Introduction
Universal Health Coverage (UHC) remains a critical yet elusive goal for many Low/Middle-Income Countries (LMICs). This is particularly the case in sub-Saharan Africa where systemic challenges such as workforce shortages, inadequate infrastructure, and inefficient health information systems persist [1]. Sierra Leone, a nation still recovering from the devastating 2014-2016 Ebola epidemic, exemplifies these struggles. Its fragile health system continues to face high maternal mortality rates (717 per 100,000 live births) and child mortality rates (109 per 1,000 live births) [2]. Healthcare workforce density in the country is among the lowest globally, with only 0.2 physicians and 1.1 nurses per 1,000 population far below the WHO-recommended threshold [3]. These deficiencies are compounded by stark urban-rural disparities, where 70% of the healthcare professionals are concentrated in Freetown, leaving rural populations severely underserved [4].
In response, the Sierra Leone National Health Sector Strategic Plan (NHSSP, 2021-2025) prioritizes UHC as a key objective, emphasizing the need for innovative approaches to strengthen the health system [4]. One promising avenue is the strategic integration of health informatics; defined as the interdisciplinary use of Information Technology (IT), data science, and digital communication to improve healthcare delivery, education and decision-making [5]. Globally, digital health interventions such as Electronic Health Records (EHRs), telemedicine, and mobile health (mHealth) applications have demonstrated significant potential in enhancing healthcare access, efficiency, and quality; particularly in resource-limited settings [6]. For instance, Rwanda’s mUbuzima telemedicine platform reduced referral delays by 40% and improved diagnostic accuracy in rural clinics [7]. Similarly, Ghana’s use of mobile-based clinical decisionsupport tools increased adherence to malaria treatment protocols by 35% [8].
However, the adoption of health informatics in Sierra Leone is still in its infancy. Only 30% of the health facilities report using any form of digital record-keeping, and fewer than 20% of the healthcare workers have received formal training in health IT systems [4]. This gap is particularly pronounced in health education, where medical and nursing schools continue to rely on traditional, lecture-based pedagogies with minimal exposure to digital tools [9]. Given that a well-trained workforce is the backbone of UHC, the absence of informatics-integrated curricula perpetuates skill deficits and inefficiencies in service delivery.
Despite global evidence supporting the role of informatics in advancing UHC, Sierra Leone lacks a coherent strategy for incorporating digital health competencies into medical and allied health education. Existing literature on health informatics in LMICs predominantly focuses on service delivery (e.g., telemedicine, electronic health records EHRs) rather than education and training [10]. Few studies have ever examined how informatics can be systematically embedded in health profession curricula to produce a digitally proficient workforce capable of leveraging technology for improved care. Thus, the key unresolved questions include: i) How is health informatics currently being taught (or neglected) in medical and nursing schools in Sierra Leone? ii) What infrastructural, financial, and policy barriers hinder the adoption of digital health education in the country? iii) Which scalable context-appropriate informatics models could be adapted to the constraints Sierra Leone?
Addressing these gaps is critical for developing sustainable interventions that align with UHC goals in Sierra Leone. Without targeted investments in health informatics education, the country risks perpetuating a cycle of dependency on external technical assistance rather than building local capacity for long-term system resilience. Thus, this study sought to: i) Assess the current state of health informatics integration in health education system in Sierra Leone, including curriculum content, digital literacy levels, and institutional readiness; ii) Identify barriers and facilitators to the adoption of informatics-based training, with a focus on infrastructure, policy, and sociocultural factors; and iii) Propose evidence-based policy recommendations for embedding informatics in health education to accelerate progress toward UHC delivery.
This research contributes to both academic and policy discourse by providing a comprehensive assessment of health informatics in the education sector of Sierra Leone, filling a critical knowledge gap in digital health literature for LMICs. The findings of the study will also inform policymakers, educators, and development partners on scalable strategies to modernize health training through Information and Communication Technology (ICT). Then lessons learned can serve as a model for other postconflict and epidemic-affected nations striving to strengthen healthcare systems via informatics.
Materials and Methods
Study Design
The sequential mixed-methods design was used in this study to evaluate the integration of health informatics into medical and nursing education in Sierra Leone, with the goal of advancing sustainable UHC. The research design was particularly suited to health systems research in low-resource settings, as it effectively combined the generalizability of quantitative data with the contextual depth of qualitative insights [11]. Given the multifaceted nature of health informatics adoption (encompassing technological, educational, and policy dimensions), this approach enabled a thorough examination of both prevalence indicators (such as digital literacy rates) and underlying determinants (including institutional barriers and policy gaps).
The study first used the quantitative phase, which involved a cross-sectional survey of 250 healthcare trainees and instructors across five major health training institutions in Sierra Leone. This was followed by a qualitative phase, comprising in-depth interviews and focus group discussions with policymakers, IT specialists, and educational administrators. This sequential design allowed quantitative findings to inform the development of qualitative probes, facilitating deeper investigation of key trends [Ivankova et al., 2006]. The study received ethical approval from the Research and Development Directorate of Njala University (Ref: NUDRD-2025-010), with all participants providing informed consent.
Sample Size
For quantitative data, the target population included medical students, nursing trainees, and instructors from five key institutions: College of Medicine and Allied Health Sciences (COMAHS), Sierra Leone School of Nursing and Midwifery, Eastern Polytechnic School of Clinical Sciences, Njala University Department of Public Health, and Ernest Bai Koroma University of Science and Technology Medical School. A stratified random sampling technique was used to ensure fair representations across the institutions, disciplines (medicine, nursing, public health), and training levels (undergraduate, postgraduate, instructors). The sample size was determined using Cochran’s formula for finite populations at a 95% confidence level with a 5% margin of error, yielding a minimum required sample of 240. The final sample included 250 participants (200 students and 50 instructors) to account for potential non-responses.
Data Collection
Quantitative data was collected using structured selfadministered questionnaire, adapted from the WHO Digital Health Education Competency Framework (2021) and validated tools for low/middle-income country studies [10]. The questionnaire was used to assess various dimensions including demographics, digital literacy (measured on a 5-point Likert scale), informatics exposure in curricula, perceived barriers to implementation, and attitudes toward health informatics. The instrument demonstrated strong internal reliability (α=0.82) following pretesting with 30 participants. Surveys were administered using both paper-based forms for rural institutions and Kobo Toolbox digital platform used for urban respondents, achieving an 89% response rate.
Purposive sampling was used to identify 25 key stakeholders across four categories: policymakers (n=5), educators (n=8), IT specialists (n=7), and development partners (n=5). The data collection involved semi-structured in-depth interviews, exploring national policies on digital health education, institutional readiness for curriculum reform, and lessons from past informatics initiatives. Two focus group discussions with 6-8 participants each were used to examine consensus and divergences in stakeholder perspectives. All qualitative data was audio-recorded with consent, transcribed verbatim, and anonymized to ensure confidentiality.
Data Analysis
Quantitative data analysis was done in SPSS v.28, using descriptive statistics to summarize participant characteristics and key variables. Then chi-square tests and logistic regression were used to examine associations between variables such as informatics training and digital literacy levels. Open-ended survey responses were thematically coded to inform qualitative probes. For qualitative data analysis, the thematic analysis framework in NVivo 12 software was used [12]; progressing through open coding, axial coding (to link themes with quantitative findings), and selective coding to synthesize main themes [13, 14].
Strengths/Limitations
The qualitative methodology was particularly valuable in uncovering policy-related barriers such as fragmented governance structures and funding gaps, technical challenges including unreliable electricity and internet infrastructure, and stakeholder-specific recommendations for improvement. This was used to complement quantitative data by providing deeper contextual understanding of the challenges facing health informatics integration in health educational in Sierra Leone. Although rich contextual data was captured, limitations such as the bias of urban sampling and generalizing questions in lowresource settings existed.
Results & Analysis
Health Informatics Education
Table 1 shows a significant deficit in formal and specialized health informatics training. While foundational computer literacy existed, there was almost complete lack of training in critical modern components of digital health. It indicated that the healthcare system was in the early stage of digital transformation, facing major challenges in implementing effective electronic health systems. General computer class as the most common form of informatics training was offered in 60% of the healthcare institutions. It suggested that most of the institutions recognized the need for digital literacy, a positive start. Such classes generally cover operating systems, word processing, and spreadsheets, which are useful but insufficient for clinical care services. Basic computer skills overlapped with general computer classes, but the lower score (42%) indicated a more focused effort on core skills such as typing and file management rather than broad classes. The fact that it was lower was slightly puzzling, but suggested inconsistency in what was being offered.
Little was done on the other indicators, including dedicated health informatics (13%), EHR training (8%), practical sessions (7%), data privacy and security (0%), and telemedicine protocols (0%). As this forms the backbone of modern health information system, it suggested that key disciplines including improving healthcare delivery through information technology, remote healthcare administration, and patient confidentiality ethics were mostly lacking. As systems become digital, patient data becomes vulnerable to breach and misuse. (Table 1)
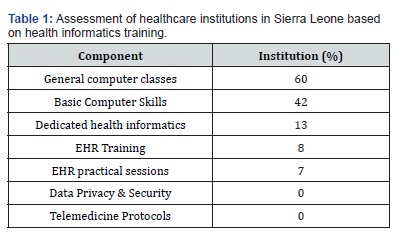
Table 2 further shows that while the healthcare workforce had a modest general digital literacy, it was critically low in proficiency of specialized informatics skills needed for efficient modern healthcare delivery. There was a dramatic decline in competency as the skills became more specific and advanced, indicating a severe training gap with direct impact on healthcare quality and efficiency in the country. General computer use (62%) and basic digital literacy (45%) had the highest rating, much in line with what was observed in Table 1. Most of the workforce possessed foundational skills; a valuable asset and a strong foundation upon which to build more specific skills. However, the drop from general use to digital literacy suggested that competencies like troubleshooting, cloud concept understanding, or more complex software use were weak.
All the other measures of digital literacy in Table 2 are week; including EHR navigation (18%), EHR utilization (12%), data analysis software (9%), health data analytics (8%), telemedicine platforms (12%), and telemedicine applications (3%). The low percentages are a direct consequence of the lack of EHR training (8%) in Table 1. Only a small fraction of health workers can effectively navigate or utilize EHR system, the central nervous system of modern hospitals. This directly translates into inefficiency (where more time is spent on administrative tasks), potential for errors (through incorrect data entry, inability to find patient information), and poor data quality. If data going into the EHR is bad, any attempt at data analysis or digital health innovation will fail. (Table 2)
Urban-Rural Discrepancies
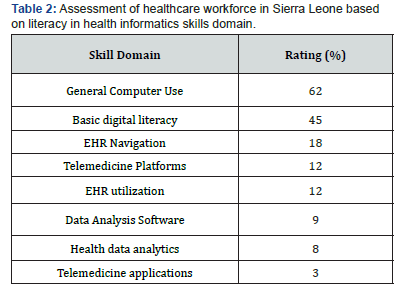
Fig. 1 plots the distribution of key digital health resources between the capital city and the provinces in Sierra Leone; illuminating a critical and profound digital infrastructure divide. This disparity served as a fundamental explanatory factor for the identified deficits in health informatics training and workforce competency, particularly outside the urban center. The data showed a severe inequality, where the capital city of Freetown enjoyed relatively adequate infrastructure and the provincial areas acutely under-resourced. This has created a primary barrier to nationwide digital health advancement.
Analysis of the individual resources highlighted the scale of the challenge. Access to stable power, while a challenge nationwide at 68% in the capital and 57% in the provinces, represented the most basic barrier to operating any digital technology. The presence of a computer lab was one of the most dramatic disparities, with 100% availability in the capital and only 32% in the provinces. This absence of physical tools directly crippled the ability to provide practical training, explaining the low skill acquisition rates. The most extreme gap was in stable internet, reported at 78% in the capital versus a mere 11% in the provinces. This deficiency had a cascading effect, crippling online training initiatives, rendering cloud-based EHRs and telemedicine platforms unusable, and hindering transfer of health data for public health surveillance. Consequently, access to dedicated EHR training tools was almost exclusively limited to the capital city (45%), compared to the virtually nonexistence of it in the provinces (3%). This was directly connected to the abysmal rates of EHR training identified earlier, as effective instruction requires specialized software.
Systemic Barriers
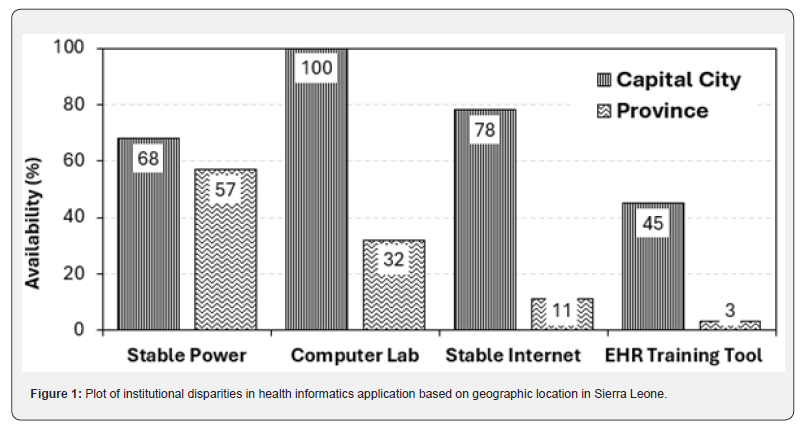
Fig. 2 provides a critical perspective on the mobile technology landscape in Sierra Leone, providing national averages with specific metrics for health training facilities. It showed an environment defined by high mobile penetration but limited internet-based connectivity, with health facilities showing both advantages and surprising deficits. The most striking finding was the nearuniversal adoption of USSD/SMS (unstructured supplementary service data) technology, with a national average of 89% and an even higher 94% within health training facilities. This indicated a robust foundation for basic mobile communication and data exchange. USSD, which enables menu-driven systems without an internet connection. SMS are widely accessible and understood too across the population and the healthcare training sector. This suggested that any digital health strategy seeking broad reach should prioritize these low-tech ubiquitous channels as a primary foundation.
Mobile phone ownership was moderately high nationally (67%) and significantly higher among health training facilities (82%). This was expected as healthcare workers are typically more educated and have greater access to resources. A more telling metric was smartphone prevalence, which was 41% nationally and 58% in health facilities. While this indicates that most of the health workers had access to more advanced devices capable of running applications, it also meant that a significant portion (42%) did not. It created a digital divide within the health sector itself, limiting the universal deployment of app-based solutions.
The data on connectivity revealed the central challenge. Mobile broadband penetration was low nationally (35%) and paradoxically even lower for health training facilities (25%). This suggested that while health workers were more likely to own a smartphone, they were less likely to have a subscribed data plan, potentially due to cost or lack of availability in their specific locations. This made the high rate of daily mobile internet use (33% nationally vs. 63% in health facilities) particularly interesting. It implied that health workers were actively finding ways to access internet, likely relying on Wi-Fi hotspots or purchasing small, daily data bundles when needed. This demonstrated a strong motivation and ability to use online resources despite infrastructural barriers. Finally, the near absence of fixed broadband (8%) nationally and a mere 3% in health training facilities confirmed that the future of digital connectivity in Sierra Leone was outrightly mobile. Reliable, highspeed wired internet was not a feasible cornerstone for national health infrastructure planning. (Figure 2)
Digital Literacy Drivers
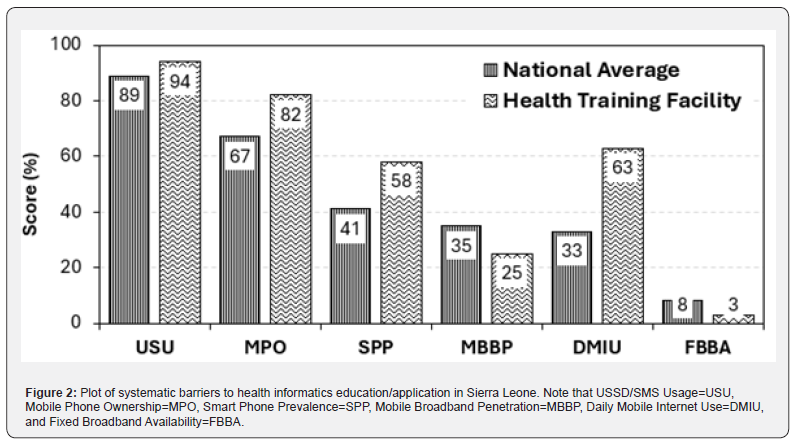
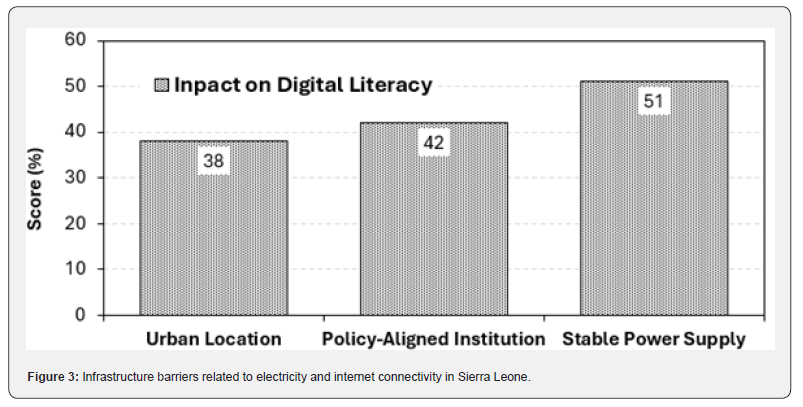
Fig. 3 plots the results of a regression analysis which identified three key factors that significantly influence digital literacy levels, with β (beta) coefficients quantifying the strength and direction of the effect of each factor. The positive values for all the coefficients indicated that each factor had a positive and additive effect on the individual digital literacy scores. The most influential factor was stable power supply, with β coefficient of +0.51. This was the largest effect size, underscoring that reliable electricity was the most fundamental prerequisite for digital literacy. Without consistent power, digital devices cannot be charged, computer labs inoperable, and internet connectivity impossible to maintain. This finding strongly supported infrastructure-first argument, positing that efforts to improve digital skills have limited returns without first addressing this basic infrastructural barrier. It provided a statistical basis for the stark urban-rural divide observed in Fig. 1. Stable power is often concentrated in urban centres.
The second strongest factor was being part of policy-aligned institution, with β= +0.42. This suggested that institutional environment and strategic direction were critical enablers. An institution aligned with national digital health policies was more likely to prioritize digital training, invest in relevant technology, and create a culture that values and fosters digital skills among its staff. This factor highlighted the importance of top-down support, structured curricula, and dedicated resources, moving beyond individual initiative to create a supportive learning ecosystem.
The third factor, urban location, had a positive effect of +0.38. It captured the aggregate advantage of urban settings, which included better access to infrastructure (like stable power and internet), greater availability of training centres, higher exposure to technology in daily life, and larger peer network with digital skills. The coefficient statistically validated the observed digital divide between urban and rural areas (Fig. 1), showing that location itself was a significant determinant of digital literacy outcomes. (Figure 3)
Discussion
There was a massive gap in technology application in clinical workflows, data management, and patient care (Table 1), which made technology investment in the country inefficient or ineffective. Even with installed EHR system, the lack of training results in low adoption, use errors, and staff frustration. It implied that the data within the existing HER could not be complete or reliable, defeating any purpose of investing in digital platform. It highlighted a missed opportunity, especially for a country like Sierra Leone where geography is a barrier to healthcare access. Telemedicine can be used to reach far and beyond to improve healthcare efficiency. Without standardized protocols and training, it is unlikely to implement health informatics safely or effectively.
Proficiency was almost non-existent, which is about going beyond simple data entering to actual generation of insights. The health system was operating without the key tool for evidence-based practice, public health surveillance, and resource management. The ability to track disease outbreaks, measure treatment effectiveness, or manage inventory was severely hampered, which kept the system reactive rather than proactive. There was little familiarity with the concept of telemedicine platform, but practical application was virtually zero. It suggested that the healthcare system was unprepared for remote care service delivery. This limited its resilience (e.g., during outbreaks with risky physical contact like Ebola or COVID-19) and the ability to reach rural or underserved populations. The lack of training in telemedicine protocols (Table 1) directly explained this result. It further suggested that because the institutions were not providing adequate training, especially in specialized areas like EHR, data security, and telemedicine, the workforce lacked the necessary skills for complex digital tasks.
Fig. 1 provided the crucial explanation to what the data showed on training and skills. The inequalities in foundational resources created inequalities in training opportunities, resulting in a workforce that lacked essential health informatics skills. This chain of disparity ultimately culminated in inequalities in the quality and modernity of healthcare delivery, threatening to create a two-tiered health system. The relatively digitized capital city risked becoming increasingly disconnected from the largely analog/paper-based provincial system, further undermining equitable access to healthcare.
The implications of this data are significant. It strongly suggested the need for infrastructure-first strategy, positing that investments in software and training curricula will fail without first addressing the fundamental gaps in electricity, hardware, and connectivity, especially in rural areas. It also underscored the necessity for “offline-first” digital health solutions designed to function with limited or intermittent internet connectivity, ensuring usability in low-resource settings. Furthermore, the high penetration of mobile networks could be leveraged as a strategic bridge, with training and health applications designed for mobile phones offering a potential workaround.
Digital health strategy in Sierra Leones must be mobile-first, but not internet-only. The high USSD/SMS usage and smartphone prevalence without commensurate mobile broadband penetration has created a connectivity paradox. Health workers have the tools (phones) but often lack the consistent and affordable means (data) to use internet-dependent applications. Therefore, a successful strategy must adopt a hybrid approach. For maximum reach and reliability, USSD/SMS systems should be used for critical notifications, data reporting, and patient communication. For more complex tasks, applications should be designed to function offline or with minimal data usage, syncing when a connection is available. The high daily internet use rate showed a workforce eager to leverage digital tools, but the infrastructure and cost models must be addressed to make it sustainable.
The implications for health informatics training and practice were significant. Training programs cannot assume always-on internet connectivity. Curricula must include skills for using offline-capable tools and for working in low-connectivity environments. Furthermore, the widespread use of basic mobile features presented an opportunity to train health workers on using simple SMS-based reporting systems or USSD menus for data collection and patient follow-up, building on an alreadyestablished and familiar technology base.
In conclusion, Fig. 2 moved beyond simply highlighting a digital divide to revealing the specific nature of digital access in Sierra Leone. It argued for a sophisticated, context-specific approach to digital health that prioritizes appropriate technology; leveraging the common USSD/SMS while simultaneously investing in improving mobile internet affordability and access for health workers, for whom it is clearly an essential tool.
Synthesized, the three factors (Fig. 3) pointed to a multi-level framework required to develop digital literacy effectively. The analysis suggested that success depended on a combination of macro-level infrastructure (stable power), meso-level institutional policy (alignment and support), and geo-demographic context (urban advantages). The largest effect coming from stable power confirmed that no amount of policy alignment or urban location can fully compensate for a complete lack of electricity. Conversely, even in an urban area with power, the lack of a supportive institutional policy would likely hinder the organized development of specific digital skills..
The implications for strategy are that interventions must be holistic and simultaneous. Investing in reliable energy infrastructure, particularly in rural areas, was the single most impactful step. This must be backed up with efforts to develop and disseminate clear national digital health policies and to support institutions in aligning training programs and resources with the goals. Finally, specific strategies were needed to mitigate urbanrural gap, such as deploying mobile training labs and satellite internet to extend the benefits of urban centres to provincial facilities.
Fig. 3 moved from describing associations to identifying likely causative factors with measurable impact. It provided robust and quantitative evidence that digital literacy was not merely an individual skill but that it was profoundly shaped by the enabling environment, with stable power as the most critical foundational element.
Conclusion And Recommendations
Conclusion
The integrated analysis suggested that healthcare system in Sierra Leone was at a critical juncture of digital transformation. A key conclusion is that the development of health informatics in the country was severely constrained not by lack of will, but by profound and multi-layered digital divide. This divide manifested in three interconnected dimensions infrastructure, skills, and geographic equity. The near-absence of training in critical areas like EHR utilization, data privacy, and telemedicine protocols indicated that the healthcare workforce was unprepared for modern data-driven care delivery. This skills deficit was a direct consequence of institutional training gaps, where fewer than 10% of the institutions offered practical EHR sessions with none providing data security training.
The root cause of these training and skills shortages was the stark infrastructural chasm, most acutely felt between the capital city and provincial areas. While all capital city institutions (100%) had computer labs, only 32% had these labs in the provinces. Stable internet availability was also 78% in the capital as against 11% in the provinces. The extreme disparity in resources created an insurmountable barrier for equitable education. The urbanrural divide threatened to create a two-tiered health system, undermining equitable access to quality care. Regression analysis quantitatively confirmed that foundational issues like stable power supply (β=+0.51) and supportive institutional policies (β=+0.42) were the most significant predictors of digital literacy, even more so than urban location (β=+0.38). Policy alignment and stable power supply were respectively 1.1 and 1.3 times more impactful for health informatics education than geographical location. This underscored that without first addressing these foundational enablers, efforts to enhance skills will remain fragmented and ineffective.
Paradoxically, a significant opportunity existed within this challenge. Sierra Leone has a robust and ubiquitous mobile phone culture, with USSD/SMS usage at 89% nationally and 94% among health training facilities. This high penetration of basic mobile technology, coupled with a strong motivation for digital engagement with 63% of the health workers using mobile internet daily (despite low broadband penetration), provided a unique foundation. It indicated that the workforce was not technophobic but instead constrained by lack of access to appropriate, contextspecific tools and training. Therefore, the path forward required a fundamental shift in strategy away from importing highresource, internet-dependent digital health models and towards a pragmatic, hybrid approach that leverages existing strengths while systematically building capacity.
Recommendations
To address these challenges, a multi-layered and sequential strategy is imperative. The primary and most critical recommendation is to adopt an infrastructure-first investment strategy. National and international resources must be prioritized to provide reliable off-grid power solutions such as solar energy to provincial healthcare and training facilities. Concurrently, expanding internet connectivity through innovative solutions like satellite-based services is essential to bridge the connectivity gap. This foundational step is not substitutable; without stable power and connectivity, all other interventions will fail to achieve scale and sustainability.
The second step is the deployment of the educational curricula and technology to embrace a hybrid mobile-first approach. Training programs and digital health tools should be designed to function effectively in low-connectivity environments. This involves leveraging high USSD/SMS penetration for critical alerts, data reporting, and patient follow-up, while developing smartphone applications that are optimized for offline use, syncing data only when a connection is available. Training should pivot to include competencies in using these low-data technologies, ensuring that skills are relevant and immediately applicable in the resource-constrained environments where most health workers operate.
Third, a deliberate effort to build human and institutional capacity is required. This involves creating a standardized national health informatics curriculum that moves beyond basic computer literacy to include EHR navigation, data privacy principles, and use of data for decision support. Furthermore, well-resourced institutions in the capital should be leveraged as centres of excellence and central training hubs to host intensive residential training for provincial staff. To address the immediate hardware gap, investing in mobile computer labs that can tour provincial facilities can provide crucial hands-on experience.
Finally, these efforts should be unified under a cohesive national policy and advocacy framework. The positive effect of policy alignment demonstrates the need for strong governance. A clear national digital health strategy should be developed, outlining standards for data privacy, interoperability, and technology procurement. This policy must explicitly aim to mitigate the urban-rural divide, directing resources and incentives to ensure equitable development. By building from the foundation of infrastructure, tailoring solutions to the mobile reality, investing in people, and guiding the effort with strong policy, Sierra Leone can overcome its current constraints and harness digital tools to build a more resilient, efficient, and equitable healthcare system for all.
Acknowledgement
I wish to thank my supervisors for their expert guidance and support during this project. I am also grateful to my colleagues in my department and university for their helpful discussions and feedback. I would also like to acknowledge the foundational work of the researchers in this field, which provided the essential groundwork for this study. Finally, thank you to the anonymous reviewers for their invaluable comments.
References
- World Health Organization (WHO) (2023) Universal Health Coverage Global Monitoring Report. Geneva: WHO.
- UNICEF (2022) The State of the World’s Children 2022: On my mind-Promoting, protecting and caring for children’s mental health. UNICEF.
- The World Bank (2023) World Development Report 2023: Migrants, Refugees, and Societies. World Bank Group.
- Ministry of Health and Sanitation (MOHS) (2021) National Health Sector Strategic Plan. Freetown: GovSL.
- Shortliffe EH, Cimino JJ (Eds) (2021) Biomedical informatics: Computer applications in health care and biomedicine (5th ed.). Springer Nature.
- Mehl G, Labrique A, Vasudevan L, Berg M (2020) Digital health innovation for sustainable development: A review of the evidence. The Lancet Digital Health 2(8): 408-416.
- Binagwaho A, Scott KW, Dushime T (2019) Telemedicine as a tool for equity in Rwanda: A narrative review. Journal of Medical Internet Research 21(4).
- Amoakoh HB, Adu Gyamfi RS, Amoakoh KA, Sarpong E, Agyepong IA, et al. (2022) Effect of a mobile clinical decision support system on the management of malaria in children under 5 years in Ghana: A cluster-randomised controlled trial. BMJ Global Health 7(3).
- Kamara MB, Sesay AI, Bangura ST (2023) Barriers to integrating digital health technologies in medical and nursing education in Sierra Leone: A qualitative multi-stakeholder analysis. BMC Medical Education 23(1): 145.
- Fatehi F, Menon A, Bird D (2020) Digital health in low and middle-income countries: Progress and challenges. The Lancet Digital Health 2(6): 298-300.
- Creswell JW, Plano Clark VL (2018) Designing and Conducting Mixed Methods Research. Sage Pp: 1-520.
- Braun V, Clarke V (2006) Using Thematic Analysis in Psychology. Qualitative Research in Psychology 3(2).
- Ministry of Health (MOHS) (2022) Sierra Leone Health Informatics Audit. Freetown: MOHS.
- World Health Organization (WHO) (2021) Digital Health Education Competency Framework. Geneva: WHO.






























