Abstract
Background: Lifestyle behaviors such as diet, physical activity, sleep, stress management, social connection, and substance use are major determinants of chronic disease and overall well-being. Despite strong evidence supporting their role in health, practical tools to assess these behaviors efficiently and holistically are limited.
Objective: This paper describes the development and application of six brief health screeners referred to as lifestyle vital signs that address the core pillars of lifestyle medicine: food quality, physical activity, sleep quality, coping habits, social connections, and substance use.
Methods: Guided by public health guidelines, behavioral science frameworks, and plain language principles, each screener was designed to be completed in under three minutes. The tools support self-assessment, personalized feedback, and brief intervention across a range of settings. The development process emphasized clarity, accessibility, and alignment with theoretical models such as the Health Belief Model, Transtheoretical Model, Self-Determination Theory, and the Social Ecological Model.
Results: Each screener includes behaviorally specific items that reflect evidence-based recommendations and key health determinants. The tools were written at a readability level suitable for public-facing use and designed to facilitate health literacy and engagement. Applications include use in primary care, community outreach, health education, and digital platforms.
Conclusion: These brief, user-friendly screeners offer a scalable and accessible approach to embedding lifestyle medicine into public health practice. Their adoption can improve lifestyle risk assessment, guide behavior changes conversations, and support efforts to reduce health disparities and promote whole-person care. Future research will focus on validating these tools and evaluating their impact on individual and population health outcomes.
Keywords: Health screeners; Lifestyle vital signs; Health behavior assessment; Behavior change; Substance use; Health literacy; Health risk screening
Abbreviations: FQS: Food Quality Screener; AHEI: Alternative Healthy Eating Index; PAS: Physical Activity Screener; SQS: Sleep Quality Screener; CHS: Coping Habits Screener; SUS: Substance Use Screener; SCS: Social Connections Screener
Background and Introduction
The field of lifestyle medicine has grown significantly over the past two decades, evolving from a clinical niche into a global movement that uses of evidence-based behavioral interventions to prevent, treat, and even reverse chronic diseases. As Lippman et al. [1] noted, lifestyle medicine focuses on six core pillars: nutrition, physical activity, restorative sleep, stress management, social connection, and avoidance of risky substances. These pillars are supported by a growing evidence base, and an international infrastructure aimed at integrating lifestyle approaches into health systems worldwide.
The six-lifestyle medicine vital signs food quality, physical activity, sleep quality, coping habits, social connections, and substance use represent powerful, modifiable factors that shape health across the lifespan. Unlike traditional vital signs, such as heart rate or blood pressure, these behavioral indicators reflect everyday habits that are directly linked to the leading causes of chronic disease and premature mortality [2,3]. Substantial evidence shows that lifestyle-related behaviors account for a large proportion of preventable mortality and chronic disease burden in the United States and globally [4,5].
Incorporating lifestyle vital signs into clinical, educational, and public health practice supports a proactive, whole-person approach to disease prevention and health promotion. Low diet quality, physical inactivity, and poor sleep quality are major contributors to obesity, type 2 diabetes, cardiovascular disease, and certain cancers [6,7]. Likewise, chronic stress, social isolation, and substance use are increasingly recognized as contributors to mental health disorders, substance-related harm, and increased healthcare costs [8,9]. Addressing these behavioral risk factors is essential to achieving health equity and reducing disparities.
Despite growing awareness of the six pillars, practical tools to assess these behaviors in an integrated, efficient, and accessible way remain limited. Existing screeners often focus on individual behaviors (e.g., physical activity or diet) and rarely account for the full range of lifestyle factors that influence chronic disease risk and overall well-being [3,2]. Even fewer tools are designed for rapid use in real-world settings, grounded in behavioral theory, or written in plain language to support health literacy.
To address this gap, we developed six brief lifestyle screeners guided by four key principles for effective lifestyle assessment tools:
1. Tools should support both assessment and behavior change.
2. Tools should be brief ideally under three minutes.
3. Tools should be grounded in public health guidelines and behavioral theory.
4. Tools should be written in plain language to enhance accessibility.
Without brief, user-friendly screeners, healthcare professionals and educators miss valuable opportunities to assess lifestyle behaviors holistically, engage in brief interventions, or track progress over time. Quick-to-complete tools can improve patient engagement, guide health goals, and support population-level surveillance of behavioral risks [10]. These tools also align with national goals like the Healthy People 2030 objective on organizational health literacy, which calls on systems to ensure that individuals can understand and use health information [11]. This paper describes the development and application of six brief lifestyle screeners aligned with lifestyle medicine principles. Each screener reflects public health priorities, incorporates behavioral theory, and is designed for real-world use. Together, they represent a scalable strategy to embed lifestyle medicine into clinical care, education, and community health practice.
Food Quality Screener
The Food Quality Screener (FQS) consists of 11 items mainly adapted from the Alternative Healthy Eating Index (AHEI) index categories; a validated dietary quality scoring system associated with lower risk of chronic disease and premature mortality (Table 1) [12]. Items 1-6 assess consumption of high-quality, nutrient-dense foods: vegetables (excluding potatoes), fruits (excluding juice), whole grains, nuts/seeds, legumes, and fish. These foods are emphasized in the AHEI and linked to reduced risk for cardiovascular disease, type 2 diabetes, and certain cancers due to their fiber, antioxidant, and healthy fat content [13,14].
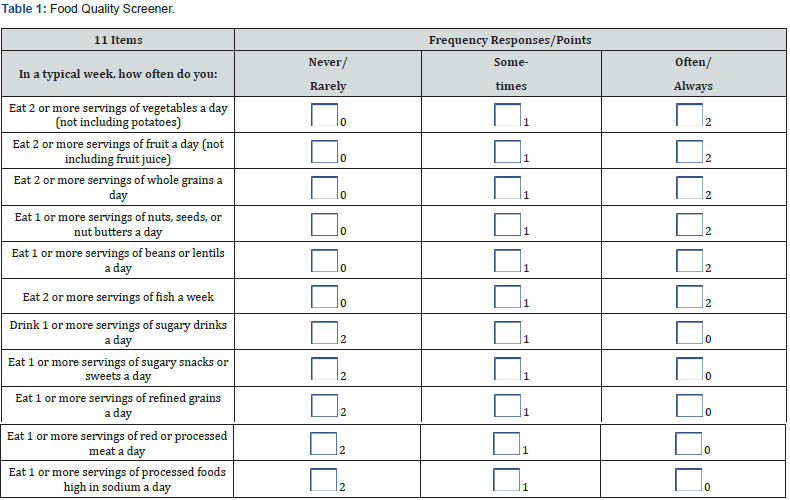
Items 7-11 assess consumption of lower-quality foods andbeverages, including sugary drinks (item 7), sugary snacks (item 8), and refined grains (item 9). Frequent intake of sugar-sweetened beverages, red/processed meats, and refined snacks has been associated with systemic inflammation, insulin resistance, and increased mortality risk [15,16]. Items 10 and 11 assess red or processed meat and processed foods high in salt, both of which are known contributors to hypertension, and overall dietary risk when consumed in excess [17,18]. Reverse scoring is used for lower quality items 7-11 to ensure that higher total scores reflect an unhealthy dietary pattern. Together, these 11 items provide a practical, behaviorally specific overview of diet quality, supporting awareness, self-reflection, and brief nutritional counseling.
The FQS is concise and easy to complete in under three minutes. It includes 11 plain language questions and uses a three-point response format. Clear examples (e.g., “oats, brown rice,” “soda,” “candy”) help users recognize food choices in their everyday lives. This brief, user-friendly format allows for implementation in primary care clinics and community settings [19,20]. The tool also draws on principles from the Transtheoretical Model, encouraging users to consider readiness for change with questions like “Are you ready to change an eating habit in the next month?” [21]. Additionally, its emphasis on choice and small, incremental improvements aligns with Self-Determination Theory, promoting autonomy and confidence in making healthy food decisions [22]. Finally, the tool uses plain language to enhance health literacy and inclusivity. Questions are framed in accessible terms, and the feedback section offers supportive messages like “One change at a time” and “A small change can have a big impact on your health.” It also acknowledges individual variability in dietary needs and preferences, reinforcing that there is no one-size-fits-all eating pattern an approach that supports both health equity and cultural relevance [23,24].
Physical Activity Screener
The Physical Activity Screener (PAS) includes seven items that assess the frequency, variety, and balance of movement behaviors aligned with national guidelines and evidence-based recommendations (Table 2). The first two items measure engagement in aerobic activity (e.g., brisk walking, jogging) for at least 2½ hours per week (Item 1) and muscle-strengthening activities (e.g., squats, lifting weights) at least twice weekly (Item 2). These recommendations reflect the Physical Activity Guidelines for Americans, which emphasize the health benefits of both aerobic and resistance exercise for cardiovascular, metabolic, and musculoskeletal health [25]. Items 3 and 4 focus on flexibility and balance training, respectively often overlooked yet vital components of functional fitness, fall prevention, and injury reduction, especially for older adults [26]. Item 5 assesses participation in light-intensity physical activity (e.g., housework, yardwork, standing tasks) for three or more hours per day, recognizing the cumulative health benefits of non-exercise movement throughout the day [27]. Items 6 and 7 address sedentary behavior, specifically sitting less than eight hours per day and breaking up sitting every 30 minutes with movement. These items reflect emerging evidence on the health risks of prolonged sedentary time, independent of moderate-to-vigorous physical activity [28]. By encompassing a range of intensities and movement domains, the screener provides a comprehensive, behaviorally specific profile of physical activity and inactivity.
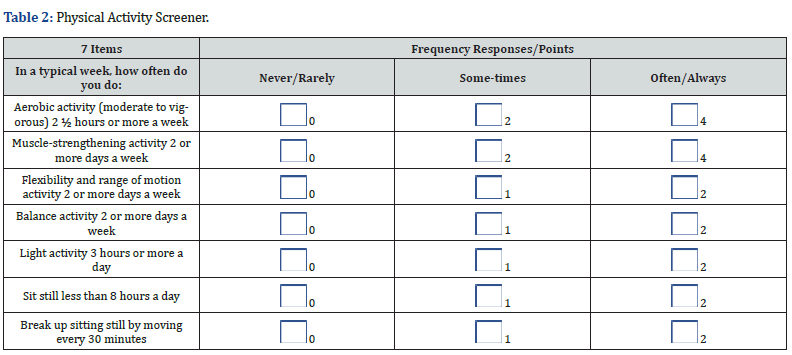
The PAS can be completed in under three minutes. It uses a simple three-point response scale and includes concrete examples (e.g., “brisk walking,” “stretching,” “housework”) to enhance usability across diverse literacy levels. The low burden makes it appropriate for clinics and community screenings [29]. The screener also reflects behavioral constructs from the Social Ecological Model, recognizing that movement is shaped by individual, environmental, and social contexts [30]. In addition, its emphasis on autonomy, variety, and enjoyment is consistent with Self-Determination Theory, which supports sustainable, self-directed behavior change [22]. Finally, the tool emphasizes plain language to improve accessibility and engagement. Terms like “sit still less,” “move every 30 minutes,” and “activities you enjoy” are clear, conversational, and motivating. The tool avoids technical jargon and uses an encouraging message “Moving Matters” to affirm that all movement counts and that small steps can make a meaningful impact on physical and mental well-being [20,11].
Sleep Quality Screener
The Sleep Quality Screener (SQS) includes eight items that assess essential components of healthy sleep behavior (Table 3). Items 1 and 2 focus on sleep onset and continuity specifically, falling asleep within 30 minutes and sleeping through the night without prolonged awakenings. These are fundamental indicators of sleep efficiency and are often used in clinical and research settings to evaluate sleep disorders and disturbances [31,32]. Item 3 assesses sleep duration, asking whether individuals typically get 7 to 9 hours of sleep per night, consistent with national sleep guidelines for adults [33,34]. Items 4 through 6 evaluate sleep hygiene practices, including maintaining a consistent sleep-wake schedule, limiting bed use to sleep and sex, and creating a quiet, dark sleep environment. These behaviors are associated with improved circadian regulation and reduced sleep latency [35]. Items 7 and 8 capture subjective sleep quality and daytime functioning, asking whether individuals feel rested upon waking and whether they feel alert and able to focus during the day. These items reflect restorative sleep and are closely linked to cognitive performance, mood, and overall health [36,32]. Collectively, the screener provides a concise, behaviorally anchored assessment of sleep quality that supports both self-awareness and brief intervention.
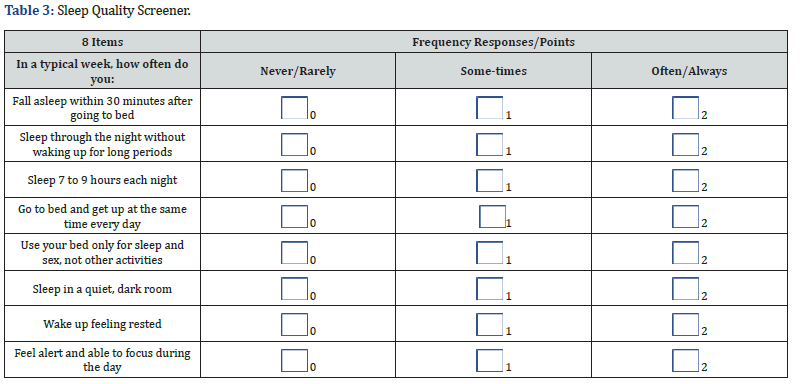
The SQS is quick and easy to administer. With only eight plain language questions and a simple scoring system, it can be completed in under three minutes. Its low burden makes it suitable for community health settings and clinic waiting rooms where time is limited and user engagement is critical [19]. The SQS is grounded in both public health guidance and behavioral theory. It reflects evidence-based sleep recommendations from the Centers for Disease Control and Prevention [37] and the American Academy of Sleep Medicine [33]. In addition, the design aligns with principles of the Health Belief Model by helping individuals assess perceived susceptibility and benefits and Self-Determination Theory, by promoting autonomy and internal motivation through self-assessment and personalized feedback [38,22]. Finally, the screener is intentionally written in plain language to enhance health literacy. Each item uses everyday terms (e.g., “fall asleep,” “wake up rested,” “quiet, dark room”) to ensure broad accessibility. The instructions, scoring guide, and brief educational message (“Sleep Quality Matters”) further support user understanding, empowering individuals to recognize the importance of sleep and consider manageable steps toward improvement [20,24].
Coping Habits Screener
The Coping Habits Screener (CHS) includes 13 items that assess a range of strategies individuals use to manage stress in everyday life (Table 4). The first ten items reflect adaptive coping behaviors that are commonly associated with improved mental health and resilience. Items 1-3 assess cognitive coping, such as identifying stressors (“figure out what’s making me feel stressed”), problem-solving (“solve problems step by step”), and learning from difficult experiences all of which are central to cognitive-behavioral models of stress management [39,40]. Items 4–6 represent emotion-focused coping strategies, including using humor, seeking social support, and engaging in calming activities like prayer or music, which are linked to improved mood and emotional regulation [41,42]. Items 7-10 emphasize self-care behaviors taking breaks, moving the body, eating healthy foods, and getting adequate sleep that contribute to stress recovery and overall well-being [43,44]. In contrast, Items 11-13 reflect maladaptive coping patterns, such as self-blame, avoidance, and using substances to manage stress. These responses are reverse scored, as they are associated with negative outcomes including increased anxiety, depression, and substance misuse [45,46]. By including both adaptive and maladaptive strategies, the screener supports a balanced, behaviorally specific assessment of coping habits. It encourages reflection on which responses may be helpful, and which might signal a need for additional support or skill development.
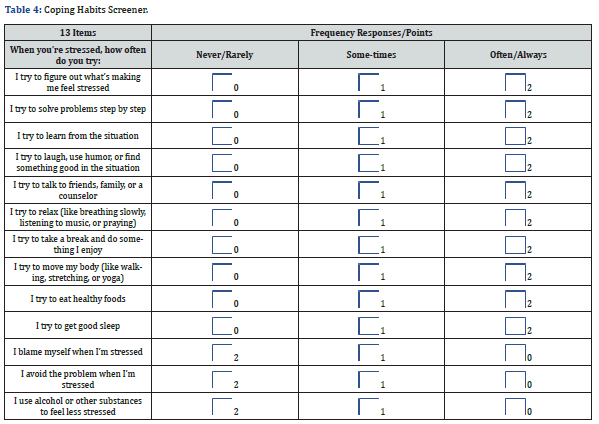
The CHS is quick and easy to administer, taking approximately three minutes to complete. The 13 plain language items employ a simple three-point scale and user-friendly scoring instructions. This low-burden format makes the tool well-suited for use in health education, clinical settings, or community outreach programs, especially where time or literacy may be barriers [19,20]. The CHS is informed by public health guidelines and psychological theory. It draws upon validated principles from Cognitive Behavioral Therapy (CBT), which emphasizes identifying and modifying unhelpful coping patterns, and Lazarus and Folkman’s Transactional Model of Stress and Coping, which highlights the importance of cognitive appraisal and adaptive responses [39,40]. It also aligns with Self-Determination Theory by encouraging users to reflect on intrinsic motivation and autonomy in how they manage stress [22]. The inclusion of both approach-based strategies (e.g., problem solving, seeking support) and avoidant strategies (e.g., substance use, self-blame) enables a well-rounded reflection of coping habits. Finally, the screener prioritizes plain language and health literacy. Each item uses accessible vocabulary and relatable examples (e.g., “talk to friends,” “move my body,” “eat healthy foods”), and the brief explanatory message (“Coping Habits Matter”) reinforces the importance of managing stress in a supportive tone. The screener avoids medical jargon and helps users recognize behaviors they can build on or modify to improve resilience and emotional health [24,11].
Social Connections Screener
The Social Connections Screener (SCS) includes eight core items that assess the presence, quality, and effects of social relationships in everyday life (Table 5). The first two items evaluate social engagement the frequency of contact with friends or family (Item 1) and participation in community activities such as volunteering or gatherings (Item 2). These behaviors reflect involvement in both personal and community-level networks, which are associated with stronger support systems and improved well-being [47,48]. Items 3 and 4 assess the quality of close relationships, asking whether individuals feel emotionally connected to others (Item 3) and whether they can trust the people closest to them (Item 4). These aspects are key indicators of perceived social support, a known protective factor for mental and physical health [49]. Items 5 and 6 address functional support, measuring whether individuals have someone to confide in during distress (Item 5) and someone who can provide instrumental assistance, such as help with errands or transportation (Item 6). These types of support emotional and tangible have been shown to buffer the effects of stress and reduce risk for depression and chronic disease [50]. Item 7 captures reciprocity, assessing whether the respondent helps others when needed. Giving support can enhance feelings of purpose and belonging, reinforcing mutual social bonds [51]. Finally, Items 8 and 9 identify negative social experiences, including feelings of loneliness or exclusion (Item 8) and social interactions that increase distress (Item 9). These items are reverse scored to capture social strain, which has been independently linked to poorer health outcomes [52]. Together, the items provide a brief yet comprehensive overview of both protective and risk-related dimensions of social connectedness.
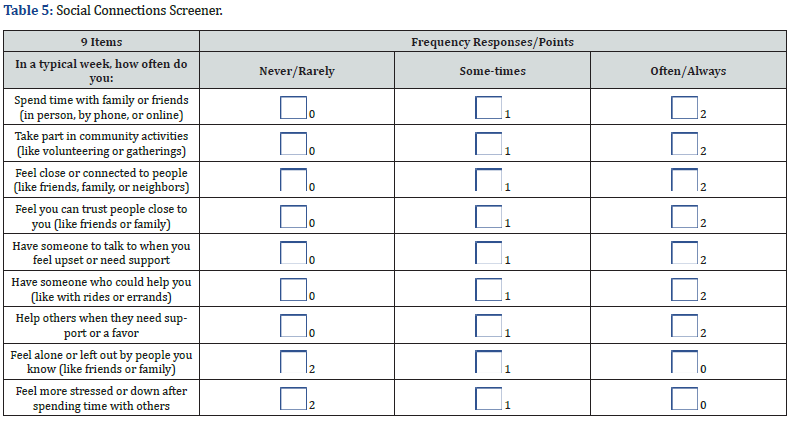
The SCS is quick and simple to administer. It includes nine clearly worded questions, each using a three-point scale, and can be completed in under three minutes. Its ease of use allows for integration into brief clinical encounters, community screenings, or educational programs without imposing significant time burdens on users or facilitators [19]. The SCS is grounded in both public health priorities and theoretical frameworks. It draws upon the Social Ecological Model, recognizing that social support occurs at multiple levels individual, interpersonal, community, and societal [53]. It also reflects constructs from Self-Determination Theory, including relatedness, which emphasizes the fundamental human need to feel connected and valued by others [22]. The screener is consistent with the CDC’s emphasis on social connectedness as a protective factor for mental health, chronic disease prevention, and longevity [54]. Finally, the tool is written in plain language to enhance health literacy and accessibility. Each item uses everyday terms (e.g., “spend time,” “help others,” “feel left out”) and avoids clinical jargon. The brief educational message “Social Connections Matter” reinforces the importance of relationships in a user-friendly tone. These strategies support understanding, reflection, and behavior change, especially among populations with varying literacy levels [23,24].
Substance Use Screener
The Substance Use Screener (SUS) consists of eight items that assess patterns and contexts of alcohol, nicotine, cannabis, and medication use (Table 6). Items 1-4 focus on the frequency and type of substance use, including drinking more than one alcoholic drink per day (Item 1), using tobacco or nicotine (Item 2), using marijuana in any form (Item 3), and using prescription medications in ways other than prescribed (Item 4). These behaviors reflect commonly misused substances and align with established risk indicators for substance-related harm [55,56]. Item 1’s alcohol threshold also mirrors guidance from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), which defines low-risk drinking limits based on daily and weekly intake [57]. Items 5-8 examine situational and functional use, including using substances to cope with stress (Item 5), before engaging in potentially dangerous activities like driving or working (Item 6), to manage negative emotions such as sadness or boredom (Item 7), or continuing use despite adverse consequences at home or work (Item 8). These questions capture behavioral patterns associated with problematic substance use and align with criteria found in validated screening tools such as the ASSIST and the AUDIT [58,59]. They also reflect core elements of the Transtheoretical Model, which emphasizes identifying risk behaviors and raising awareness as precursors to behavior change [21]. Collectively, the screener enables brief risk stratification across substance types and contexts, supporting early identification and referral using evidence-based models like SBIRT [60].
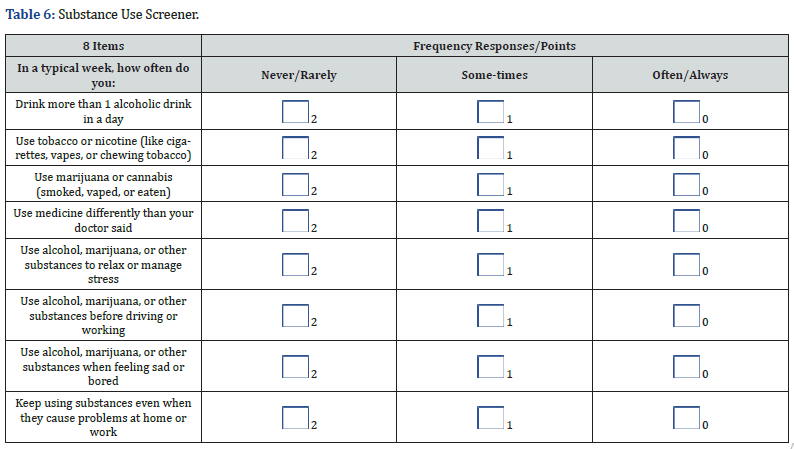
The SUS is brief and easy to complete in under three minutes. With eight yes-or-no-style questions framed on a three-point scale, the screener minimizes complexity and respondent burden. This makes it suitable for use in clinics, counseling centers, and community settings where time, stigma, and literacy may otherwise pose barriers to candid discussion [19,59]. The screener is informed by public health guidelines and behavior change theory. It aligns with principles from Screening, Brief Intervention, and Referral to Treatment (SBIRT), an evidence-based model for identifying and addressing risky substance use [61]. In addition, the structure and messaging reflect constructs from the Transtheoretical Model, encouraging individuals to move through contemplation and preparation stages toward behavior change [21]. The emphasis on awareness and non-judgmental self-assessment also supports Self-Determination Theory by encouraging autonomy and intrinsic motivation for change [22]. Finally, the screener uses plain language to enhance health literacy and reduce stigma. Questions avoid clinical or diagnostic terms and instead use accessible phrases like “use medicine differently than your doctor said” or “use substances to relax or manage stress.” The message “Substance Use Matters” highlights the relevance of this topic to mental, physical, and relational well-being in a supportive tone. Together, these strategies promote honest self-reflection and readiness for change, particularly among individuals who may not otherwise engage with traditional screening tools [23,24].
Conclusion
As chronic disease rates continue to rise, there is an urgent need to prioritize prevention and promote health through modifi- able lifestyle behaviors. This manuscript introduced six brief, the- ory-informed screeners centered on food quality, physical activity, sleep quality, coping habits, social connections, and substance use that reflect the core pillars of lifestyle medicine. These lifestyle vital signs offer a practical and scalable way to assess everyday behaviors that influence long-term health and well-being.
Each screener was developed using public health guidelines, behavioral science frameworks, and plain language principles to ensure accessibility, scientific rigor, and ease of use. Designed to be completed in under three minutes, these tools support brief intervention, personalized feedback, and integration into a wide range of clinical, educational, and community settings. By facilitat- ing conversations around lifestyle habits, these screeners empow- er individuals to engage in their health and help organizations track population-level trends.
Widespread adoption of these tools could enhance efforts to address health disparities, improve health literacy, and support whole-person care. Our future research will focus on validating the screeners across diverse populations, integrating them into electronic health records, and exploring their impact on behavior change, clinical outcomes, and health system performance. Embedding lifestyle vital signs into routine practice represents a meaningful step toward a more proactive, equitable, and prevention-focused model of care.
References
- Lippman D, Stump, M, Veazey E, Guimaraes ST, Rosenfeld R, et al. (2024) Foundations of lifestyle medicine and its evolution. Mayo Clin Proceed (1): 97-111.
- Ford ES, Bergmann MM, Kröger J, Schienkiewitz A, Weikert C, et al. (2009) Healthy living is the best revenge: findings from the European Perspective Investigation into Cancer and Nutrition-Potsdam study. Arch Intern Med 169(15): 1355-1362.
- Katz DL, Frates EP, Bonnet JP, Gupta SK, Vartiainen E, et al. (2018) Lifestyle as medicine: The case for a true health initiative. Am J Health Promot 32(6): 1452-1458.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States, 2000. JAMA 291(10): 1238-1245.
- World Health Organization (2022) Noncommunicable diseases country profiles 2022. Geneva: WHO.
- Centers for Disease Control and Prevention (2022) Chronic Diseases in America. Atlanta: U.S. Department of Health and Human Services.
- Itani O, Jike M, Watanabe N, Kaneita Y (2017) Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med 32: 246-256.
- Holt Lunstad J (2022) Social connection as a public health issue: The evidence and a systemic framework for prioritizing the ‘social’ in social determinants of health. Annu Rev Public Health 43: 193-213.
- National Academies of Sciences, Engineering, and Medicine. The Social and Behavioral Sciences in K-12 Education: Past, Present, and Future. Washington, DC: The National Academies Press 2021.
- Krist AH, Davidson KW, Ngo Metzger Q, Mills J, Kusnoor SV (2020) Primary care practice facilitation for implementation of evidence-based prevention interventions: a case study. J Gen Intern Med 35(Suppl 2): 558-564.
- Office of Disease Prevention and Health Promotion. Healthy People 2030: Organizational Health Literacy. U.S. Department of Health and Human Services 2020.
- Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML et al. (2012) Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 142(6): 1009-1018.
- Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, et al. (2017) Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol 70(4): 411-422.
- Willett WC, Rockström J, Loken B, Springmann M, Lang T, et al. (2019) Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet 393(10170): 447-492.
- Schwingshackl L, Hoffmann G, Iqbal K, Schwedhelm C, Boeing H (2017) Food groups and intermediate disease markers: a systematic review and network meta-analysis of randomized trials. Am J Clin Nutr 105(6): 1462-1473.
- Malik VS, Popkin BM, Bray GA, Després JP, Hu FB (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care 33(11): 2477-2483.
- Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB (2011) Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 364(25): 2392-2404.
- Orlando EA, Rebellato AP, Silva JG, Andrade GC, Pallone JA (2020) Sodium in different processed and packaged foods: Method validation and an estimative on the consumption. Food Res Int 129(2): 111-121.
- Frates EP, Moore MA, Lopez CF, McCartney N (2021) Lifestyle medicine: a brief review of its dramatic impact on health and survival. Am J Lifestyle Med 15(5): 579-589.
- Baur C, Prue C (2014) The CDC Clear Communication Index is a new evidence-based tool to prepare and review public communication products. Health Promot Pract 15(5): 629-637.
- Prochaska JO, Velicer WF (1997) The Transtheoretical Model of health behavior change. Am J Health Promot 12(1): 38-48.
- Deci EL, Ryan RM (2000) The ‘what’ and ‘why’ of goal pursuits: Human needs and the self-determination of behavior. Psychol Inq 11(4): 227-268.
- Stableford S, Mettger W (2007) Plain language: a strategic response to the health literacy challenge. J Public Health Policy 28(1):71-93.
- S. Department of Health and Human Services (2010) National Action Plan to Improve Health Literacy. Washington, DC: USDHHS.
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, et al. (2018) The Physical Activity Guidelines for Americans. JAMA 320(19): 2020-2028.
- Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, et al. (2019) Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019(1): 1-452.
- Ekelund U, Tarp J, Steene Johannessen J, Hansen BH, Jefferis B, et al. (2019) Dose-response associations between accelerometry measured physical activity and sedentary time and all-cause mortality: systematic review and harmonized meta-analysis. BMJ 366: l-10.
- Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, et al. (2017) Sedentary Behavior Research Network (SBRN)-Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act 14(1): 14-75.
- Bennie JA, Pedisic Z, van Uffelen JG, Gale J, Banting LK, et al. (2016) The descriptive epidemiology of total physical activity, muscle-strengthening exercises and sedentary behavior among Australian adults results from the National Nutrition and Physical Activity Survey. BMC Public Health 16(1): 1-13.
- Sallis JF, Owen N, Fisher EB (2008) Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior: Theory, Research, and Practice. 4th San Francisco: Jossey-Bass Pp: 465-485.
- Ohayon MM, Wickwire EM, Hirshkowitz M, Albert SM, Avidan A, et al. (2017) National Sleep Foundation's sleep quality recommendations: first report. Sleep Health 3(1): 6-19.
- Buysse DJ (2014) Sleep health: can we define it? Does it matter? Sleep 37(1): 9-17.
- Watson NF, Martin JL, Wise MS, Carden KA, Curhan GC, et al. (2015) Delaying middle school and high school start times is a key factor in reducing adolescent sleep deprivation. J Clin Sleep Med 11(10): 1215-1217.
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, et al. (2015) National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health 1(1): 40-43.
- Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH (2015) The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev 22: 23-36.
- Medic G, Wille M, Hemels ME (2017) Short and long-term health consequences of sleep disruption. Nat Sci Sleep 9: 151-161.
- Centers for Disease Control and Prevention (2017) Sleep and Sleep Disorders. Atlanta, GA: CDC.
- Glanz K, Rimer BK, Viswanath K (2015) Health Behavior: Theory, Research, and Practice. 5th San Francisco: Jossey-Bass Pp: 1-512.
- Lazarus RS, Folkman S (1984) Stress, Appraisal, and Coping. New York: Springer.
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A (2012) The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognit Ther Res 36(5): 427-440.
- Folkman S, Moskowitz JT (2004) Coping: pitfalls and promise. Annu Rev Psychol 55: 745-774.
- Carver CS (1997) You want to measure coping but your protocol’s too long: Consider the Brief COPE. Int J Behav Med 4(1): 92-100.
- Chida Y, Steptoe A (2008) Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med 70(7): 741-756.
- Pressman SD, Jenkins BN, Kraft Feil TL (2014) Positive emotions and health: the role of affect as both a determinant and an outcome of physical health. In: Huppert FA, Cooper CL, eds. Wellbeing: A Complete Reference Guide. Chichester: Wiley Blackwell Pp: 1-28.
- Aldwin CM (2007) Stress, Coping, and Development: An Integrative Perspective. 2nd New York: Guilford Press.
- Hyman SM, Sinha R (2009) Stress-related factors in cannabis use and misuse: implications for prevention and treatment. J Subst Abuse Treat 36(4): 400-413.
- Berkman LF, Glass T, Brissette I, Seeman TE (2000) From social integration to health: Durkheim in the new millennium. Soc Sci Med 51(6): 843-857.
- Umberson D, Montez JK (2010) Social relationships and health: a flashpoint for health policy. J Health Soc Behav 51(Suppl): 54-66.
- Holt Lunstad J, Smith TB, Baker M, Harris T, Stephenson D (2015) Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 10(2): 227-237.
- Thoits PA (2011) Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav 52(2): 145-161.
- Brown SL, Brown RM (2015) Connecting prosocial behavior to improved physical health: contributions from the neurobiology of parenting. Neurosci Biobehav Rev 55: 1-17.
- Lincoln KD (2000) Social support, negative social interactions, and psychological well-being. Soc Serv Rev 74(2): 231-252.
- McLeroy KR, Bibeau D, Steckler A, Glanz K (1988) An ecological perspective on health promotion programs. Health Educ Q 15(4): 351-377.
- Centers for Disease Control and Prevention (2023) Social Connectedness and Health. Atlanta, GA: CDC.
- Substance Abuse and Mental Health Services Administration (2019) Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Rockville, MD: SAMHSA.
- National Institute on Drug Abuse (2020) Commonly Used Drugs Charts. Bethesda, MD: NIDA.
- National Institute on Alcohol Abuse and Alcoholism (2021) Alcohol facts and statistics. Bethesda, MD: NIAAA.
- World Health Organization (2010) The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care. Geneva: WHO.
- Babor TF, Higgins Biddle JC, Saunders JB, Monteiro MG (2001) AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for use in primary care. 2nd ed. Geneva: WHO.
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, et al. (2009) Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and six months later. Drug Alcohol Depend 99(1-3): 280-295.
- Substance Abuse and Mental Health Services Administration (2019) SBIRT: Screening, Brief Intervention, and Referral to Treatment. A Comprehensive Approach to the Delivery of Early Intervention and Treatment Services. Rockville, MD: SAMHSA.






























