nailing is to recognize the existence of a “compaction chamber”, that is to say a void of bone. The aim is to reopen this chamber and keep its banks well apart to restore the length of the radius. The elasticity of the nail has to enable to maintain this opening. This principle was described by Desmanet in 1989 [6]. Some implants have even been specially designed to fill the void of the compaction chamber. They have the disadvantage of being bulky and not providing any mechanical stability. However, they widely open the fracture focus and they offer the advantage of showing the volume of bone loss at the distal metaphysis level (Figure 1).
Method of Preliminary Reduction
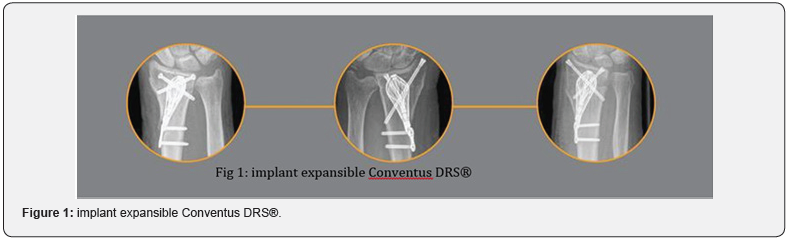
The fracture of the distal radius is reduced by manual traction. It dis impacts the fracture site and reopens the metaphysis. The nail, as a central stake, maintains the reduction and the void thus created (Figure 2-4).

The Long History of the Non-Invasive Osteosynthesis
The nailing of long bones was described by R. Danis of the University of Brussels (Belgium) in 1938 and by G. Küntscher at the University of Kiel (Germany) in 1939. The later used his nails on the wounded of the Finnish front during the Second World War [7]. The transverse locking of the nail has been described by Modny and Bambara in 1953 [8]. This lock was improved by Kempf & Grosse [9] in 1978 to the point where it prevailed over the screw plate osteosynthesis which popular in the 1960-1980. This method has revolutionized the treatments of long bones fractures. Since de year 2000 it has been applied to the upper limbs. The real goal was to go back to closed focus osteosynthesis as done for the lower limbs. Most recent series seem to show the equivalence of radiological and functional results, between closed nailing and the anterior plates. “The present study supports the view that intramedullary nail fixation and flat fixation for the treatment of displaced extra-articular distal radius fractures have equivalent radiographic and functional outcomes. Garcia said [10] (Figure 5).

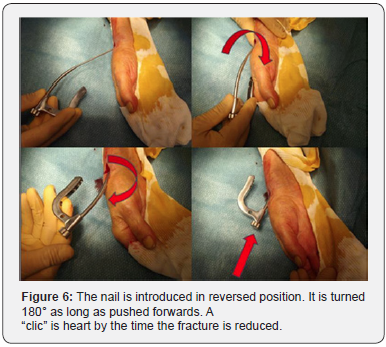
Nail-o-flex® Nailing Procedure
The Nail-o-flex® nail was introduced in 2005. It is a specific nail for fractures of the distal radius. It comprises a distal portion which is perforated and a long, smooth proximal part that is thin and flexible to ensure elasticity. The nail-o-flex® nail application technique is directly derived from the long bones nailing of the lower limb. The radius fracture is reduced by manual traction. The nail is inserted at the level of the snuffbox, outside the tendinous areas. The entrance is perforated with a small square point. The nail has an “S” shape. It is inserted with curvature upside down to fit the metaphyseal angle, it is then turned over and entirely inserted. It is stopped by the aiming frame which stumbles on the radial styloid. Locking is performed as for the femur or tibia. The nail is freestanding thanks to its “S” design and its 3 points of support. It is also elastic since the 2/3 of the nail are fine as a pin (2mm) and automatically realigns the distal epiphysis and keeps the focus open. It must be locked at its distal part, with at least two epiphyseal screws (Figure 6).
Method

Between May 2008 and May 2015, the Nail-o-flex® nail was used to treat fractures of the lower end of the radius. All cases presenting an extra-articular fracture (Colles or Smith) and/or an intra-articular fracture (except marginal fracture and comminuted fractures with 4 fragments or more) have been treated. The preliminary series includes 83 cases. Of these 83 cases, the female/male ratio was 7 to 1. The average age was 67 years, ranging from 18 to 89 years. Average operating time was 45 minutes. The hospital stay was 2 days up to 2013, when all these fractures were then treated as outpatients. A Velcro splint has been routinely used for a period of 5 weeks. The clinical results were analyzed with the Constant score: 55 excellent, 20 satisfactory and 8 poor result. There was no redo for insufficient result. Fractures have been classified according to Laulan & Bismuth [11]. The purpose of this Clinical Series was to confirm that metaphyseal bone defect could be treated with an elastic nail according to the principle of Desmanet, without graft or surrogate, and that the distal epiphyseal lock was sufficient to keep the epiphyseal fragments in a good position during the entire consolidation period. In this series, we have shown that 75/83 cases had retained a radio-ulnar index less than or equal to 0. This shows a good restoration of the length of the radius. These cases correspond to the 75 cases of the pre-series (Figure 7).
Discussion
The nailing of the fractures of the radius is an outsider because there is a kind of unanimity about the anterior screwed plate. One can criticize plates to be inserted openly opposite to the damaged area. This can be the source of additional pain. However mini-nails of the radius have been compromised by unreliability and limited indications. None of them had incorporated the need for an elastic recall force to oppose the natural compaction of the compaction chamber. This is the originality of the nail-o-flex® nail. The nail-o-flex® nail is a “nail-pin” that combines distal locking of Kempf and Grosse and the proximal elasticity of Desmanet. As so it can behave like an internal distractor. Improvements have been made on the quality of the locking screws and the accuracy of the viewfinder. Today this nail is a simple to use for any operator familiar with the femur or tibia nails.
a) The Compaction Chambers
The first question in the distal radius fractures seems the loss of bone matter in the metaphyseal region due to the flattening of the spongy bone. The clinical series has shown that the radius only recoils in 10% of cases (75/83), whereas this complication was frequent with the Kapandji type entanglements. Efficiency seems to be due to the fact that the nail acts as a central guardian, without shear stress.
b) The Reduction must be Accurate. And secondarily, to Maintain A Self-Stable
epiphyseal reduction is obligatory. The use of palmar plates may seem paradoxical since the bone comminution is mainly on the opposite side [11-13]. The operator does not have access to it. Even self-stable screws cannot replace a missing bone. Many authors question themselves about this method which is widely diffused [13-15]. The intramedullary percutaneous nail is mechanically more logical. It is central, thus more neutral and simpler to use. Lateral approach is direct and offers more security.
c) To maintain a good orientation of the radial epiphysis: The functional result is good if the 15° epiphyseal anteversion is restored. One tolerates a tilting of only a few degrees because it does not have any impact on the degree of flexion of the wrist. But a retroversion of the epiphysis was considered a poor result, even if the index radio-ulnar remained equal to zero. We found 7 poor cases, mainly at the beginning of the series. However, the absence of shortening of the radius made it possible to maintain normal pronosuppination. Patients therefore did not feel the need for a redo.
d) The painful assessment is favorable. It is recognized that closed osteosynthesis are less painful than open procedures as screwed plates. (Kempf I., Leung KS, “Practice of intramedullary locked nails.” Springer, 2002).
e) The aesthetic aspect is interesting. The intervention is conducted by 3 or 4 holes of 2 or 3 mm (Figure 8).

f) And its cost is low (the implant costs 250 euros) [16].
Conclusion
Distal radius pinning is proving itself to be logical and reliable. The Nail-o-flex® nail was designed in 2005. Its aim was to offer an immediate stability along the radial shaft with an effective grip on the proximal diaphysis (3 support points). This seems to offer indeed a stable length restoration of the radius bone. With its 12 years of success records, the nail is a simple and inexpensive osteosynthesis implant. Its use is easy for any surgeon familiar with the pinning of the tibia. Its reliability is comparable to the best series of palmar plates. It requires only moderated X-ray irradiation.
References
- Wilcke MKT, Hammarberg H, Adolphson PY (2013) Epidemiology and changed surgical treatment methods for fractures of the distal radius. A registry analysis of 42, 583 patients in Stockholm County, Sweden, 2004-2010, Acta Orthopaedica 84(3): 292-296.
- Ostéoporose: stratégies de prévention et de traitement - Paris: INSERM (1996) (Expertise collective) 1(6): 85-87.
- Persoons D Fracture du radius distal: Comment prolonger la philosophie de Kapandji trucs et astuces en chirurgie orthopédique, Sauramps medical, Tome 11: 212-215.
- The Treatment of Distal Radius Fractures: Guidelines by AAOS (2009) Point n° 13,14; Key Recommendations Adopted by the American Academy of Orthopaedic Surgeons.
- Tsuchia F, Naito K, Mogami A, Obayashi O (2013) New Technique for dorsal fragment reduction in distal radius fractures by using volar bone fenestration J Orthop. Case Reports 3(2): 8-11.
- Desmanet E (1989) Osteosynthesis of the radius by double elastic spring-pinning. Functional treatment of the distal end fractures of the radius. A study of 130 cases. Ann Chir Main 8(3): 193-206.
- Küntscher K (2015) Die Tecknik der Marknagelung des Oberschenckels. Zbl F Chir, 1940z: 1145) (Rommens P, Hessmann MH, Intramedaullary nailing, a comprehensive guide, Springer-Verlag 3-7.
- Modny MT, Bambara J (1953) The perforated intramedullary nail: preliminary report of its use in geriatric patients, J Am Geraiatr Soc 1(8): 579-588.
- Kempf I, Grosse A, Lafforge D (1978) L’apport du verrouillage dans l’enclouage centro- médullaire des os longs Rev Chir Orthop 64: 635-1
- Obert L, Leclerc G, Blanchet P, Vichard P, Garbuio P (2008) Fractures of distal radius with dorsal displacement treated with palmar plates: fashion trend or real progress? In: maîtrise orthopédique, N°171, Fé
- Diaz-Garcia R, Oda T, Shauver MJ, Chung KC (2011) A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly J Hand Surg Am 36(5): 824-35.
- Hull P, Baraza N, Gohil M, (2011) Volar locking plates versus K-Wires fixation in dorrsally displaced Radius Fractures. A Functional outcome Study, J Trauma 70(6): E125-E128.
- Grad G, Mielscha M, Wendta M, Falka S, Mittlmeiera T (2014) All: Injury 45(1): S3-S8.
- Margaliot Z, Haase SC, Kotsis SV, Kim HM, Chung KC (2005) A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures J Hand Surg Am 30(6): 1185-99.
- Mattila VM, Huttunen TT, Sillanpää P, Niemi S, Pihlajamäki H, et al. (2011) Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland, J Trauma 71(4): 939-42, discussion 942-943.
- Pino S, Bonila J, Borras J (2011) Comparative study of distal radius fracture treated with volar plate or external fixation. J Bone J Surg B p. 99-8.