Public Survey on the Knowledge and Attitudes Related to Antibiotic Use and Antibiotic Resistance in Yenagoa Metropolis
Ibegi S Ibegi, Owonaro A Peter*, Eniojukan F Joshua and Iyele Kamenebali
Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, Niger Delta University, Nigeria
Submission: March 21, 2024; Published: April 16, 2024
*Corresponding author: Owonaro A Peter, Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, Niger Delta University, Nigeria
How to cite this article: Ibegi S Ibegi, Owonaro A Peter*, Eniojukan F Joshua and Iyele Kamenebali. Public Survey on the Knowledge and Attitudes Related to Antibiotic Use and Antibiotic Resistance in Yenagoa Metropolis. JOJ Pub Health. 2024; 8(5): 555750. DOI: 10.19080/JOJPH.2024.08.555750
Abstract
Antibiotics, as a group of medications, have been subject to indiscriminate use, which is considered to be a primary factor in the development of antibiotic-resistant microorganisms, leading to complications in patients. In a bid to understand the knowledge, and attitudes of antibiotic use and antibiotic resistance in Yenagoa metropolis, a descriptive cross-sectional survey was used to assess knowledge, and attitudes relating to antibiotic use and antibiotic resistance among 408 residents of randomly selected communities in Yenagoa metropolis. An in-house questionnaire was developed and used to collect data, which was then analyzed by IBM SPSS version 27 and Microsoft Excel (version 2013), for descriptive statistics where mean, frequencies, p-values, and Kruskal Wallis test were obtained respectively. A knowledge score was determined by calculating the number of correct answers to these 10 questions. The mean knowledge score was 5.65 (SD = 2.68), and the median was 7.0. 92.4% of respondents knew that antibiotics are effective in treating bacterial infections. However, over half (62%) of respondents wrongly believe that antibiotics are effective in treating viral infections, also, 76% of respondents agreed that taking antibiotics when not necessary can increase the risk of developing antibiotic resistance.
Five questions assessed attitude towards antibiotic use. Common aspects of attitude were used as descriptors to properly ascertain the respondents’ attitude towards the subject. 86.8% of respondents displayed a good attitude toward antibiotic use, while 0.7% were classified as having a poor attitude. Over 80% of respondents believed that antibiotics should only be used when prescribed by health care professionals, similarly over 80% of the study population agreed that the prescribed dose of antibiotics should not be terminated even when they start feeling better. The test for respondents’ knowledge showed that most respondents had above-average knowledge of antibiotic use and antibiotic resistance. On the aspects of respondents’ attitudes towards antibiotics, the results obtained from the field survey revealed that generally, most residents of Yenagoa metropolis had good attitudes toward antibiotic use.
Keywords: Antibiotic use; Antibiotic resistance; Cross-sectional design; Inclusion and Exclusion Criteria; Risk of infection
Introduction
Background of Study
Antibiotic therapy is used to kill or inhibit the infecting organism without damaging the host; this is known as selective toxicity. This is commonly accomplished through the use of antibiotics [1]. Antibiotic resistance-bacterial infections that no longer respond to the drugs used to treat them-is a global health crisis of growing concern [2]. The demand for existing antibiotics is too high, which drives the evolution of resistance in pathogens the supply of new classes of antibiotics that can treat drug-resistant infections is too low, which leaves us with few treatment options for the most serious infections [3].
Antibiotics, as a group of medications, have been subject to indiscriminate use, which is considered to be a primary factor in the development of antibiotics-resistant antibiotic-resistant microorganisms, leading to complications in patients [3]. It has been reported that the abuse of antibiotics by the public is an important risk factor for antibiotic resistance [4]. There have also been reports that people are ignorant of the role of antibiotics in the management of common infections [5]. Thus, it is crucial to gain an understanding of the public knowledge and attitude towards antibiotics. This research study aims to enhance our understanding of how the public perceives antibiotics. The main purpose of this study was to understand the awareness and knowledge, residents of Yenagoa metropolis have about antibiotic use and antibiotic resistance, and how that knowledge influences their attitudes towards antibiotics.
Methodology
Study Site
Bayelsa state which is situated in the southern part of Nigeria is at the core of the Niger Delta and is encompassed on both sides by Delta and Rivers states. The capital city Yenagoa has spread to cover several sub-communities that form Yenagoa Metropolis. These communities include Igbogene, Yenigue, Akemfa, Agudama, Akempai, Edepie, Etegwe, Okutukutu, Opolo, Biogbolo, Yenizuegene, Kpansia, Yenizue-Epie, Okaka, Ekeki, Amarata, Onopa, Ovom, Swali and Azikoro.
Study Design
A quantitative cross-sectional design was used in this study.
Study Population
From the data of Nigeria’s population census done in 2006, the population of Yenagoa Metropolis was given as 138, 633. The majority of the residents here are civil servants, farmers, and artisans, it is pertinent to note that there is a great likelihood of cases of antibiotics misuse, even though it is the state capital.
Sample size determination or Power calculation
The sample size was calculated using the Yamane formula.
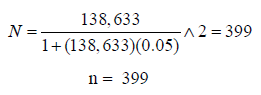
420 participants were sampled (Reason: Attrition).
Data Collection
A structured questionnaire was used as the research tool to collect the field data. The questionnaire was adapted from previous studies (André, Vernby, Berg, & Lundborg, 2010; Awad & Aboud, 2015; Alam, et al., 2023; Fang, Chen, Geng, & Kiprop, 2023) and customized to suit this research. The questionnaire had three sections with section - A structured to collect respondents’ demographic information while sections B and C were the research questions. The instrument was certified by the supervisor after a pilot study before the formal distribution to the respondents in the study area. The pilot study was conducted on 25 respondents to check for the reliability of the tool.
Data Analysis
IBM SPSS version 27 and Microsoft Excel, descriptive statistics such as frequency and mean values were used to present data and further expressed in charts.
Ethical Issues
Ethical approval was obtained from the Bayelsa State Ministry of Health as well as the participants themselves. The study was explained to all participants and informed verbal consent was obtained before conducting the interview.
Inclusion and Exclusion Criteria
Inclusion Criteria: Participants included residents who were willing to participate.
Exclusion Criteria: Residents who were not willing to participate, and individuals who were below the age of 18 years were exempted. Residents who participated in the pilot study were also exempted.
Results and Discussion
Demography of Respondents
Age of Respondents
From the results obtained, the age group 18-24 years had the highest number of respondents at 37.5%, followed by the age group 25-34 at 36%, 16% of respondents were from the age group 35-44, 5.9% of respondents were from age group 45-54, 2.2% of responses came from age group 55-64, while 1.7% of respondents came from geriatrics (65 years and above).
Gender of Respondents
From the results, 57.8% of the respondents were female, while 42.2% of the respondents were male.
Marital Status of Respondents
From the results obtained, Singles made up the highest proportion of respondents at 61.5%, respondents who were married were 31.9%, 4.4% of respondents were divorced, and 2.2% of respondents were widowed.
Education Level of Respondents
The results show that 62% of respondents were those who had attained a tertiary level of education, more so those whose highest level of education was the secondary level formed 32.8% of respondents, while 5.1% of respondents had primary education.
Occupation of Respondents
The results revealed that those in business/trading were the highest respondents in the study at 34.3%, students made up 29.7% of respondents, civil servants were also among those sampled forming 23.8% of respondents, 9.1% of respondents were unemployed, while retirees made up 3.2% of respondents.
Ethnicity of Respondents
From the results, respondents belonging to the Ijaw ethnic group were the highest in this study at 62%, respondents who were Igbos formed 15.9% of the sample population, while 9.8% of respondents belonged to the Yoruba ethnic group, respondents who were Hausa made up 3.7%, while 8.6% of respondents were of other ethnicities.
Religion of Respondents
Excerpts from the field revealed that Christians were the highest number of respondents in this study at 91.4%, 6.4% of respondents were Muslims, and 2.2% of respondents were traditionalists.
Research Questions
Research Question One: What is the knowledge of antibiotic use and antibiotic resistance among the public in Yenagoa Metropolis?
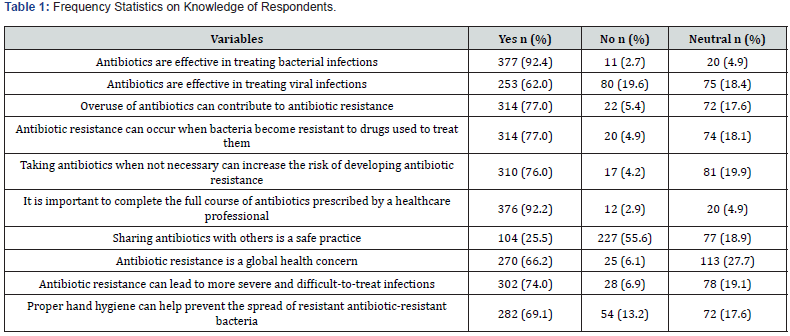
Ten questions were utilized to evaluate knowledge related to antibiotic use and antibiotic resistance. A knowledge score was determined by calculating the number of correct answers to these 10 questions. The mean knowledge score was 5.65 (SD = 2.68), and the median was 7.0. This goes to show that most of the respondents have a good level of knowledge of antibiotic use and antibiotic resistance.
A large proportion (92.4%) of respondents knew that antibiotics are effective in treating bacterial infections. Over half (62%) of respondents wrongly agreed by saying yes to the statement; that antibiotics are effective in treating viral infections (e.g., common cold, flu). 77% of the respondents correctly answered the statement; that the use of antibiotics can contribute to antibiotic resistance. Over half (55.6%) of respondents correctly disagreed by answering no to the statement; that the sharing of antibiotics is a safe practice, although over 25% agreed that it is a safe practice. Over three-quarters (77%) of respondents correctly agreed by saying yes to the statement, that antibiotic resistance can occur when bacteria become resistant to the drugs used to treat them. Also, 76% of respondents agreed that taking antibiotics when not necessary can increase the risk of developing antibiotic resistance, and a large proportion (92.2%) of respondents knew that it is important to complete the full course of antibiotics prescribed by a healthcare professional. Over half (66.2%) of respondents agreed that antibiotic resistance is a global concern (Table 1).
Inferential statistics on knowledge showed that there are significant differences for the following demographic variables - marital status, and educational level. A linear regression was carried out, which showed that widowed respondents were 0.17 times less likely to have good knowledge about antibiotic use and antibiotic resistance. Also, it showed that respondents who had attained a tertiary level education were 0.8 times more likely to have good knowledge.
Research Question Two: What attitude does the general public have towards antibiotics in the Yenagoa metropolis?
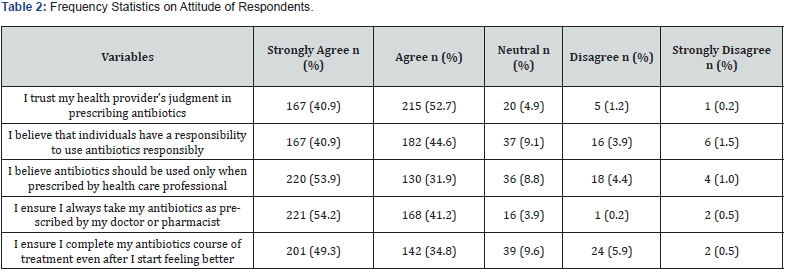
Five questions assessed attitude towards antibiotic use. Common aspects of attitude were used as descriptors to properly ascertain the respondents’ attitude towards the subject. The respondents were required to indicate their level of agreement with issues around their attitude toward antibiotic use. The data collected were carefully rated on a 5-point Likert scale, which was converted into a mean score of over 5, then classified as poor attitude (1 - 2 33), moderate attitude (2.34 - 3.67), and good attitude (3.68 - 5.00). From the results, 86.8% of respondents displayed a good attitude toward antibiotic use, while 0.7% were classified as having a poor attitude (Table 2).
Inferential statistics for respondents’ attitudes indicated significant differences in attitudes of respondents in various demographic variables including, age and marital status. As indicated by their p-values which were all less than 0.05. A logistics regression was carried out to identify specific areas where these differences exist. For the age group, it indicated that respondents in the age group 35-44 were 1.2 times less likely to have a good attitude towards antibiotics compared to the 18-24 age group. For marital status, it showed that respondents who were divorced or widowed were 1.6 times and 1.09 times less likely to have a good attitude towards antibiotics when compared to single respondents respectively.
Discussion
This study investigated the knowledge and attitudes related to antibiotic use and antibiotic resistance in the Yenagoa metropolis of Bayelsa State in Nigeria. The key findings of the study are discussed below.
Knowledge of Respondents on Antibiotics Use and Antibiotics Resistance
Findings showed that 92.4% of respondents had appropriate knowledge regarding antibiotics being effective in treating bacterial infections, this corroborates the findings of [6,7], in which the majority of respondents believed that antibiotics are effective in treating infections caused by bacteria. On the other hand, 62% of the respondents did not know that antibiotics are not effective against viruses which are similar to the proportions (47-70%) reported from Britain, Europe, Denver, Wisconsin, Minnesota, the Republic of Georgia, New Jersey, Netherlands, Qatar and India [6,8-10], (Filipetto, Modi, Weiss, & Ciervo, 2008; Grigoryan, et al., 2023; Kandelaki & Marrone, 2015; McNulty, Boyle, Nichols, Clappison, & Davey, 2007b; Wilson, Crane, Barrett, & Gonzales, 1999). A possible reason for this knowledge gap could be due to the words used; ‘bacterial’ and ‘viral’. Respondents may lack adequate knowledge to differentiate between diseases that are caused by bacterial infections and viral infections.
Regarding overuse of antibiotics being a factor that contributes to antibiotic resistance, 77% of respondents knew that antibiotic overuse can result in antibiotic resistance, which is higher than the proportions (67%) reported by [7]. With regards to what antibiotic resistance implies, 77% of the respondents knew that antibiotic resistance occurs when bacteria become resistant to drugs used against them, indicating that the majority of respondents were aware that it is the bacteria that develop resistance, according to the World Health Organization (2023), antibiotics resistance occurs when bacteria change in response to the use of these medicines. Bacteria, not humans or animals become “antibiotic-resistant”.
Furthermore, on the unnecessary use of antibiotics resulting in antibiotic resistance, 76% of respondents knew that taking antibiotics when not necessary can increase the risk of developing resistance. Similarly, studies in Norway and Saudi Arabia found that a high percentage of respondents knew that unnecessary use of antibiotics can lead to resistance against them, with more than 90% awareness in Norway [11] and around half of the respondents in Saudi Arabia [12]. On the importance of completing the full course of antibiotics, over 92% of respondents agreed that it is important to complete the full course of antibiotics prescribed by healthcare professionals, this is higher than a study by [13] in Ethiopia that found that about 70.8% of respondents were aware that sharing antibiotics with others is a risk factor for antimicrobial resistance.
About 74% of respondents agreed that antibiotic resistance results in more severe and difficult-to-treat infections. The CDC emphasizes that resistant infections can be difficult and sometimes impossible to treat [2], therefore antibiotic resistance does result in more difficult-to-treat infections, posing a threat to public health and modern medicine. A good proportion of the respondents had appropriate knowledge that good hand hygiene can reduce the spread of antibiotic-resistant bacteria, 69.1% of respondents agreed that proper hand hygiene can help to prevent the spread of antibiotic-resistant bacteria. According to [14], proper hand hygiene is the single most important, simplest, and least expensive means of reducing the prevalence of healthcareassociated infections and the spread of antibiotic resistance.
Attitude of Respondents towards Antibiotics
Regarding the aspects of respondents’ attitude towards antibiotics, the results obtained from the field survey revealed that generally, most residents of Yenagoa metropolis have a good attitude towards antibiotic use. In this study, about 90% of respondents say they trust their healthcare provider’s judgment in prescribing antibiotics, this is unlike a study by Munthe & Havstrom (2022), which found that 18% of respondents indicated they had obtained antibiotics without a prescription, and 16% would consider doing so, often due to dissatisfaction with or lack of healthcare trust. It is important to note that trust does not always correlate with lower expectations for antibiotics, as greater trust seemed to boost the effect of information provision in reducing inappropriate antibiotics expectations in some cases according to [15]. This suggests that while trust in healthcare providers is important, it may not always lead to appropriate antibiotic prescribing. Therefore, healthcare providers must engage in antibiotic stewardship and for patients to be educated on appropriate antibiotic use [15,16].
A good proportion of respondents had an appropriate attitude towards completing the antibiotics course of treatment. Over 80% of the study population agreed that the prescribed dose of antibiotics should not be terminated even when they start feeling better which is higher than findings (70%) from [9] and higher than reports from other surveys which reported 34% [10]. Understanding this concept is important because premature discontinuation of antibiotics puts an individual at risk of infection relapse, colonization with antibiotic-resistant organisms, and complicated disease outcomes [17]. Antibiotic concentrations in the body that are subinhibitory resulting from incomplete dosage regimens may lead to the development of antibiotic resistance [18].
Findings from the study also showed that over 80% of respondents believed that antibiotics should only be used when prescribed by health care professionals, this is higher than findings from a study in India, conducted by [19], where 67% of respondents exhibited an appropriate attitude towards obtaining antibiotics with a doctor’s prescription. Antibiotics are designed to treat specific bacterial infections and should not be used to treat conditions for which they are not prescribed. The Centre for Disease Control emphasizes that antibiotics should only be taken if needed and exactly as prescribed by a doctor [20]. The Cleveland Clinic also states that in the United States of America, a prescription from a healthcare provider is required to legally obtain oral antibiotics, and this is for the patient’s safety and protection [21].
Conclusion
After a detailed study of the knowledge and attitudes related to antibiotic use and antibiotic resistance in the Yenagoa metropolis of Bayelsa State in Nigeria, several truths were uncovered. First, the study was able to uncover that people wrongly believe that antibiotics are effective in treating viral infections like the common cold and flu. Secondly, residents of Yenagoa metropolis generally have a good attitude towards antibiotics [22-25]. The results of this study have identified some areas of misconceptions and specific groups to be targeted for interventions. There is an urgent need for initiatives that enhance comprehension regarding the appropriate use of antibiotics, focusing particularly on groups where misunderstandings about their usage are widespread.
Recommendations
i. The government should sponsor a national survey to understand the knowledge, attitude, and practice among Nigerians, to provide insight into the variations and knowledge gaps that may be peculiar to a particular region.
ii. Government should conduct public campaigns aimed at educating the public about the difference between bacterial and viral infections, and that antibiotics are not effective against viral infections.
Acknowledgment
The researchers appreciate the statistician, respondents, and co-researchers for the time.
Conflict of Interest
The researchers declare that there was no conflict of interest.
References
- Leekha S, Terrell CL, Edson RS (2011) General principles of antimicrobial therapy. Mayo Clin Proc 86(2): 156-167.
- Centers for Disease Control and Prevention (2022) Antimicrobial Resistance.
- Ventola CL (2015) The antibiotic resistance crisis: part 1: causes and threats. P T 40(2): 277-283.
- Melander E, Ekdah K, Jonsson G, Molstad S (2000) Frequency of penicillin-resistant pneumococci in children is correlated to community utilization of antibiotics. Pediatr Infect Disease J 19(12): 1172-1177.
- Wise R, Hart T, Cars O, Streulens M, Helmuth R, et al. (1998) Antimicrobial resistance is a major threat to public health. BMJ 317(7159): 609-610.
- Cals JW, Boumans D, Lardinois RJ, Gonzales R, Hopstaken RM, et al. (2007) Public beliefs on antibiotics and respiratory tract infections: an internet-based questionnaire study. Br J Gen Pract 57(545): 942-947.
- Munana C, Kirzinger A, Lopes L, Hamel L, Brodie M (2019) Data Note: Public Awareness Around Antibiotic Resistance.
- Belongia E, Naimi T, Gale C, Besser R (2002) Antibiotic use and upper respiratory infections: a survey of knowledge, attitudes, and experience in Wisconsin and Minnesota. Prev Med 34(3): 346-352.
- Moienzadeh A, Massoud T, Black E (2015) Evaluation of the general public's knowledge, views and practices relating to appropriate antibiotic use in Qatar. Int J Pharm Pract 25(2): 133-139.
- Rao M (2016) Assessment of public knowledge and attitudes regarding antibiotic use in a tertiary hospital. Assessment 9(1).
- Waaseth M, Abdifatah A, Røen I, Eriksen K, Stanojevic T, et al. (2019) Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers - a cross-sectional study. BMC Public Health 19(1): 66.
- Shatla M, Althobaiti F, Almqaiti A (2022) Public Knowledge, Attitudes, and Practices Towards Antibiotic Use and Antimicrobial Resistance in the Western Region of Saudi Arabia. Cureus 14(11): e31857.
- Simegn W, Moges G (2022b) Awareness and knowledge of antimicrobial resistance and factors associated with knowledge among adults in Dessie City, Northeast Ethiopia: Community-based cross-sectional study. PLoS One 17(12): e0279342.
- Mathur P (2011) Hand hygiene: back to the basics of infection control. Indian J Med Res 134(5): 611-620.
- Thorpe A, Sirota M, Juanchich M, Orbell S (2020) Always take your doctor’s advice’: Does trust moderate the effect of information on inappropriate antibiotic prescribing expectations? Br J Health Psychol 25(2): 358-376.
- Centers for Disease Control and Prevention (2021a) Antibiotic Prescribing and Use: Antibiotic Do's & Don’ts.
- Carey B, Cryan B (2003) Antibiotic misuse in the community - a contributor to resistance? Irish Med J 96(2): 43-44.
- Austin D, Kristinsson K, Anderson R (1999) The relationship between the volume of antimicrobial consumption in human communities and the frequency of resistance. Proc Natl Acad Sci 96(3): 1152-1156.
- Khyati B, Suchitra SM, Shrikala BB, Unnikrishnan B, Shantharam B (2021) Knowledge, attitude, and practices related to antibiotic use and resistance among the general public of coastal south Karnataka, India: A cross-sectional survey. Clin Epidemiol & Glob Health 11: 100717.
- Centers for Disease Control and Prevention (2021b) Antibiotic Prescribing and Use: Outpatient.
- Cleveland Clinic (2023) Antibiotics.
- Ajzen I (1991) The theory of planned behavior. Organizational Behavior and Human Decision Processes 50(2): 179-211.
- Ajzen I, Fishbein M (2005) The influence of attitudes on behavior. In Albarracin D, Johnson B, & Zanna M (Eds.), The handbook of attitudes, Lawrence Erlbaum, Mahwah NJ, pp. 173-221.
- Jean MV, Natasha SH (2017) Principles of Infectious Diseases: Transmission, Diagnosis, Prevention, and Control. International Encyclopedia of Public Health 2nd edition, Ref Module BioMed Sci 22-39.
- Scully JL (2004) What is a disease? EMBO reports 5(7): 650-653.






























