Abstract
The HIV Infectious Disease Advisory Summit, held from September 10 to 12, 2024, in Dakar, Senegal, served as a bilingual platform for scientific exchange and education, fostering peer-to-peer learning and collaboration among public health specialists and experts. The summit focused on three pivotal areas: (1) MTCT with a focus on HBV, (2) implementation of 4th generation HIV Testing to capture acute infections, crucial for achieving the UNAIDS 95-95-95 targets, and (3) advocating for utilization of BB HIVST to improve access and acceptance among diverse populations.
This report consolidates the critical insights, challenges, and recommendations that emerged from the summit discussions. Key findings highlighted regional health challenges, such as a 35.5% HIV prevalence among MSM in the Greater Banjul region of The Gambia in 2018; an 8.1% HBV adult prevalence in Nigeria in 2023; and, a congenital syphilis rate of 26.77 per 100,000 live births in DRC in 2022. Sub-Saharan Africa accounts for 70% of global HIV self-testing demand. Liberia’s dual HIV-syphilis testing model in antenatal care significantly increased syphilis testing from 8% to 75% among pregnant women. Nigeria shows favourable acceptance rates of BB HIVST among high-risk populations, reflected in The STAR Survey project findings, that 17.1% of prior oral HIVST users prefer BB HIVST, compared to 12.5% who preferred oral HIVST. Sierra Leone reported how provider-initiated HIV testing and counselling increased from 4% to 95% in most hospitals, despite challenges like stigma and supply chain gaps.
Key recommendations include 1) formation of robust national policies and guidelines, 2) public awareness campaigns to reduce stigma and increase testing uptake, and 3) strategies to ensure the best available tests reach the appropriate populations on time. Cross-cutting themes emerged, highlighting the need for updated funding proposals, impactful awareness campaigns, data-driven interventions, and robust community engagement. These elements are deemed vital to securing support from development partners and enhancing health outcomes. The summit’s outcomes outline actionable next steps that aim at strengthening regional responses to HIV, syphilis, and HBV.
Keywords: PMTCT (Prevention of Mother-to-Child Transmission); Triple elimination; 4th generation HIV Testing; Blood-based HIV Self-Testing (BB HIVST); Central Africa; West Africa
Abbreviations:MTCT: Mother-to-Child Transmission; BB HIVST: Blood-Based HIV Self-Testing; HBV: Hepatitis B Virus; UNAIDS: Joint United Nations Programme on HIV/AIDS; CWA: Central and West Africa; CSOs: Civil Society Organizations; NGOs: Non-Governmental Organizations; ANC: antenatal Care
Introduction
The HIV Infectious Disease Advisory Summit, held from September 10 to 12, 2024, in Dakar, Senegal, provided a vital bilingual platform for scientific exchange and education, fostering peer-to-peer learning and collaboration among public health specialists and experts. This summit focused on three critical areas essential for combating the intertwined epidemics of HIV, syphilis, and Hepatitis B Virus (HBV): (1) Triple Elimination of Mother-to-Child Transmission (MTCT) with an emphasis on HBV, (2) Implementation of 4th-generation testing to effectively capture acute infections, thereby supporting countries in achieving the Joint United Nations Programme on HIV/AIDS (UNAIDS) 95- 95-95 goals [1], and (3) Advocating for the utilization of Blood- Based HIV Self-Testing (BB HIVST) to enhance accessibility and acceptance among diverse populations.
The summit was timely, reflecting the pressing need for innovative solutions in the Central and West Africa (CWA) region, which encompasses 22 countries and approximately half a billion people [2]. Notably, about 12% of this population is under the age of 15, making it one of the youngest demographics globally and constituting roughly 43% of Africa’s total population [2]. The region is characterized by a disproportionately high prevalence of HIV, syphilis, and HBV, underscoring the urgency of the summit [3-5]. For instance, the Greater Banjul region of The Gambia reported an alarming HIV prevalence rate of 35.5% among men who have sex with men (MSM) in 2018 [6], while Nigeria faced an HBV prevalence rate of 8.1% among adults aged 15-64 years in 2023 [7]. Moreover, the Democratic Republic of Congo (DRC) documented a congenital syphilis rate of 26.77 per 100,000 live births in 2022 [8]. These statistics highlight the region’s critical public health challenges, further exacerbated by economic instability and limited healthcare access. Throughout the summit, 120 participants from countries including Senegal, Nigeria, Liberia, and Sierra Leone shared their experiences and insights, reflecting diverse perspectives on regional health successes and challenges. These discussions emphasized the importance of learning from previous initiatives and successful collaborations, as well as the need for capacity building and innovative approaches to ensure long-term impact.
A recurring theme of the sessions was the imperative to ensure funding to support relevant interventions and equitable access to diagnostics for hard to reach and marginalized populations. Overcoming stigma and implementation barriers remained central to the conversations. The agenda featured thematic presentations, interactive discussions, group work, and case study reviews, all designed to facilitate knowledge sharing and collaboration. The key outcomes from this meeting included the establishment of collaborative partnerships, identification of strategic priorities, better understanding of available funding pathways, and the need for clear implementation plans which should be tailored to address the region’s pressing health needs. By harnessing the collective expertise and commitment of stakeholders, the summit aimed to bolster regional responses to HIV, syphilis, and HBV prevention and treatment. The three-day meeting held the aim of being a scientific and educational platform to encourage peer-to-peer learning, engagement and best-practice sharing amongst public health specialists and experts in the field to bridge diagnostic gaps in infectious diseases.
Meeting objectives included:
• Presenting the science, economical and clinical value of
rapid diagnostic testing in CWA.
• Sharing best-practice on programmatic and point of care
diagnostics amongst key opinion leaders from CWA Countries.
• Networking and workshop experience for public
health specialists to brainstorm paths and initiatives to disease
elimination while leveraging cross-country experience and
expertise.
Participating countries and organizations: Countries represented:
• Burkina Faso
• Burundi
• Cameroon
• Cote d’Ivoire
• Democratic Republic of Congo
• Liberia
• Nigeria
• Senegal
• Sierra Leone
Organizations represented:
• Abbott
• Cameroon Network of HIV-positive Adolescents and
Youth (RECAJ+) and Member of the Global Fund Youth Council
• HIV Division, Burundi
• HIV Programme, Democratic Republic of Congo
• HIV Testing Services Task Team, Nigeria
• Jhpiego, Nigeria
• National AIDS Control Program, Liberia
• National ART Task Team, Nigeria
• PMTCT Programme, Burkina Faso
• Programme National de Lutte Contre le SIDA, Senegal
Key Discussions and Debates
Triple elimination for MTCT (with a focus on HBV)
The pursuit of Triple Elimination of Mother-to-Child Transmission (MTCT) of HIV, syphilis, and HBV is impeded by the absence of integrated guidelines, notably in Sierra Leone, whereas Liberia is in the process of validating their guidelines. These structural deficiencies are compounded by service delivery challenges and the pervasive stigma associated with these infections. Liberia, however, has demonstrated a noteworthy model of progress.
Dr. Jonathan Flomo (Program Manager for the National AIDS & STI Control Program in Liberia), highlighted the significant impact of dual HIV-syphilis testing within antenatal care (ANC). Dr. Flomo elaborated that, in Liberia, 95% of pregnant women attend only one of the four scheduled antenatal ANC visits, making it vital to conduct the HIV-syphilis testing when the women do attend. Prior to the introduction of HIV-syphilis dual testing, 80% of pregnant women underwent HIV testing, and only 8% underwent syphilis testing. With the introduction of HIV-syphilis dual testing, Syphilis testing increased to 75%, representing “a game changer in Liberia”, and signifying a pivotal shift in maternal healthcare practices.
Dr. Flomo explained that this advancement underscores syphilis’s status as an “easy win,” given its cost-effectiveness and feasibility of detection and treatment, explaining that, despite being a preventable and treatable condition, MTCT of syphilis remains a silent threat, causing more child deaths globally than HIV. Dr. Flomo’s evidence presents a compelling case for prioritizing syphilis testing within PMTCT initiatives.
The dual HIV-syphilis testing advancement was facilitated by the revision of the national HIV Counseling and Testing guidelines in 2020, which now include HIV-syphilis dual testing [9]. This framework underscores the potential for triple testing initiatives, supported by country-specific training of trainers (ToT) programs to equip healthcare providers at the facility level. Additionally, the decentralization of services and incorporating syphilis screening and treatment indicators have enhanced programmatic planning and monitoring.
However, during group work, it became evident that other nations, such as Ghana are yet to develop policies for triple testing, alongside insufficient funding and training initiatives. Dr. Atsu Godwin Seake-Kwawu (Program manager for Viral hepatitis in Ghana) explained that awareness regarding triple elimination remains low, contributing to reduced demand for integrated testing services-a situation exacerbated by the stigma of positive diagnoses. Dispensing the hepatitis vaccine is also a key platform for hepatitis testing and management. The presence of testing kits and capacity building require funding support. However, funding partners fund only those countries that have a need for testing, highlighted, for example, by high prevalence of the disease and have a guideline or policy in place for end-to-end service provision, including treatment, not just testing.
For instance, a private sector collaboration with Ghana’s Ministry of Health and the Africa CDC was discussed, which exemplifies a multi-stakeholder collaboration, which supported the successful updating of the medicines list to include hepatitis management. Key takeaways underscore the necessity of developing national guidelines that integrate best available HIV, syphilis, and HBV elimination tools and strategies (including ToT and healthcare worker training), alongside public awareness campaigns to mitigate stigma and promote testing and treatment uptake.
Advancing HIV testing with 4th-generation assays
The integration of 4th-generation HIV assays is pivotal for the early detection of acute infections, a critical component in achieving the UNAIDS 95-95-95 targets. These assays facilitate early diagnosis, thereby enabling the reduction of onward transmission rates and ensuring timely linkage to care and initiation of treatment. The implementation of Determine HIV Early Detect (DHED), 4th generation HIV Testing in Burundi and Burkina Faso highlights both progress and ongoing challenges in this domain.
Dr. Aime Ndayizeye (HIV Division Manager, Burundi), presented on the topic of 4th generation HIV Testing in Burundi, where the HIV prevalence stands at 0.29%, and HBV and Hepatitis C Virus (HCV) prevalence between 5-10% and 10%, respectively. Dr Ndayizeye described Burundi’s new screening campaign, which is delivered in collaboration with service providers, targeting key populations, plus pregnant women, men, and utilizing index testing methodologies. Although 4th generation HIV Testing has been introduced, Dr. Ndayizeye emphasized the necessity of increased awareness and advocacy to enhance its utilization. The presentation underscored the importance of capacity building among service providers for expanding access and utilization of 4th-generation testing.
Mr. Manason Rubainu (HIV Laboratory Task Team Chairman, Nigeria) spoke on HIV Testing Strategies in Nigeria, a country with an estimated 1.9 million people living with HIV, representing one of the highest burdens globally [10]. The presentation highlighted existing strategies to combat the epidemic, including the integration of HIV testing into general healthcare services, antenatal care, and community-led initiatives such as mobile testing units and door-to-door campaigns. Nigeria’s National HIV/ AIDS Strategic Framework (2019-2021) has focused on scaling up testing, especially in high-prevalence areas and among key populations, along with the introduction and expansion of selftesting.
Mr. Rubainu further elaborated on Nigeria’s validation of the DHED 4th-generation HIV rapid test kit, capable of simultaneously and differentially detecting HIV antibodies and the HIV p24 antigen. He explained that this test is more efficient for diagnosing acute HIV infections than 4th-generation ELISA tests and recommended its inclusion as a first-line rapid diagnostic test (RDT). The potential of DHED testing to inform targeted public health interventions was highlighted as a significant advancement. Panel discussions drew on parallels from Senegal, where the introduction of rapid tests has revolutionized the accessibility of diagnostics, enabling communities to participate in self-testing. Prof. Diop Ndiaye Halimatou (Laboratoire Bactériologie-Virologie, Senegal) emphasized the importance of training and supervision, along with quality controls, to ensure effective implementation. Additionally, in line with WHO recommendations, it is crucial that individuals are retested before receiving treatment.
Key recommendations from these discussions include implementing comprehensive training programs for healthcare providers to enhance the effective use of 4th generation HIV Testing and incorporating these tests into broader screening initiatives targeting high-prevalence groups. The discourse suggests that scaling up viral load testing, integrating HIV testing with other health services such as tuberculosis, malaria, and sexual and reproductive health, and leveraging digital health innovations, for example, a dashboard that returns results electronically in realtime, thereby eliminating wait times, could significantly improve monitoring and follow-up processes. These efforts underscore the critical need for public-private partnerships and community engagement in the design and implementation of testing programs, and ensuring informed consent and confidentiality for individuals. By addressing these challenges, countries can move towards more effective management and control of the HIV epidemic, aligning with global health objectives.
Blood-based HIV self-testing (BB HIVST)
Dr Victor Adepoju (Project Director - Global Projects, UNITAID HIV, Viral Hep and Infectious Diseases ST Africa (STAR); Nigeria Country Director Jhpiego), presented on the efficacy and strategic implementation of HIVST in Nigeria, emphasizing its role in enhancing accessibility, particularly for hard-to-reach populations. He emphasized that Sub-Saharan Africa accounts for 70% of the global demand for HIV Self-Testing (HIVST), and that Nigeria reports favourable acceptance rates among high-risk populations, especially men, who report preferring BB HIVST over its oral counterpart due to its higher accuracy (99.5% sensitivity and 98.5% specificity), despite it being more invasive in nature. Studies, including the STAR project survey, showed that 17.1% of prior oral HIVST users prefer BB HIVST, 12.5% of prior BB HIVST users preferred oral HIVST, and 7.7% of prior users of both Oral and BB HIVST prefer blood-based tests [11,12].
Dr Adepoju emphasized that BB HIVST is not only a
programmatic choice, but also a behavioural choice, and that
the preference for both tests is dynamic and subject to change
based on availability and user experience. In Nigeria, HIVST is
a vital strategy to increase testing among groups facing limited
access or stigma-related barriers. Nigeria’s development
of operational guidelines for HIVST in 2018 facilitated the
piloting and scaling of distribution through various models,
including community, facility, workplace, and pharmacies. The
pharmacy model, extensively utilized, incorporated blood and
oral HIVST into a pre-accreditation training program for Patent
Medicine Vendors (PPMVs) and community pharmacists. This
initiative, supported by the Pharmacy Council of Nigeria and
the Association of Community Pharmacists of Nigeria (ACPN),
ensured the affordability of HIVST kits. Dr Adepoju underscored
that BB HIVST is particularly advantageous for individuals at
higher risk of recent HIV exposure. The dynamic nature of selftesting
preferences necessitates adaptability based on available
options and user experience. A positive HIV self-test requires
confirmation following the national HIV testing algorithm. Dr
Adepoju described the key lessons from Nigeria’s experience to
include:
• tailored-training and collaboration with partners
improve care linkages and test result return rates
• engagement with the private sector, particularly
pharmacies, facilitated kit accessibility through demand-side
financing, transitioning from free to subsidized distribution
models
• removing regulatory barriers and integrating HIVST into
national systems ensured proper data tracking.
Dr Adepoju concluded that BB HIVST is vital for scaling testing and achieving 95-95-95 goals, and requires improved education and messaging. Dr Ali Johnson Onoja (CEO at African Health Project, Nigeria; HTS Task Team Chairman, Nigeria) addressed the topic of linkage to care following HIV BB ST in Nigeria, highlighting that of the 770,588 HIVSTs conducted in 2023, 479,287 were assisted and 291,301 were unassisted. The widespread use of HIV BB ST enables earlier knowledge of HIV status, facilitating timely treatment and contributing to achieving the 95-95-95 targets. However, barriers to treatment linkage persist, including limited access to care, stigma, unfriendly healthcare providers, long wait times, and fear of antiretroviral therapy (ART) side effects.
Dr Onoja recommended strategies to enhance linkage to care, such as community and facility-based testing, tracking mechanisms, messaging on test kit leaflets regarding accuracy and early treatment, and support platforms like help desks and web-based services. It is crucial to provide pre-test and posttest counseling through HIVST service providers or community distributors. HIVST serves as a preliminary screening tool, necessitating immediate confirmation of positive results according to the national algorithm. Addressing data gaps in the contribution of HIVST to testing outcomes and linkages to treatment remains essential.
Key recommendations emphasize integrating HIVST into national HIV policies and advocating for pharmacy-based distribution models to ensure sustainable scale-up. By addressing these challenges, countries can move towards more effective management and control of the HIV epidemic, aligning with global health objectives.
HIV testing strategy case studies
Dr. Nadia Yameogo (PMTCT Programme Manager, Burkina Faso) and Dr. Sulaiman Lakoh (Director Disease Prevention, Sierra Leone) highlighted key strategies for improving HIV testing through Burkina Faso and Sierra Leone case studies.
Burkina Faso
Dr. Yameogo discussed the National Plan for the Elimination of Mother-to-Child Transmission of HIV, developed in 2021. The plan aims to reduce new cases and prevalence of HIV, congenital syphilis, and HBV. Key strategies include resource mobilization, capacity development, improved data quality, and community involvement. These efforts led to over 95% HIV testing and ARV treatment initiation among pregnant women and improved early detection and ARV prophylaxis for HIV-exposed children. Success factors included availability and implementation according to national guidelines, healthcare provider training, community support, and commitment from all stakeholders.
Sierra Leone
Dr. Lakoh presented the challenges and strategies in HIV testing, noting a 1.7% adult HIV prevalence with low partner testing and significant regional disparities [13]. A Quality Improvement Collaboration (QIC) improved provider-initiated HIV testing and counseling (PITC) from 4% to 95% in most hospitals. Challenges included stigma, data limitations, testing service integration, and rapid test kit stockouts [14]. Current strategies focus on using an HIV patient tracker for care linkage, public education, technology for supply chain gaps, and integrating testing services into national guidelines. Both presenters emphasized the importance of stakeholder commitment, community involvement, data utilization, and resource availability in enhancing HIV testing
Cross-Cutting themes from the meeting presentations and sessions
Four cross-cutting themes emerged from the summit presentations and sessions:
Comprehensive guidelines and funding proposals
Updated and thorough guidelines are crucial for securing funding from global donors like the Global Fund and PEPFAR. Proposals should include detailed implementation plans and strategies to enhance effectiveness and alignment with donor priorities.
Public awareness and stigma reduction campaigns
Campaigns must raise awareness about testing and treatment options, focusing on triple elimination and HIVST. The goal is to ensure timely and appropriate testing access for all individuals, reducing stigma and misconceptions.
Data-Driven interventions
Strengthening data collection and monitoring systems is vital for assessing program impacts and maintaining donor support. Integrating triple-elimination indicators into monitoring frameworks will enhance evaluation processes.
Community engagement and integration
Engaging communities and incorporating local nuances and cultural contexts into health strategies help improve acceptance and penetration of testing, especially in hard-to-reach areas. Collaborative efforts with community-based organizations (CBOs) can foster trust and acceptance.
Next steps
The following steps are recommended to maintain momentum and integrate the deep learnings shared at the meeting.
Follow-Up meetings
Schedule follow-up meetings to monitor progress on shared learnings, recommendations, and commitments from the summit.
Continued collaboration
Maintain stakeholder engagement to support and innovate initiatives discussed during the summit.
Policy development
• Integrate HBV into national guidelines for a cohesive
Triple Elimination strategy.
• Develop and update guidelines to include diverse testing
options, like BB HIVST and 4th generation HIV Testing.
Capacity building
• Implement Training-of-Trainers (ToT) programs to
empower healthcare providers with new diagnostic protocols.
• Conduct regular assessments to ensure high standards
in HIV and syphilis counseling and testing.
Community engagement and awareness campaigns
• Launch culturally relevant campaigns to reduce HIV
stigma, targeting key populations.
• Utilize social media and CBOs to promote new testing
methods, including BB HIVST.
Funding and resource mobilization
• Strengthen funding proposals with operational plans
aligned with donor priorities.
• Explore innovative financing models, like public-private
partnerships, for sustainable funding.
Data-Driven interventions
• Enhance monitoring systems to track HIV testing and
triple elimination outcomes.
• Use real-world data to demonstrate new diagnostic
tools’ effectiveness, guiding health policy decisions.
Conclusion
The summit underscored the need for integrated approaches, innovation, and collaboration to tackle HIV, HBV, and syphilis challenges effectively. By following the outlined next steps and recommendations, countries can advance toward global HIV targets, improving health outcomes for vulnerable populations.
Contributors
We thank the following speakers for their contributors, without whom this meeting and report would not have been as fruitful. Dr. Atsu Godwin Seake-Kwawu (Program manager for Viral hepatitis in Ghana); Dr. Aime Ndayizeye (HIV Division Manager, Burundi); Prof. Diop Ndiaye Halimatou (Laboratoire Bactériologie-Virologie, Senegal) Dr. Nadia Yameogo (PMTCT Programme Manager, Burkina Faso) and Dr. Sulaiman Lakoh (Director Disease Prevention, Sierra Leone);
Declaration of Interests
Funding for this report was provided by Abbott. The report was written by Policy Wisdom, LLC. Allira Attwill, Amit Mehto, Claudia Ramly, and Ana Rita Gonzalez are consultants at Policy Wisdom LLC. This article and the educational event were sponsored by Abbott. The presentations were independently prepared by the speakers to share best practices from their respective countries.
Supplementary Materials/Annexures
List of Speakers
The following speakers presented at the meeting. Listed in
alphabetical order.
• Dr Ali Johnson Onoja
• Dr. Aime Ndayizeye (HIV Division Manager, Burundi)
• Dr. Atsu Godwin Seake-Kwawu (Program manager for
Viral hepatitis in Ghana)
• Dr. Jonathan Flomo
• Dr. Nadia Yameogo (PMTCT Programme Manager,
Burkina Faso)
• Dr. Sulaiman Lakoh (Director Disease Prevention, Sierra
Leone)
• Dr. Victor Abiola Adepoju
• Mr. Manason G Rubainu
• Prof. Diop Ndiaye Halimatou (Laboratoire Bactériologie-
Virologie, Senegal)
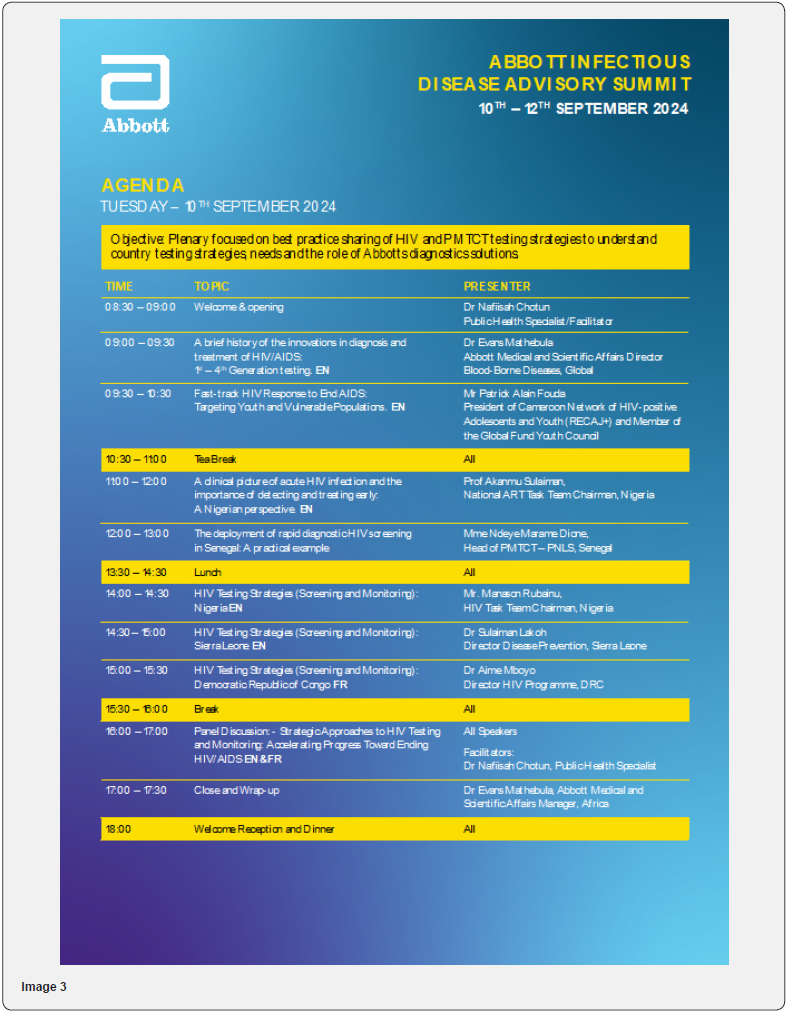
Image (1-7)






Acknowledgement
We acknowledge the contributions of all participants, speakers, and stakeholders whose expertise and dedication are invaluable in addressing HIV and infectious diseases in Central and West Africa.
References
- UNAIDS (2023) The Path that Ends. UNAIDS Global AIDS Update.
- World Bank (2024) The World Bank in Western and Central Africa.
- Mussa Aamirah, Jarolimova Jana, Ryan Rebecca, Wynn Adriane, Ashour Dina, et al. (2024) Prevalence Among People Living with and Without HIV in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Sexually Transmitted Diseases 51(3): 1-7.
- World Health Organization (2023) Sexually transmitted infections (STIs).
- Coalition for Global Hepatitis Elimination (2022) Central African Republic.
- UNAIDS (2020) Country progress report-Republic of The Gambia Global AIDS Monitoring.
- WHO (2025) Nigeria News. In Nigeria, boosting viral hepatitis awareness and treatment.
- WHO (2024) Global Health Observatory Data Repository (African Region).
- Flomo J, Efronson E (2024) Liberia’s Breakthrough in Dual Syphilis and HIV Screening. BMJ Global Health Blog.
- Adeniran A, Shogbamimu Y, Ojo OY, Chieme FC, Olowofeso HO, et al. (2023) How Do People Living with HIV (PLHIV) and AIDS Feel About the Quality of Care They Received Amid the COVID-19 Pandemic in Lagos, Nigeria? J Int Assoc Provid AIDS Care 22: 1-7.
- O Reilly A, Mavhu W, Neuman M, Moses K Kumwenda, Cheryl C Johnson, et al. (2022) Accuracy of and preferences for blood-based versus oral-fluid-based HIV self-testing in Malawi: a cross-sectional study. BMC Infect Dis 22 (Suppl 1): 1-11.
- Shapiro AE, van Heerden A, Krows M, Kombi Sausi, Nsika Sithole, et al. (2020) An implementation study of oral and blood-based HIV self-testing and linkage to care among men in rural and peri-urban KwaZulu-Natal, South Africa. Journal of the International AIDS Society 23(S2): 1-8.
- Lakoh S, Firima E, Jiba DF, Sesay M, Conteh MM, et al. (2019) Low partner testing in high HIV prevalence setting in Freetown, Sierra Leone: a retrospective study. BMC Res 12(1): 1-6.
- Kassa G, Dougherty G, Madevu Matson C, Egesimba G, Sartie K, et al. (2020) Improving inpatient provider-initiated HIV testing and counseling in Sierra Leone. PLoS One 15(7): 1-11.






























