Abstract
This Patient Accord highlights the value of precision medicine (PM) in improving cancer care through biomarker-guided treatments. With a focus on Argentina, Brazil, India, and Mexico, the Patient Accord draws on patient insights to identify gaps in access, awareness, and policies, as well as structural barriers that hinder PM adoption in emerging economies. The methodology included a non-systematic literature review of studies from 2019-2024 and collaboration with patient advocacy groups through virtual meetings to ensure patients’ perspectives shaped the findings. The Accord is a tool to advocate for PM as the gold standard of care and provides policy and structural recommendations to ensure equitable implementation and improved outcomes.
Keywords:Precision medicine; Genomic research; Patient-cantered care; Genetic testing; Healthcare access; Policy advocacy; Affordable healthcare; Policy advocacy
Abbreviations:PAGs: Patient Advocacy Groups; LCIF: Lung Connect India Foundation; PM: Precision medicine; IARC: International Agency for Research on Cancer; MoH: Ministry of Health; INC: National Cancer Institute; WHO: World Health Organization
Objective
This Patient Accord outlines patients’ perspectives on the value of biomarkers in determining the most effective treatment options. It is a tool to advocate for the global adoption of biomarkers and precision medicine (PM) as the standard of care, focusing on four emerging economies: Argentina, Brazil, India, and Mexico. The document aims to promote broader acceptance and implementation of PM to improve patient outcomes worldwide by highlighting patient insights.
Methodology
A non-systematic literature review was conducted to gather recent evidence on (1) the benefits of precision medicine (PM) in oncology, (2) the level of awareness among patients and patient advocacy groups (PAGs) about PM and biomarkers, (3) the burden of cancer, policies, and the adoption of biomarkers and innovative drugs in selected emerging economies, and (4) barriers to broader adoption and reimbursement. Keyword searches were performed in Google Scholar and PubMed, focusing on studies from 2019-2024, especially from the selected emerging economies. Older publications were included only if they provided essential foundational information not covered in newer studies. To ensure the inclusion of patients’ perspectives, leading PAGs from the target countries collaborated to create and validate this document. These groups provided critical insights into patient pathways, barriers, challenges, and recommendations. The participating organizations included the Liga Argentina de Lucha Contra el Cáncer (LALCEC) and Donde Quiero Estar from Argentina, Oncoguia from Brazil, Lung Connect India Foundation (LCIF), and Fundación Fomento de Desarrollo Teresa de Jesus (FUTEJE) from Mexico. Their contributions were gathered through two virtual meetings to discuss, review, and refine the draft collectively. The process culminated in a post-meeting validation to achieve a consensus on the Patient Accord. All participating patient representatives formally approved the final content of this document.
Background and Introduction
Cancer is a leading cause of death and disability in emerging economies, accounting for 14.9% of the disease burden. Despite advances in health coverage, barriers like delayed diagnosis, unequal access to treatments, and high-cost drugs hinder better cancer care and outcomes [1-3]. Precision medicine (PM) tailors’ disease prevention and treatment by considering genetic, environmental, and lifestyle variations. In cancer care, biomarkers guide clinical decisions, improving diagnosis, treatment, and health outcomes [4]. PM improves cancer patients’ quality of life and saves resources by focusing treatments on disease characteristics, avoiding costly, low-success options [5]. Increasing evidence highlights its value, and many are advocating for PM as the standard of care in high-income and emerging economies. Patients have the right to be heard and to be informed about PM’s potential so they can make decisions that are in their best interest. Evidence increasingly supports PM in cancer treatment [6,7], with many patients understanding its value, such as optimizing treatment by testing tumours to guide it [8]. However, access to biomarker and genetic testing remains limited. Patients still encounter disparities, and there remains a need for greater patient familiarity to advocate for these advantageous technologies [9,10]. This Patient Accord aims to establish PM as the gold standard of care. It outlines PM, biomarkers, and their cancer applications; examines PM’s value and current situation in emerging economies; and reviews global and regional policies. Using critical insights from patient advocates, it identifies gaps, barriers, and challenges to PM implementation and concludes with patient-driven recommendations.
The Value of Improving Cancer Care
Globally, cancer accounts for 14.6% of deaths and nearly one in ten disability-adjusted life years lost (DALYs). Though some emerging countries have a lower cancer burden, it remains a leading cause of death [11]. The WHO’s International Agency for Research on Cancer (IARC) reports 19.1 million people living with cancer in the last five years [12]. With current trends unhindered, IARC estimates cancer cases will grow to 11.8 million and annual deaths to 7,052,117 by 2045 [13]. Precision medicine (PM) has the potential to improve this scenario.
PM represents a transformative approach to cancer care, offering the most promising pathway to address this growing global health challenge, but it poses significant challenges in low-resource settings, highlighting concerns about health equity [14]. However, precision oncology offers the potential for greater efficacy, enhanced safety, and reduced economic burden [15]. To ensure these advances benefit patients globally, a multi-stakeholder approach is essential, focusing on evidence generation, value assessment, and effective healthcare delivery [16]. The Cancer Genome Atlas (TCGA) mapping of genetic alterations in various cancers enables precision oncology with molecular diagnostics and targeted therapies, significantly improving patient outcomes.
Current Situation Policies
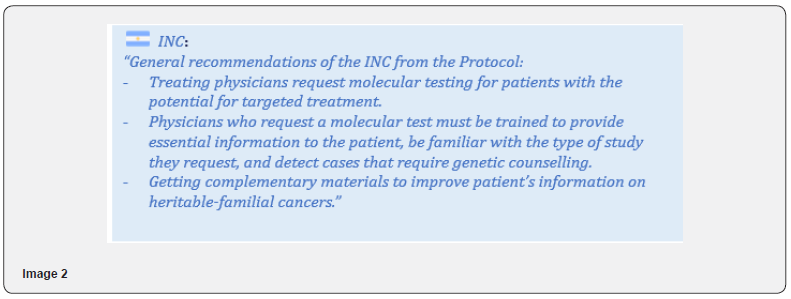
The Argentinian Ministry of Health (MoH) and National Cancer Institute (INC) recently published a “Protocol on the role of oncological genetic counselling within the framework of precision oncology” as part of the National Familial Cancer Program [17]. As approved in February 2024, Brazil covers biomarker testing for targeted therapies for NSCLC based on cost-effectiveness [18]. Issued in December 2023, this country’s National Cancer Policy emphasized principles of more precise, less invasive diagnostics and therapies [19]. India’s MoH Operational Framework for Managing Common Cancers lacks guidance on precision or personalized therapies, and no related PM policy was found [20]. The Specific Action Plan of Cancer Prevention and Control in Mexico does not address molecular diagnostics or PM [21]. However, the General Health Council’s protocol for malignant breast tumours mandates comprehensive genetic testing and counselling for breast cancer patients, though it’s unclear if treatment algorithms address variations beyond HER2 [22]. The lung cancer protocol, likewise, recommends genetic/molecular testing [23]. Despite these advances, access to precision diagnostics in public settings of upper-middle-income countries remains challenging-including in Brazil and Mexico-though some cancer centres offer these innovative medicines.
Structural conditions: funding, access, infrastructure, and workforce Funding and access
Funding for PM and companion diagnostics is rare outside high-income countries and is usually absent from state budgets. Companion diagnostics (CDx) are essential for guiding the safe, effective use of targeted therapies by identifying patients most likely to benefit based on characteristics like genetic profiles [24]. Despite limited funding overall, emerging countries have specific mechanisms. In Argentina, for example, cancer medicines in the public system are funded through the National Oncologic and Special Drugs Bank, which received ARS$11,278.2 million (US$13.1 million*) in 2024 [25]. Nevertheless, as remarked by LALCEC and Donde Quiero Estar, provincial health authorities may have additional funding mechanisms for innovative medicines, though coverage varies widely. Brazil’s Unified Health System (SUS) provides some high-precision therapies and companion diagnostics but lacks earmarked budget allocations [26]. In contrast, funding for high-cost innovative PM technologies is not available for people not covered under any insurance scheme (government or private), while government employees, exservicemen, and serving officers may have access to PM [27]. This disparity in funding directly impacts access to these advanced treatments.
In Mexico’s public non-social-security system, healthcare, infrastructure, and high-cost disease medicines are funded through the FONSABI fund, which received about MXN 9,443 million (US$552.2 million*) in 2024 [28,29]. Social security institutions fund the diagnostics and medicines that are included in both the National Compendium of Health Supplies (CNIS) and their institutional lists. Expenditure on specialty medicines, however, is low in most upper-middle-income countries. Argentina’s total health expenditure on specialty medicines is 4%, 2% in Brazil, and 3% in Mexico, compared to the 5% OECD average [30]. Access to PM requires both market authorization and reimbursement. Market authorization allows medicines to be available, while reimbursement determines if patients can afford and access them.
PM access has grown globally, especially in high-income regions like North America, Western Europe, and Japan, but adoption has been slower in emerging economies. No crosscountry comparisons on companion diagnostics access were found, though trends likely mirror those for medicines. An analysis by IQVIA found that India has the lowest share of targeted oncology medicines among all surveyed countries and regions, with minimal change from 2018 to 2023. Latin America, though higher than India and META, showed an uneven trend, with the share of targeted oncology medicines declining from 2019 to 2022 and beginning to recover in 2022 [31]. IQVIA’s study indicates minimal use of PD-1/PD-L1 inhibitors in emerging economies, with slow adoption in Latin America [31]. Meanwhile, in India, these technologies are advised to all patients, but only those who are financially able can access the required genetic testing [27]. While there is broad awareness of these technologies, the infrastructure and financial resources for access are often lacking in the public system. Therefore, India’s fragmented public health system leads to significant inequities, with more comprehensive coverage from the subsystems for government employees and military personnel. In addition, India shows significant delays in adopting new technologies, with low approval rates for new drugs: Only 17% of drugs launched globally from 2012 to 2021 were approved in India by 2022, with oncology drugs taking an average of 48 months to gain approval after their global launch [32].
In LATAM, the local availability of globally approved oncology drugs is higher but still limited. Of 115 oncology drugs approved globally (2014-2021), 73 are approved in at least one LATAM country. Argentina approved 48 but reimburses 37 only through the private sector, with none fully accessible via public healthcare. However, Argentina’s National Commission of Health Technology Assessment and Clinical Excellence (CONETEC) has begun evaluating PM, with binding recommendations. Brazil approved 41 drugs, with 20 in the public sector (three fully, 17 partially (I)) and 29 available privately. Mexico approved 41 drugs, with 26 partially (II) or fully available in public institutions and 15 only accessible through private insurers [33]. The affordability of oncologic drugs is a major challenge in LATAM, where prices are often higher and more variable than in high-income countries [34]. Factors driving higher and inconsistent LATAM prices include weak pricing regulations, limited reimbursement policies, and insufficient bargaining power [35]. Precision oncology funding in emerging markets, particularly Latin America, is hindered by limited government support for research and biobanks, unlike well-funded initiatives in high-income countries.
Finally, discussing precision oncology funding in emerging markets must include the availability of public resources for research and biobanks [35]. Unlike in high-income countries, this funding gap forces researchers to depend on external sources, such as pharmaceutical companies and fundraising [36]. Therefore, the lack of local resources influences research priorities and underscores the need for greater investment to ensure Latin American representation in precision oncology advancements [34].
Infrastructure and workforce
Argentina, Brazil, and Mexico have significant laboratory capacity for genetic and molecular diagnosis but lack the scale and reach for full access [37-39]. As LALCEC mentioned, a study by Argentina’s National Cancer Institute (INC) shows nearly 60% of genetic diagnostic tests occur in Buenos Aires. Mexico has PM experts (mostly trained abroad) and recently launched training programs, such as the precision oncology program at the National Institute of Genomic Medicine (INMEGEN). However, local graduates are still insufficient, with only Mexico City reaching one medical geneticist per 100,000 population [40]. Oncologist training must ensure readiness to utilize available PM treatments. In India, according to LCIF, several genomics and PM initiatives have been implemented in major government-funded tertiary hospitals, such as Tata Memorial Hospital and Rajiv Gandhi Super Specialty Hospital, indicating some existing investment and capacity. However, their studies report limited sample sizes, with fewer than 10,000 sequences [41]. In the private sector, individual cancer centres offer tumour boards, precision oncology diagnostics, and treatments with advanced labs and quick turnaround times [42-44]. These limited efforts are steps in the right direction, but they are insufficient to meet the needs of the Indian population. The Indian oncology workforce is also insufficient, with about one oncologist per million people in both countries [45,46].


Pathways to care
Pathways to care are pivotal in the outcomes of cancer treatment, as survival rates are closely related to diagnosis and treatment delays. In Argentina, bureaucratic hurdles delay access to therapies even after approval, though the Ministry of Health’s Access Map platform provides guidance on navigating these processes by province, as remarked by Donde Quiero Estar [47]. In Brazil, many patients, particularly in the northern and midwestern regions, must travel to other municipalities for treatment [48]. In India, while public cancer centres offer subsidized treatments, they face limited capacity, shortages of essential medications, and long radiotherapy wait times [45]. In Mexico, the median interval between detection and treatment is seven months [49], with public healthcare limitations pushing more patients to private care. For instance, breast cancer cases in private facilities nearly doubled from 2018 to 2019 [50].

Gaps, Barriers, and Challenges
The participating organizations agree that the main barrier to adopting precision medicine (PM) is a lack of awareness among the general population and patients, who often do not know which tests they need or the treatments they are entitled to under current policies.
Policy
Argentina’s national cancer control policy lacks a single cohesive document, and genetic diagnostics are limited to hereditary cancers under the Familial Cancer Program [17]. Data for the tests performed under the program’s Protocol on the role of oncological genetic counselling within the framework of precision oncology are not publicly available. Additionally, as LALCEC and Donde Quiero Estar observed, cancer measurement in the country faces deficiencies, relying on the Institutional Tumour Registry of Argentina (RITA), which collects data from 44 hospitals but is not nationally representative. Another challenge is the fragmentation of Argentina’s health system, which lacks a unified coverage policy, as the existing medicines and services formulary (PMO) varies by province (as LALCEC indicated). Additionally, there is no pooled procurement mechanism, though incipient efforts are underway to establish one [51].
In Brazil, the National Policy on Prevention and Control of Cancer, introduced in December 2023, mentions “more precise and less invasive” diagnostics and therapies but limits these to those already incorporated into the SUS [19]. Additionally, as noted by Oncoguia, implementation is delayed, as the necessary regulations have yet to be issued (as of November 2024).
India lacks a stand-alone cancer policy, with cancer control integrated into the National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) launched in 2010 [52]. Nevertheless, initiatives like mandatory oral, breast, and cervical cancer screening in 100 districts have been introduced, but uptake remains low. Mexico lacks a national cancer registry despite its presidential endorsement in 2014. After a promising start, during which population-based reporting was implemented in eight of 32 states, as mentioned by FUTEJE, the project was cancelled in the last administration, and funding was cut. The previous administration issued the Specific Action Program for Cancer Prevention and Control 2021-2024 [21], but no long-term National Cancer Plan or Law exists [53]. While genetic diagnostics are in clinical protocols for common cancers, other cancers lack updated guidelines [54,23]. FUTEJE points out that this is symptomatic of government efforts, which focus on the four highest-impact cancers-breast, cervical, lung, and prostateleaving cancers like colon cancer, the third most frequent and a leading cause of cancer deaths, without any dedicated plan or program.
Structural conditions Regulatory approval, funding, and reimbursement
Funding for PM in middle-income countries is scarce, with reimbursement for genetic diagnostics and innovative drugs remaining a significant challenge [25,28,29,31,55]. For example, Argentina’s National Special Drugs Bank has limited funding, and its list of covered medications has not been updated since 2022 [25,56]. This issue is exacerbated by the lack of an effective procurement policy, leading to higher drug prices than in highincome countries. In Brazil, even with CONITEC approval for public system coverage, low spending per cancer patient in the SUS limits access to genetic diagnostics and PM [57]. Evidence shows that India’s public health system does not cover or reimburse innovative PM, and while some treatments are available in large tertiary public hospitals and by the government employees and military subsystems, as LCIF commented, most patients must pay out-of-pocket or depend on private insurance, rendering these therapies inaccessible to many [27,45]. In Mexico, there is a significant backlog in marketing approvals. Additionally, a nearly 70% reduction in funding for high-cost medicines between 2019 and 2023 has led to frequent drug stock-outs of medicines included in Mexico’s government drug formulary (CNIS) [58]. Patients often face incomplete treatments or must purchase medications out-of-pocket, sometimes relying on patient organizations, such as FUTEJE, for support.
Beyond limited coverage for PM molecules, public coverage of companion and genomic diagnostics is also lacking or restricted. Currently, these advanced tests are often funded by pharmaceutical-company-sponsored programs [59,60]. While such initiatives improve access to some extent, participating organizations emphasize that they are typically short-term and cannot replace a sustainable system-wide coverage model supported by government financing. There are examples of successful policy-backed biomarker testing internationally. For example, England instituted the NHS Genomic Medicine Service after a pilot program showed its value, and France’s €1.7M EGFR testing program for 16,000 lung cancer patients saved €69M by avoiding ineffective treatments in 90% of cases [61,62].
Infrastructure and workforce
Middle-income countries face barriers to genetic counselling services due to a lack of medical geneticists and limited diagnostic tools [40]. In Argentina, Donde Quiero Estar shared that the shortage of pathologists delays basic tests like immunohistochemistry and forces patients to travel, with precision diagnostics often deprioritized as they may imply out-of-pocket costs to patients. Private labs conduct genetic testing, but costs are mainly covered by pharmaceutical companies and, only sporadically, by Obras Socials. Similarly, in Brazil, few oncologists are trained in PM, and many avoid prescribing genomic tests due to limited facilities or high patient costs. A study by the Brazilian Thoracic Oncology Group (GBOT), mentioned by Oncoguia, found most oncologists lacked adequate training to interpret genomic tests. Likewise, in India, as confirmed by LCIF, the scarcity of trained specialist providers limits precision oncology and cancer general care accessibility, forcing patients to travel long distances to tertiary hospitals, adding significant travel and lodging expenses to the cost of their treatment. These conditions make access to genetic diagnostics and PM a significant challenge across these countries.
Pathways to care
Cancer care in the focus countries faces significant challenges, including late-stage diagnoses and long delays from detection to treatment [49,47-45]. LALCEC pointed out how the lack of unified electronic clinical records in Argentina and other uppermiddle- income countries hinders the tracking of early symptoms or prior consultations. In addition, to access public cancer care, a new Argentinian policy requires patients to provide proof that they are not covered otherwise, but the certification process remains uncertain and unregulated, as Donde Quiero Estar stated. In Mexico, FUTEJE remarked that even patients with private insurance face barriers as policy limits often fail to cover the full cost of innovative treatments, forcing reliance on the public system. PM is mainly available through manufacturer-sponsored clinical trials requiring out-of-pocket testing and limited to institutions in Mexico City, such as the National Cancerology Institute (INCan) and the National Institute of Medical Sciences and Nutrition (INCMNSZ), restricting access for those in other regions.
As in other countries, the patient organizations participating in this Patient Accord help navigate access to innovative treatments through guidance and sponsored testing. However, as they said, bureaucratic delays, communication gaps, and administrative hurdles often obstruct treatment pathways. For instance, even stocked medications may not be administered until registered in hospital inventory systems. While patient organizations help circumvent such barriers, across emerging countries there is a lack of systematic policies ensuring transparent, system-wide access. The language of existing coverage policies is also not patient-friendly, adding another layer of difficulty.
Conclusion
To advance precision medicine (PM) in emerging countries, it is critical to address several interconnected challenges. Policy gaps, including the absence of cohesive cancer control strategies and limited integration of PM in public health systems, hinder widespread implementation. Structural barriers, such as inadequate funding mechanisms and inconsistent access to therapies due to regulatory delays, exacerbate the problem. Workforce deficiencies, including a shortage of trained specialists and uneven resource distribution, further limit PM’s reach. Additionally, patient awareness remains low, while bureaucratic hurdles and a lack of navigation systems complicate care access. This Patient Accord emphasizes the need for multi-stakeholder collaboration to develop sustainable frameworks, improve diagnostics, and expand access to life-saving therapies. Emerging countries must develop tailored approaches for PM adoption to improve quality of cancer care.
Recommendations
Participant organizations considered the current situation and the barriers reviewed above and shared the following recommendations.
Policy
• Support legislative initiatives that mandate national
cancer control plans with regular updates, multi-stakeholder
input, and earmarked budget. (III)
• Establish medium and long-term monitoring to evaluate
outcomes of cancer control plans.
• Include patient advocacy groups, medical societies, and
industry in policymaking to ensure patient-centred and costefficient
precision medicine solutions.
• Develop representative national cancer registries linked
to the identified electronic records for better burden assessment
and policy planning.
• Launch health literacy campaigns to improve awareness
of precision oncology and gold-standard care.
• Prioritize the incorporation of diagnostic tests over
drugs into public formularies to characterize tumours adequately
and optimize therapy selection, especially for late-detected
cancers, like lung cancers. Regulatory approval, funding, and
access
Structural conditions Regulatory approval, funding, and access
• Develop robust cost-effectiveness studies to
demonstrate the value of innovative technologies for submissions
to HTA entities.
• Disseminate information to improve patient access to
precision medicine technologies.
• Create system-wide navigation maps to simplify access
and clarify coverage rules.
• Implement innovative public procurement models for
medical technologies.
Infrastructure and workforce
• Facilitate specialized precision medicine training for
oncologists and pathologists.
• Expand laboratory capacity to meet genetic diagnosis
needs.
• Implement provider-patient communication protocols
to enhance quality of care.
Pathways to care
• Implement screening programs to reduce the share of
late diagnoses.
• Develop unified electronic clinical records to ease
referrals and system navigation.
• Streamline administrative requirements and develop
patient-friendly guides to socialize information about the pathway
to care.
Signatory Organizations
• Francisco Freyría Sutcliffe: Executive Director, Fundación Fomento de Desarrollo Teresa de Jesus (FUTEJE)Civil Society Working Commission for the Promotion of Comprehensive Cancer Care in Mexico, (México) • Luciana Holtz de Camargo Barros: President, Instituto Oncoguia, (Brazil) • Bruno Nascimbene: Executive Director, Liga Argentina de Lucha Contra el Cáncer (LALCEC), (Argentina) • María de San Martín: Executive Director, Donde Quiero Estar, (Argentina) • Sanjeev Sharma: Director and CEO, Lung Connect India Foundation (LCIF), (India)
References
The authors acknowledge financial support from Pfizer for this project. However, the funding organization was not involved in the literature review, virtual meetings, data analysis, or the development of the Patient Accord. Furthermore, Pfizer did not contribute to the project’s design, interpretation of findings, or manuscript preparation. The views and conclusions presented in this article are exclusively based on an evidence-based literature review and the insights provided by PAG leaders who participated in the virtual meetings.
References
- Global Cancer Observatory (2024) Cancer Today-Globo can 2022: Upper middle income [Fact sheet]. International Agency for Research on Cancer. World Health Organization.
- Werutsky G, Goessling G, Pellegrini RA, Ampuero GAS, Rebelatto T (2022) Socioeconomic impact of cancer in Latin America and the Caribbean. Archives of Medical Research 53(8): 818-825.
- Alzehr A, Hulme C, Spencer A, Morgan Trimmer S (2022) The economic impact of cancer diagnosis to individuals and their families: a systematic review. Supportive care in cancer 30(8): 6385-6404.
- Moore DC, Guinigundo AS (2023) The Role of Biomarkers in Guiding Clinical Decision-Making in Oncology. Journal of the advanced practitioner in oncology 14(Suppl 1) 15-37.
- Ciardiello F, Arnold D, Casali PG, Cervantes A, Douillard JY, et al. (2014) Delivering precision medicine in oncology today and in future-the promise and challenges of personalised cancer medicine: a position paper by the European Society for Medical Oncology (ESMO). Annals of Oncology 25(9): 1673-1678.
- Kästner A, Kron A, van den Berg N, Moon K, Scheffler M, et al. (2024) Evaluation of the effectiveness of a nationwide precision medicine program for patients with advanced non-small cell lung cancer in Germany: a historical cohort analysis. The Lancet Regional Health-Europe 36: 1-13.
- Brown A (2024) Precision Medicine in Oncology: Targeted Therapies and Genetic Profiling. International Journal of Machine Learning Research in Cybersecurity and Artificial Intelligence 15(1): 141-151.
- Ciardiello F, Adams R, Tabernero J, Seufferlein T, Taieb J, et al. (2016) Awareness, understanding, and adoption of precision medicine to deliver personalized treatment for patients with cancer: a multinational survey comparison of physicians and patients. The oncologist 21(3): 292-300.
- Martin NA, Tepper JE, Giri VN, Stinchcombe TE, Cheng HH, et al. (2021) Adopting consensus terms for testing in precision medicine. JCO Precision Oncology 5: 1563-1567.
- Botham J, Shilling V, Jones J (2021) Patient and public understanding of the concept of ‘personalised medicine’ in relation to cancer treatment: a systematic review. Future Healthcare Journal 8(3): 703-708.
- Global Burden of Disease Collaborative Network (2022) Global Burden of Disease Study 2021 (GBD 2021) Results. Institute for Health Metrics and Evaluation (IHME).
- IARC (2024) Cancer Today: Estimated number of prevalent cases, Both sexes, in 2022-All cancers- Upper middle income. Globo can 2022 (version 1.1).
- IARC (2024) Cancer Tomorrow: Estimated number of deaths from 2022 to 2045, Both sexes, age [0-85+]-All Cancers (Upper middle income). Globo can 2022 (version 1.1).
- Asrina A (2024) Precision Medicine Approaches in Oncology: Current Trends and Future Directions. Advances in Healthcare Research 2(1): 36-48.
- Rulten SL, Grose RP, Gatz SA, Jones JL, Cameron AJ (2023) The future of precision oncology. International Journal of Molecular Sciences 24(16): 1-18.
- Mateo J, Steuten L, Aftimos P, André F, Davies M, et al. (2022) Delivering precision oncology to patients with cancer. Nature medicine 28(4): 658-665.
- National Cancer Institute (2024) Protocol on the role of oncological genetic counselling within the framework of precision oncology. Argentina Ministry of Health Pp: 1-32.
- Brazilian Ministry of Health (2024) Recommendation Report-Procedure No. 879: rt-PCR for the identification of epidermal growth factor receptor (EGFR) mutation in patients with non-small cell lung cancer Pp: 1-106.
- Law No 14,758 of December 19, 2023. Official Gazette of the Union Ed. 241, Sec. 1.
- India Ministry of Health and Family Welfare (nd) Operational framework: Management of common cancers Pp: 1-44.
- Mexico Secretariat of Health (2021) Specific action program of cancer prevention and control 2021-2024 Pp: 1-44.
- Mexico General Health Council (2022) Technical protocol-C50 Malignant breast tumour. PT004.
- Mexico General Health Council (CSG) (2022) Technical Protocol-Malignant tumour of the bronchius and of the lung CIE-10: C34 (C34.0-C34.9). PT039. Commission to Define Treatments and Medicines Associated to Diseases that Cause Catastrophic Expenditures.
- FDA (2023) Companion Diagnostics.
- Government of Argentina (2024) Open Programming Explorer.
- Brazil Ministry of Health (2024) New medicines and treatments that will benefit over 14 thousand people incorporated.
- As reported by Lung Connect India Foundation (LCIF) in the meeting held on November (2024).
- Mexico Secretariat of Finance (2024) Budget Transparency-Open Data: Federal Expenditure Budget PEF.
- GUIDELINES for the operation of Budget Program U013 Health Care and Free Medicines for the Population without Social Security for the fiscal year 2024. IMSS-Bienes tar. Diario Oficial de la Federation.
- IQVIA (2020) Innovative Funding for Medicines in Latin America.
- IQVIA Institute for Human Data Science (2024) Global use of medicines 2024: Outlook to 2028.
- PhRMA (2023) Global Access to New Medicines Report Pp: 1-60.
- IQVIA/FIFARMA (2024) Patient WAIT indicator 2023 Latin America: Final report Pp: 1-41.
- Rivera Alcántara JA, Esparza Hurtado N, Galán Ramírez GA, Cruz Bautista I, Mehta R, et al. (2024) A systematic review of biobanks in Latin America: Strengths and limitations for biomedical research. The International journal of biological markers 39(2): 91-106.
- Moye Holz D, Vogler S (2022) Comparison of Prices and Affordability of Cancer Medicines in 16 Countries in Europe and Latin America. Appl Health Econ Health Policy 20: 67-77.
- de Castilla EMR, Mayrides M, González H, Vidangossy F, Corbeaux T, et al. (2024) Implementing precision oncology in Latin America to improve patient outcomes: the status quo and a call to action for key stakeholders and decision-makers. Ecancermedicalscience 18: 1-11.
- Argentina Ministry of Health (nd) Genetics laboratories. National Census of Public Resources for Diagnosis of Genetic Diseases.
- Bonilla C, Sortica VA, Schuler Faccini L, Matijasevich A, Scheffer MC (2021) Medical genetics workforce in Brazil: practitioners, services, and disease distribution. medRxiv 10: 1-36.
- Bravo ML, Santiago Angelino TM, González Robledo LM, Nigenda G, Seiglie JA, et al. (2020) Incorporating genomic medicine into primary-level health care for chronic non-communicable diseases in Mexico: A qualitative study. The International journal of health planning and management 35(6): 1426-1437.
- Bucio D, Ormond KE, Hernandez D, Bustamante CD, Lopez Pineda A (2019) A genetic counseling needs assessment of Mexico. Molecular genetics & genomic medicine 7(5): 1-13.
- Tata Memorial Center (2024) Basic research: Carcinogenesis, Genome Biology, and Precision Medicine.
- Apollo Hospitals (2024) Precision oncology.
- Kokilaben Dhirubhai Ambani (nd) Precision oncology.
- Ateeqh B (2024) The future of precision cancer medicine in India. Current science 126(4): 411-412.
- Chintapally N, Nuwayhid M, Arroju V, Muddu VK, Gao P, et al. (2023) State of cancer care in India and opportunities for innovation. Future Oncology 19(39): 2593-2606.
- Trapani D, Murthy SS, Boniol M, Booth C, Simensen VC, et al. (2021) Distribution of the workforce involved in cancer care: a systematic review of the literature. ESMO open 6(6): 1-10.
- Economist Impact (2023) The Future of cancer care: health system sustainability in Latin America – Argentina Pp: 1-4.
- de Paula Fonseca B, Albuquerque PC, de Freitas Saldanha R, Zicker F (2022) Geographic accessibility to cancer treatment in Brazil: A network analysis. The Lancet Regional Health Americas 7: 1-17.
- Ramli FI, Thokala P, Tong T, Unger Saldaña K (2024) Understanding breast cancer patient pathways and their impact on survival in Mexico. Journal of cancer policy 40: 100-482.
- Roldan N (2424) The failure of Insabi: cancer care dropped by 98% in public hospitals. Animal Político.
- Argentina Ministry of Health (2024) Minister Lugones headed the meeting of the Federal Health Council.
- National Health Mission (nd) National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS). Ministry of Health & Family Welfare, Government of India.
- As reported by FUTEJE in the meeting held on November 6 2024.
- Mexico General Health Council (CSG) (2020) Technical Protocol-C50 Malignant breast tumour. PT004. Commission to Define Treatments and Medicines Associated to Diseases that Cause Catastrophic Expenditures Pp: 1-53.
- IQVIA (2022) Assessment of access-to-medicine timelines in selected countries in Middle East and Africa.
- Resolución 3377/2022Boletín Oficial No. 35062 (2022).
- Diegoli H, Lopes Dias C, Massaoka MH Santana P (2023) IMFINZI® (durvalumab) in the consolidation treatment of patients with unresectable stage III non-small cell lung cancer whose disease has not progressed after platinum-based chemoradiation: Technical-Scientific Opinion with Systematic Review, Cost-Effectiveness Study and Analysis of Budget Impact Pp: 1-177.
- Méndez JS (2024) Health budget analysis towards 2030: Funding for specialty diseases. CIEP Pp: 1-45.
- IQ Oncologia Brasil (2019) Pharmaceutical industry giants join together to offer free molecular tests for patients with lung cancer.
- AMIIF (2020) non-small cel lung cancer biomarkers program.
- NHS England (2020) NHS gives cancer patients genetic test to select best treatment.
- Gil J, Fontrier AM, Miracolo A Kanavos P (2020) Access to personalized oncology in Europe. London School of Economics and Political Science Pp: 1-59.






























