17 May WORLD HYPERTENSION DAY Measuring BP and Managing Hypertension- A Call to Action Challenges in Developing countries- India case
K Suresh*
Family Physician & Public Health Consultant, Bengaluru, India
Submission: May 21, 2023; Published: August 29, 2023
*Corresponding author: Suresh Kishanrao, Family Physician & Public Health Consultant, Bengaluru, India
How to cite this article:K Suresh. 17 May WORLD HYPERTENSION DAY Measuring BP and Managing Hypertension- A Call to Action Challenges in Developing countries- India case . JOJ Pub Health. 2023; 7(5): 555725. DOI: 10.19080/JOJPH.2023.07.555725
Abstract
In between this World Hypertension Day on May 17, 2023, with the theme as “Measure Your Blood Pressure Accurately, Control It, Live Longer”, and World Family Doctor Day on 19 May 2023, I write this article to focus on accurate blood pressure measurement equipment and methods and to combat low awareness among people about Hypertension in developing countries mainly, India. When the pressure of the blood against blood vessel walls is too strong it is called hypertension. Our blood pressure changes throughout the day based on our activities. Hypertension is a condition of systolic and or diastolic pressure that is higher than normal. WHO defines Hypertension as a condition when the pressure in our blood vessels is systolic blood pressure (SBP)140 and Diastolic blood pressure (DBP) 90 mm Hg or higher.
All people with high blood pressure may not feel symptoms. The only way to know is to get your blood pressure checked. High blood pressure can cause damage to the vessels when left untreated and lead to other problems, like heart disease, stroke, and kidney disease. Hypertension was identified as one of the nine modifiable risk factors (along with smoking, lipids, diabetes, obesity, diet, physical activity, alcohol consumption and psychosocial factors) contributing to more than 90% of the risk of Acute Myocardial Infarction (AMI) in the INTERHEART study conducted in 52 countries nearly 2 decades ago.
In developing countries including India Blood pressure is measured by primary care doctors or nursing staff in major institutions and trained field research workers in community research like National Family Health Surveys (NFHS 1 to 5) and other screening programs. Accurate measurement of BP using the standardized BP measurement technique is essential to control the rising prevalence of hypertension. To mitigate the risk, high BP must be managed effectively and for this it must be measured accurately. Replacement of mercury sphygmomanometers by Digital equipment has resolved most of the problems in the last decade.
This article is the outcome of authors personal observation of measuring BP by cardiologists, general practitioners and paramedical staff and researchers in the field work and self-experience. Factors like the physical and mental status of the client, quality of equipment, skills of the service provider, the environment in which BP is measured influence the outcome (readings) and guide the management practices. Diagnosing hypertension among young (20-40 years) and Postural hypotension among diabetics is a challenge to confirm and manage. American Diabetes Association’s (ADA) January 2023 Standards of Care addresses the role of weight loss in diabetes management and cardiovascular risks and now advises lower targets for blood pressure and LDL cholesterol.
The 2023 Standards update the definition of hypertension for people with diabetes as a systolic blood pressure at least 130 mm Hg or diastolic BP at least 80 mm Hg, which is the definition used by the American College of Cardiology and the American Heart Association. Blood pressure below 130/80 mm Hg is the recommended treatment goal, with drug therapies considered for people with diabetes and hypertension.
Keywords: Blood Pressure (BP); Hypertension (High BP); manual sphygmomanometer; Digital BP apparatus; Postural Hypotension; Orthostatic hypotension; National Family Health Survey (NFHS), American Diabetes Association (ADA); American College of Cardiology (ACC); American Heart Association (AHA)
Materials and Methods
Three case reports, one each of hypertensive elderly self, an elderly lady with postural hypotension due to atrial fibrillation and a young Banking professional of 37 years with Hypertension on weekdays. Observing the process of monitoring of BP by 3 cardiologists (one each in Delhi, Gulbarga, and Bengaluru), multiple general duty doctors and health workers in Primary health care and private clinics and research assistants in multiple field surveys. The literature review of the progress from mercury sphygmomanometers since 1968 to digital equipment in the last one decade.
Introduction
World Hypertension Day was celebrated this year on May 17, 2023, with the theme as “Measure Your Blood Pressure Accurately, Control It, Live Longer”, focusing on combatting low awareness rates and accurate blood pressure measurement methods [1]. This worldwide activity was created by the World Hypertension League (WHL), first on May 14, 2005-, with the theme: Know Your Numbers! [1]. World Family Doctor Day is an annual global event celebrated on May 19 to recognize the role and contributions of family doctors in providing comprehensive and continuous healthcare to individuals, families, and communities. The day is a way to highlight the importance of primary healthcare in promoting health and well-being for all [2].
The purpose of celebration of both these days is to communicate to the public the importance of hypertension and its serious medical complications and opt lifestyle changes for prevention on one hand and to provide information on proper detection, treatment, and prevention to health professionals at Primary Care level. This action appears simple but is very challenging as measuring BP is not subjected to regulatory standards. It is possible by only motivating health professionals, hospitals, media, volunteer organizations, people at large and government in each country [3].
Definition
When the pressure of the blood against blood vessel walls is too strong it is called hypertension. Our blood pressure changes throughout the day based on our activities. Having blood pressure measures consistently above normal may result in a diagnosis of high blood pressure. WHO defines Hypertension as a condition when the systolic blood pressure (SBP) of 140 and Diastolic blood pressure (DBP) 90 mm Hg or higher in our blood vessels [3]. The ADAs 2023 Standards update the definition of hypertension for people with diabetes as a systolic blood pressure at least 130 mm Hg or diastolic BP at least 80 mm Hg, which is the definition used by the American College of Cardiology and the American Heart Association. Blood pressure below 130/80 mm Hg is the recommended treatment goal, with drug therapies considered for people with diabetes and hypertension. All people with high blood pressure may not have symptoms. The only way to know is to get our blood pressure checked. High blood pressure can cause damage to the vessels when left untreated and lead to other problems, including heart disease, stroke, and kidney disease [1].
Causes of high blood pressure: It’s not clear exactly what causes high blood pressure. But there are personal issues like being overweight (BMI), eating too much salt, not eating enough fruit and vegetables, not enough physical exercise, drinking too much alcohol or coffee or other caffeine-based drinks, smoking or chewing tobacco, stress, age over 65, family history of hypertension, living in a deprived area, and having medical conditions like, diabetes, long-term kidney infections, sleep apnoea, glomerulonephritis and atherosclerosis (thickening or hardening of the arteries caused by a build-up of plaque in the inner lining of an artery- due to high cholesterol and triglyceride levels), or narrowing of the arteries supplying the kidneys are the causes of Hypertension [1].
The International Society of Hypertension recommends an “essential” BP target of < 140/90 for most individuals, and for those under 65, they provide the option of an “optimal” BP of < 130/80. The American Diabetes Association this year revised its target BP to < 130/80 for people with diabetes, for prevention of recurrent stroke. The American Heart Society (AHA) and American Stroke Association (ASA) in 2021 recommend BP < 130/80, and the International Society for Hypertension as well as the AHA recommends a BP of < 130/80 for atherosclerotic cardiovascular disease patients.
Lower targets can lead to a significant increase in adverse events, like syncope and hypotension, with a relative risk of 1.44, and a nominal increase in serious adverse events like hospitalization or disability or death. This reflected an absolute risk increase of 3% compared with the standard target group (specifically 9.8% vs 6.8%). Another potential harm of low BP targets was the need for an average of one additional medicine to reach lower BP targets. One systematic review cited an eightfold higher withdrawal rate due to adverse events in the lower target BP groups [4].
This article is based on three case reports, one each of hypertensive elderly self, an elderly lady with postural hypotension due to atrial fibrillation and a young Banking professional of 37 years with Hypertension on weekdays. Observing the process of monitoring of BP by 3 cardiologists (one each in Delhi, Gulbarga, and Bengaluru), multiple general duty doctors and health workers in Primary health care and private clinics and research assistants in multiple field surveys. The literature review of the progress from mercury sphygmomanometers since 1968 to digital equipment in the last one decade.
Case Reports
Autobiography
Having undergone Post CABG angioplasty in February 2023, I went to my cardiologist for follow-ups in March and April 2023. Both times I drove just about 1 km from my home late in the evening, and the first check-ups in both visits recorded high systolic and diastolic blood pressure (146/96 & 150/92 respectively). In March self BP check at home before I left home read 132/68. After recording 146/96 the first reaction of the cardiologist was that he was not happy with BP control, as I reported that I was taking only Tab Embeta Xr 25 mg (Metoprolol- a Beta-blocker) and stopped the other drugs (Tab. Cardace 2.5mg- containing Ramipril) out of his prescription as I was feeling giddy due to hypotension (96- 110/56-60) in the initial fortnight. A second check both the times after resting for about 20-30 minutes gave readings well within the ranges he intended (130/80) and I recorded at home most of the days (108-118/ 56-68).
After the CABG operation in June 2005, my BP was well under control with Embeta Xr 25 mg only, though for the first year I had taken Cardace 2.5 mg also. I am a diabetic since 1991 and that too under good control with diet, exercise, and oral anti-diabetics (Amaryl 3mg and Glycomet SR 500 mg before and after lunch and dinner respectively). Tab Gibtulio (Empagliflozin- SGLT2 inhibitor agent as it inhibits SGLT2 in kidney, leading to increase in urinary glucose excretion and reduction in blood glucose) 10 mg in the morning since 2022 was added to the above list and increased to 25 mg daily in the morning after angioplasty since last 2 month for both heart and diabetes benefit.
A Case of Postural hypotension
One of my patients, a lady aged 62 years known hypertensive and diabetic for over decade on Beta blockers twice a day, felt giddy in the forenoon for a week in July 2022. On checking BP, the readings- were: Supine position- 148/69, sitting- 148/68 and standing – 121/52. BP was measured three times, at 1 min intervals, after 5 min of seated rest and on standing, using an automated cuff sphygmomanometer. Postural hypotension (PH), the reduction in blood pressure when rising from sitting or lying to standing, is a risk factor for falls, cognitive decline, and mortality.
A Case of Hypertension in a young Banking Professional:
A 37-year-old male presented to me in September 2022 with the chief complaints of weakness of all the four limbs for the last 5 months, mostly on all working days of the week. On weekends he was fine. On examination he looked like any average built, well-nourished educated young man. General examination revealed no sensory and cranial disturbances, but there was some pallor. Family history of his both parents in mid-60’s age were hypertensive and diabetics for over a decade and were under my care for 5 years but neither BP nor Blood sugar was under good control.
The first BP recorded on a Friday evening on his return from his Banking work was 152/98 mm Hg. A repeat check after 30 minutes of resting the BP was 142/94. BP taken in both arms in three positions of supine, sitting and standing gave almost similar readings. Without rushing to put him on drugs I asked him to return on Sunday morning. Around 0730 AM on Sunday the BP was recorded again in all three positions. Surprisingly, all records were well within acceptable limits, SBP around 136-138 and DBP around 86-88 mm of Hg.
A detailed history of the work schedule revealed that everyday tallying the balance sheet of transaction was onerous and stressful. I followed this young man for another 2 days in the next week with BP recordings showing SBP -138-142 and DBP 88-94, and the week-end readings just as previous weekend, leading me to diagnose as a case of young Hypertensive due to the professional stress and family history. I put him on METOLAR TL 50MG TABLET (a combination of Metoprolol and Telmisartan) once in the morning and asked him to reduce salt intake and improve fluids intake even in the office. The blood pressure came under control within 3 weeks, and he continues to take the tablet is fine.
Public Health Concern
As a Public health professional, I am more concerned about the incidence and prevalence rates estimated from all field surveys. Though home level use and equipment use in community surveys has shifted to digital equipment in the last decade in India, the testing environment and validation of equipment that decide the accuracy of monitoring, and hence incidence / prevalence rates may to be conducive all the time as home and neighbouring people congregate around any individual being examined. Therefor I suspect the HHTN estimations from community surveys or clinical practices may be underestimated or overestimated, and the program monitoring changes reported for better over time, may be misguiding as they depend upon the quality of equipment’s used.
Discussion
Magnitude of the Problem
India: India has set a target of 25% relative reduction in the prevalence of hypertension under Universal Health Coverage by 2025. Of the estimated 220 million people in India living with hypertension, only 12% have their blood pressure under control. Hypertension is a significant contributor to mortality in India. Achieving better hypertension control rate at the population level is critical in reducing cardiovascular morbidity and mortality. It is estimated that at least 25% adults in India have hypertension, only half of them know and only half of those who know and are taking medication have their blood pressure under control.
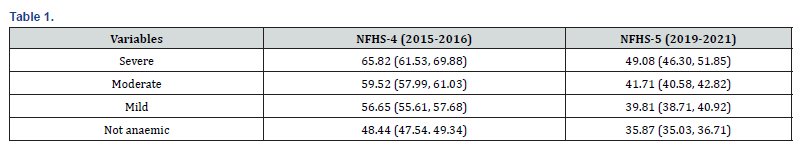
A systematic review and meta-analysis of community-based, non-interventional studies published after 2001 till 2022. It included 51 studies (n = 338,313 hypertensive patients). 21 studies (41%) reported poorer control rates among males than females, and six studies (12%) reported poorer control rates among rural patients. The pooled hypertension control rate in India during 2001–2020 was 17.5% with significant increase over the years, reaching 22.5% in 2016–2020. Sub-group analysis showed significantly better control rates in the South and West regions, compared to north, central and eastern regions. It also points to significantly poorer control rates among males compared to females [5]. National Family Health Survey (NFHS) 5, there has been decline of 12.57 to (16,72 percentage points in severe HT, 17.81 percentage points in moderate HT,16.84% in mild HT about 12.57 % in non-anaemic HT individuals) over period of 5 years between 2019-21 and 2015-16 [6] (Table 1).
The prevalence of hypertension among individuals aged 15 to 49 years was 22.8% (n = 172,532), out of which 52.06% were newly diagnosed cases. In contrast, in NFHS-4, the prevalence of hypertension among same age group was 20.4% (n = 153,384), of which 41.65% were newly diagnosed cases. In NFHS-5, 40.7% of the previously diagnosed cases were on BP-lowering medications compared to 32.6% in NFHS-4. In NFHS-5, controlled BP was observed in 73.7% of the patients on BP-lowering medication compared to 80.8% in NFHS-4. Females compared to males (a OR = 0·72 and 0·007) [7] (Table 2). The limitation of this national data is it pertains to only 15–49-year-old population and based on BP recording by short, trained research workers.

A nationally representative cohort study of the middle-aged and older Indian population, the Longitudinal Aging Study in India (LASI), data from the 2017–2019 baseline wave (N = 72,262) and the 2010 pilot wave (N = 1,683), the estimated prevalence (Hypertension self-reported physician diagnosis or elevated blood pressure (BP) on measurement, of SBP ≥ 140 mm Hg or D BP ≥ 90 mm Hg.) for the population aged 45 years and older was 45.9%[8,10] . Among hypertensive individuals, 55.7% had been diagnosed, 38.9% took antihypertensive medication, and 31.7% achieved BP control. In multivariable logistic regression models, access to public healthcare was a key predictor of hypertension treatment (odds ratio [OR] = 1.35, p = 0.001), especially in the poorest group.
Having health insurance was not associated with improved hypertension awareness among those with low and middle socio-economic status population but it was significant among high socio-economic status group. Comparing hypertension awareness, treatment, and control rates in the 4 pilot states, a statistically significant (p < 0.001) improvement in hypertension management was found from 2010 to 2017–2019. Although considerable variations in hypertension diagnosis, treatment, and control exist across different sociodemographic groups and geographic areas, reducing uncontrolled hypertension remains a public health priority in India. Access to healthcare is closely tied to both hypertension diagnosis and treatment. The limitations of this study include the pilot sample being relatively small and that it recruited from only 4 states [8-10].
Another challenge is of young-onset hypertension is a common, in India in the last 2 decades that has increased all-cause mortality and results in subclinical organ damage early in its natural history. In the absence of the evidence of blood pressure lowering in young adults in terms efficacy of antihypertensive therapy in mild grades of hypertension, referral of selected patients by the primary care Physicians to secondary care is suggested for more detailed assessment, evaluation of subclinical organ damage, and investigation of secondary causes of hypertension [11].
The ACC/AHA lowered the diagnostic threshold for stage 1
hypertension in the 2017 Guidelines from 140/90 to 130/80 mm
Hg across all age categories to some controversy. The indications
to refer Young-Onset Hypertension to Secondary Care include
i. Age <30 yrs. with no risk factors
ii. Resistant hypertension
iii. Sudden deterioration in BP control
iv. Evidence of end-organ damage
v. Clinical features or investigations suggesting a secondary
hypertension [11-13].
Prevalence of HTN in Young population
The prevalence of hypertension in the young adult population (20-40 years) is rising in India. Increased arterial stiffness due to RAAS activation and increased sympathetic overactivity due to stress have been implicated as primary factors for the same. A cross sectional observational survey using a structured questionnaire conducted online with 2287clinicians (cardiologists, diabetologists, consultant physicians and family physicians) indicated that the prevalence of hypertension was 10- 30% as per opinion of about 65% clinicians. The top three risk factors for hypertension in young were perceived to be smoking, mental stress and obesity. Majority (58%) respondents opined that both increased heart rate and systolic blood pressure were markers of sympathetic overactivity.
More than 60% respondents across specialities telmisartan were the preferred ARB by >80% respondents, to treat hypertension in young adults. Similarly, Metoprolol was the preferred beta blocker by about 2/3 of clinicians was to address sympathetic overactivity. Telmisartan & Metoprolol single pill combination achieved the BP goal in 40-60% of patients and was well tolerated in young hypertensive patients. As of now Hypertension is affecting 1 in 8 adults aged between 20 and 40 years [11]. This number is expected to escalate with lifestyle behaviours and lowering of hypertension diagnostic thresholds to SBP/DBP of 130/80 mm Hg. Age, alcohol, smoking and chewing tobacco, BMI, central obesity (defined as waist circumference >90 cm in men and >80 cm in women), consumption of low vegetables/fruits, high consumption of dietary fat and salt, and sedentary activity are the significant risk factors for HTN among Indian patients [11-13].
This study points to the fact that initiation of an early and appropriate antihypertensive treatment in young population will lower the burden of cardiovascular disease as young adults with hypertension before the age of 40 are at a high risk of developing cardiovascular events.
In a retrospective observational study at Tata Main Hospital, Jamshedpur, Jharkhand, for 5 years between April 2015 and March 2020, of patients admitted for acute coronary syndrome or chronic stable angina, aged ≤40 years, who underwent coronary angiography. Among the 117 cases 81.2% were males and 18.8% were females. Majority of cases, (52.2%) were in the age group of 36–40 years. Risk factor evaluation showed hypertension as the major risk factor, present in 30.76% of patients, followed by diabetes mellitus in 21.36%, Dyslipidaemia in 7.6%. History of smoking was present in 8.54%, history of smokeless tobacco use was in 7.69%, family history of CAD was noted in 9.4% of patients [13].
Postural Hypertension
A Systematic review, meta-analyses, and meta-regression in 2019 studies based in primary, community, or institutional care settings reported pooled prevalence’s for postural hypertension (PH) using the consensus definition- were 17% for 34 community cohorts, 19% for 23 primary care cohorts and 31% for 3 residential care or nursing homes cohorts (P = 0.16 between groups). By condition, prevalence’s were 20% with hypertension (20 cohorts), 21% with diabetes (4 cohorts), 25% with Parkinson’s disease (7 cohorts) and 29% with dementia (3 cohorts), compared to 14% without these conditions (P < 0.01 between groups). Multivariable meta-regression modelling identified increasing age and diabetes as predictors of PH (P < 0.01, P = 0.13, respectively; R2 = 36%).
PH prevalence was not affected by blood pressure measurement device (P = 0.65) or sitting or supine resting position (P = 0.24) [14-16]. The symptoms associated with delayed OH were fatigue on exertion, unsteadiness of gait, neck pain on prolonged standing, and recurrent falls [14-16]. The symptoms are due to hypoperfusion secondary to fall in BP in upright posture. Visual blurring is due to retinal or occipitallobe ischemia, and suboccipital neck pain, posterior cervical, and shoulder region is due to ischemia in the trapezius and neck muscles.
Orthostatic hypotension is defined as a sustained decrease in systolic blood pressure of 20 mm Hg or a decrease in diastolic blood pressure of 10 mm Hg within three minutes of standing compared with blood pressure from the sitting or supine position or by head-up tilt-table testing (1). When sustained blood pressure (BP) drop is after three minutes of upright posture it is called delayed orthostatic hypotension (delayed OH) [13,14].
In a pilot study, first in India of 170 patients’ Orthostatic hypotension was seen within 3 minutes in 70 patients, fifty patients had delayed OH (BP fall after 3 minutes). There were 27 males and 23 females in this group. Asymptomatic OH was more common in patients who developed OH after 10 minutes. Ideally the recordings must be obtained from both the hands and feet. The beat-to-beat BP recording permits determination of role played by sympathetic nervous system. It detects the baroreflex sensitivity. It accurately reflects the arterial BP [13].
In another community-based cross-sectional study of randomly selected 240 community-dwelling elderly from Thiruvananthapuram, Kerala reported the prevalence of OH and frailty among participants was 9.6 and 29.2 percent respectively. In the first minute, OH was associated with increased odds of falls (OR = 1.97). Increase in number of co-morbidities (ORadj = 1.82) number of medicines used (ORadj = 1.73), and orthostatic intolerance (ORadj = 3.67 increased the odds of having OH. Elderly with diabetes (ORadj = 4.81), hypertension (ORadj = 4.97 and cognitive impairment (ORadj = 5.01 were at a higher odd of having OH [14-16].
Migraine & Headache
Persons who suffer severe headaches or migraines are 25% more likely to develop hypertension in comparison to those who do not have a history of migraine, suggests a study published in the journal Nutrition, Metabolism & Cardiovascular Diseases. The risk was higher among women than in men. Data from 5716 adults from the 1999-2004 National Health and Nutrition Examination Survey (NHANES) was analysed in this cross-sectional study.
Out of the 5716 participants, 1134 (19.8%) reported migraine or severe headaches. Younger females and those with higher BMI were more likely to experience migraine. Those who reported migraine also had lower dietary potassium and calcium intake, lower serum total cholesterol, creatinine, and hemoglobin, high estimated glomerular filtration rate (eGFR) and lower educational status compared with those without migraine. After adjusting for confounding variables, participants with migraine or severe headaches were at 25% increased risk of developing hypertension with odds ratio (OR) of 1.25.
On subgroup analyses, a positive association between migraine or severe headache and hypertension was noted in women (OR 1.39), participants with a lower BMI (≤25 kg/m2) (OR 1.51) and those without diabetes (OR 1.27). This study has demonstrated a positive correlation between migraine and hypertension and the urgent need of management of migraine to prevent onset of hypertension in this population group . In developing countries including India Blood pressure is measured by primary care doctors or nursing staff in major institutions and trained field research workers in community research like National Family Health Surveys (NFHS 1 to 5) and other screening programs.
Accurate measurement of BP using the standardized BP measurement technique is essential to control the rising prevalence of hypertension. To mitigate the risk, high BP must be managed effectively and for this it must be measured accurately. Recently, 13 scientific global health organizations jointly published a consensus statement on standardized clinic BP measurement in the May 2023 issue of the American Journal of Medicine. The consensus statement has outlined four steps for implementing standardized clinic BP measurement relating to the i) equipment and the facility where BP is to be measured, ii) staff measuring the BP, iii) patient preparation, and iv) the procedure of measurement. It describes the four big ways-BP measurement-goes-wrong-andhow- tackle-them [17,18]. It has issued a “call to action” for all stakeholders to overcome the barriers to the implementation of standardized clinic BP measurement. We in India must look at these precautions and respond to the call of action.
Several factors influence the measurement of BP. These
factors are:
i. Patient-related (such as drinking tea/coffee or engaging
in physical activity just before measurement, acute meal ingestion,
slouching, unsupported back/feet/arm, sitting with crossed legs,
talking including on the phone, full bladder,
ii. Procedure-related (patient’s legs are crossed at the
knees, patient is talking, the arm is lower than heart level),
iii. Physician-related (talking, using a wrong cuff size, tying
the cuff over clothing, not taking multiple measurements)
iv. Equipment-related (non-validated automated devices,
too small or too large cuff) [2].
These factors yield readings that may be inaccurate and therefore unreliable. The consequences are missed diagnosis and therefore delayed or no treatment or inappropriate treatment. Attaining the treatment goals is difficult on account of the highly variable readings. Standardized measurement of office BP is essential to reduce errors. Inaccurate blood pressure measurement could lead to incorrect diagnosis and inappropriate treatment. The chance to reduce the risk of heart attack or stroke could also be missed. The solutions suggested are:
Equipment and the facility where BP are to be measured: The BP should be measured in a quiet room with a clinically validated BP device by trained healthcare professionals using an appropriately sized cuff over the bare upper arm. An automated device is recommended to eliminate the “human error associated with manual devices”. Replacement of mercury sphygmomanometers by Digital equipment has resolved most of the problems in the last decade [18,19]. Top BP machines used in Inda include Dr Morepen bp one bp 02 bp monitor, Dr. Trust smart talking bp monitor, Dr Morepen bp 09 bp monitor, Omron hem- 8712 bp monitor, Bpl b3 120/80 bp monitor, Omron hem-7124 bp monitor, Prozo plus fully automatic upper arm blood pressure monitor, bp monitor with premium quality, Bpl automatic 120/80 b11 white bp monitor, Choice med cbp1k3 bp monitor, hoice med digital bp monitor cbp1k2, Choice med economic cbp1e2 bp monitor
Many inaccurate monitors exist as over 3000 blood pressure
monitors are available but less than 15% of these have been
properly tested for accuracy. At clinics, filed research or at homes,
doctors researchers and public must use monitors that are
recommended, by one of these general registries:
STRIDE BP- stridebp.org/bp-monitors follow the detailed
instructions on page 2. The procedure to check validity includes
following steps:
Step 1: TYPE- www.stridebp.org/bp-monitors into your web
browser.
Step 2: SEARCH- By typing the precise model of the monitor
into the search box.
Alternatively, enter the monitor manufacturer’s name and scroll through the results until you find the model of the monitor listed. If the monitor is listed under the ‘Device Description’, then it has been validated. If “No results found” under ‘Device Description’ then the monitor is not recommended to be used
Medaval- medaval.ie/blood-pressure-monitors/ follow the instructions on page 3.
Step by step guide:
Tip: If the manufacturer name or monitor model cannot be
found, the monitor is unlikely to be validated.
Tip: Different star ratings are used by Medaval, but any
properly validated monitor will be
recommended, irrespective of the number of stars.
Step 1: SEARCH- Google* the make and model of the blood
pressure monitor, together with the word “Medaval”. *Or any
other search engine.
Step 2: LOOK- Look for and click on the link with the Medaval
evaluation of the monitor. Ignore any other advertising material
that may come up in the first few hits.
Step 3 CHECK- Scroll down to the accuracy assessment report.
Look for the Medaval assessment and Recommendation.
Service providers must not be tempted by brands or prices or reviews.
Source: Recommended by WHL/ASF/University of Tasmania
There are some COUNTRY-SPECIFIC REGISTRIES for Britain, Ireland, Canada, Germany, Japan, and United States of America. Click the relevant country and follow their instructions.
The statement has also addressed the role of out-of-office BP measurement in control of hypertension. Because of the ambiguity of evidence supporting home BP monitoring (HBPM) or ambulatory BP monitoring (ABPM) to guide management, it considers them “complementary to standardized clinic BP measurements” to be used when clinic BP measurements are unavailable [20,21].
The patient-related factors: should be eliminated. If the patient has not been prepared, then the measurement should be deferred for later. My case report clarifies the need for the patient to calm down and get familiar with the BP recorder for a while after reaching a clinic or at home for the BP to stabilize as trivial issues like driving, noise, stress, and anxiety reflect on the outcome of BP.
The procedure of measurement: The arm with the higher systolic BP readings should be used and more than 2 readings should be obtained in a gap of at least 30 seconds. The average of the readings should be recorded. Training and certification in proper office BP measurement followed by regular recertification will enhance accuracy. If Postural hypertension is suspected, BP must be measured three times, at 1 min intervals, after 5 min of seated rest and on standing, using an automated cuff sphygmomanometer, and be made a routine practice by the service provider.
Though the standardized measurement may particularly be difficult to implement in the resource-crunched parts of the world (rural India where Mercury based sphygmomanometers are still used) because of lack of availability of automated BP measuring devices or cuffs of different sizes or an optimal clinic environment or shortage of adequately trained staff. Most importantly, measuring BP is not subjected to regulatory standards, therefore improving practices will take time.
Conclusion
Accurate measurement of BP using the standardized BP measurement technique is essential to control the rising prevalence of hypertension. To mitigate the risk, high BP must be managed effectively and for this it must be measured accurately. Hypertension is a public health problem. Hence, the government regulatory agencies should devise strategies to educate the public, health care providers and institutions to meet the challenge. Training and certification should be mandated by the government. All healthcare workers must adopt the standardized measurement as part of the routine BP check in clinics and filed surveys, educate the patients on the need to do so at home. Financial incentives for standardized clinic BP equipment be provided by healthcare facilities /research organizations to enhance compliance. The role of healthcare institutions is to provide the proper validated equipment, staff and designate a proper clinic space. They must arrange for staff training and certification. Manufacturers should provide BP measuring devices and cuffs at an affordable cost. Professional societies must promote standardized clinic BP measurement among the fraternity and engage in educating the public.
References
- World Hypertension Day 2023.
- World family doctor day.
- Hypertension 2023.
- The New Blood Pressure Target in Primary Care, Neil Skolnik 2023.
- S F Koya (2022) Hypertension control rate in India: systematic review and meta-analysis of population-level non-interventional studies, 2001–2022. Lancet Reg Health Southeast Asia 9: 100113.
- S Basu (2023) Hypertension Control Cascade and Regional Performance in India: A Repeated Cross-Sectional Analysis (2015-2021). Cureus 15(2): e35449.
- Prevalence of Hypertension.
- Jinkook Lee, Jenny Wilkens, Erik Meijer, T V Sekher, David E Bloom, et.al. 2022 Hypertension awareness, treatment, and control and their association with healthcare access in the middle-aged and older Indian population: A nationwide cohort study. PLoS Med 19(1): e1003855.
- Soumitra Ghosh, Manish Kumar Prevalence and associated risk factors of hypertension among persons aged 15–49 in India: a cross-sectional study. BMJ Open 9(12): e029714.
- India Hypertension Control Initiative, a high impact and low-cost solution 2022.
- Thomas C Hinton, Zoe H Adams, Richard P Baker, Katrina A Hope, Julian F R, et al. Investigation and Treatment of High Blood Pressure in Young People- Too Much Medicine or Appropriate Risk Reduction?. Hypertension 75(1):16-22.
- Uday J (2021) Hypertension in Young Adults in India: Perspectives and Therapeutic Options amongst Clinician's in a Cross-Sectional Observational Study. J Assoc Physicians India 69(11): 11-12.
- Binayendu P, Anurag J, Mandar M S 2020 Demographic & angiographic profile of young patients aged 40 year & less undergoing coronary angiography in a tier II city of Eastern India. Journal of Family Medicine and Primary Care 9(10): 5183-5187.
- Sinead T J M, Natasha M, Christopher E (2021) Prevalence of postural hypotension in primary, community, and institutional care: a systematic review & meta-analysis. BMC Fam Pract 22 (1): 1.
- Arun G R, Siby G (2017) Delayed Orthostatic Hypotension: A Pilot Study from India, Ann Indian Acad Neurol. 20(3): 248-251.
- Akhil Sasidharan A community-based cross-sectional survey of orthostatic hypotension among elderly from south India. Indian Heart J 74(6): 478-483.
- Yusuf S, Steven H, Stephanie O, Tony D, Alvaro A, et al. (2004) Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364 (9438): 937-952.
- Four big ways-BP measurement-goes-wrong-and-how-tackle-them 2023.
- Cheung AK, Paul KW, Paul M, Aletta ES, Andrew EM, et al. (2023) international consensus on standardized clinic blood pressure measurement - a call to action. Am J Med. 136(5):438-445.
- Zhang J, Yukang M, Yansong L, Kun Z, Qiyang X, et al. (2023) Association between migraine or severe headache and hypertension among US adults: A cross-sectional study. Nutr Metab Cardiovasc Dis 33(2): 350-358.
- Blood pressure devices.






























