Wellens syndrome Type A. Case report
Sheila Candebat Correa*, Janet Quintero Chang, Kenia Roxana Candebat Correa
Doctor of Medicine, University of Medical Sciences of Santiago de Cuba, Faculty of Medicine No.1. Santiago de Cuba, Cuba
Submission: July 14, 2023; Published: July 21, 2023
*Corresponding author: Sheila Candebat Correa, Doctor of Medicine, University of Medical Sciences of Santiago de Cuba, Faculty of Medicine No.1. Santiago de Cuba, Cuba
How to cite this article:Sheila Candebat C, Janet Quintero C, Kenia Roxana Candebat C. Wellens syndrome Type A. Case report. JOJ Pub Health. 2023; 7(4): 555718. DOI: 10.19080/JOJPH.2023.07.555718
Abstract
Wellens syndrome is an electrocardiographic manifestation of critical stenosis of the anterior left descending coronary artery, the persistent reversal of the T-wave in the V2 and V3 shunts. It was decided to report the case of a 48-year-old female patient with the aim of describing her clinical and electrocardiographic characteristics. The patient goes to the Emergency Room of Saturnino Lora Provincial Hospital referring oppressive precordial pain of 15 days of evolution, where an electrocardiogram and coronary angiography are performed, being diagnosed with Wellens Syndrome type A. It was considered to report this case because it is not an immediate recognition syndrome and the findings predict with a high sensitivity and specificity the compromise of the proximal part of the anterior descending artery, requiring an early invasive strategy with the aim of avoiding complications such as acute myocardial infarction and death.
Keywords: Unstable angina; Anterior descending artery; Coronarography; Wellens Syndrome
Introduction
Cardiovascular diseases are currently the leading cause of death in industrialized countries and are expected to be so in developing countries as well. Among them, ischemic heart disease is the most prevalent manifestation, and is associated with high morbidity and mortality [1]. More than seven million people die each year as a consequence of ischemic heart disease, which corresponds to 12.8% of all deaths. This phenomenon will continue to rise in the coming years, so that by 2030 approximately 24.2 million deaths are forecast annually [1].
In Cuba, cardiovascular diseases are the first cause of death and represent 53.4%, with a rate of 284.4 deaths per 100,000 inhabitants [2]. Among the patients affected by acute coronary syndrome, a significant number present it without ST-segment elevation (NSTE-ACS) [3]. In the United States of America around 1.7 million people suffer from acute coronary syndrome, of which three quarters (almost 1.3 million patients) suffer from unstable angina or acute myocardial infarction without ST-segment elevation, and Cuba is no stranger to this statistic [4].
Wellens syndrome is an entity characterized electrocardiographically by the presence of inverted or biphasic T waves in the right precordial leads [5]. It corresponds to a subtype of unstable angina with a high risk of progressing to an acute anterior myocardial infarction [6]. These findings are associated with significant disease of the proximal segment of the left anterior descending artery (ADA) and may predict the subsequent development of an acute myocardial infarction as part of its evolution, with high sensitivity and specificity [3].
Wellens syndrome (WS), also called “left anterior descending artery T-wave syndrome”, was originally described by Wellens et al., in 1982 [7]. It was first reported as an inverted U wave, later presented as a pattern of electrocardiographic changes [8]. Of a total of 145 patients with unstable angina data, 18% did not show changes in the ST segment or changes in the QRS complex; however, inversion of the T waves of the precordial leads was found. These patients underwent an angiographic study to visualize the coronary arteries that showed occlusion of the left anterior descending artery with critical occlusion greater than 90%, with subsequent extensive anterior infarction if coronary intervention was not performed [9].
There are no publications in Cuba that include the incidence of Wellens Syndrome, nor the implications that its timely identification could have [3,10]. Wellens Syndrome is an electrocardiographic manifestation of a critical obstruction of the anterior descending artery that is usually not recognized or classified as nonspecific, so it is very important that primary care physicians, cardiologists, emergency physicians, and intensive care providers recognize. These electrocardiographic manifestations, therefore, typical or atypical, help us to assess risk and make quick decisions and actions to avoid complications that could compromise the patient’s life, for which reason it was considered to report this case with the aim of describing it clinically and electrocardiographically due to because it is not an immediately recognized syndrome, with few case reports described nationally.
Case Report
Female patient, mixed race, housewife, 48 years old with a history of Diabetes Mellitus and Hypertension for approximately 5 years, for which she has received regular treatment Metformin (500mg) 1 tablet at breakfast, lunch and dinner and amlodipine (10mg) ½ tablet every 12 hours. She refers that approximately 15 days ago due to emotional stress, she felt oppressive precordial pain which radiated to the left arm in resting position. The patient refers that the pain increased in frequency and intensity, was not relieved with sublingual nitroglycerin and was accompanied by autonomic symptoms and signs. With these clinical symptoms the patient was admitted to the Emergency Room for better study and treatment. She presents as a family pathological history of hypertension. She does not report adverse reactions to medications, surgeries, transfusions or trauma.
Positive signs on Physical Exam: Blood pressure 140/100 mmHg.
Results
Routine complementary tests were performed, which included a complete blood count, erythrocyte sedimentation rate, and blood chemistry, all of which were normal. No alterations were observed in an electrocardiogram performed as part of the chest pain protocol. Taking into account what has been stated up to now, she was admitted to the Cardiac Care Unit of the Saturnino Lora Provincial Hospital in Santiago de Cuba where biomarker enzymes of cardiac injury were indicated: Total CK: 88 U/I CK-MB: 7.5 U/I, values admitted within normal limits.
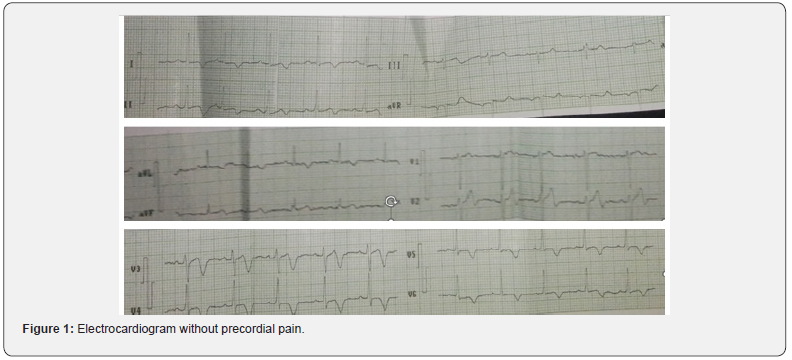
A new electrocardiogram was performed two hours later Figure 1 and the patient was free of pain, which, unlike the first, showed sinus rhythm, negative T waves in DI and AvL, V1, V4 -V6 and biphasic in V2-. V3 (Electrocardiographic tracing of precordial leads with criteria for Wellens syndrome Type A) Taking into account the aforementioned changes, it was decided to admit her to the Coronary Intensive Care Unit with the diagnosis of acute coronary syndrome without ST-segment elevation, where a complete management protocol was applied. Risk stratification of the patient considered at high risk was performed, due to the presence of dynamic electrical changes of the T wave in the electrocardiogram because Wellens syndrome, by itself, can represent a critical lesion in the anterior descending coronary artery at the proximal or medial level with a high probability of acute myocardial infarction with ST elevation in the short term and serious complications derived from it, it was coordinated with Cardiac Care Unit of Santiago de Cuba to perform Coronary Angiography and an early invasive strategy.
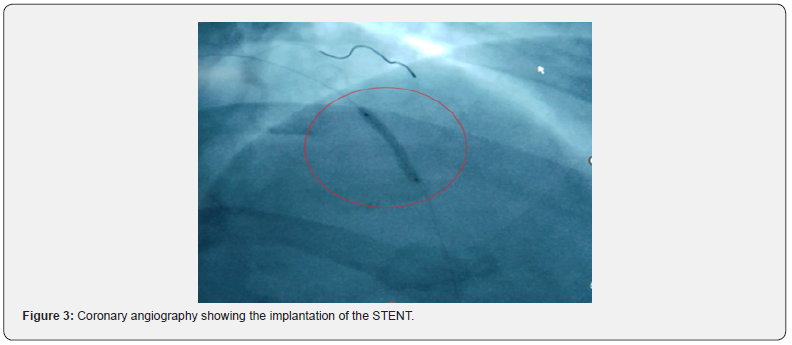
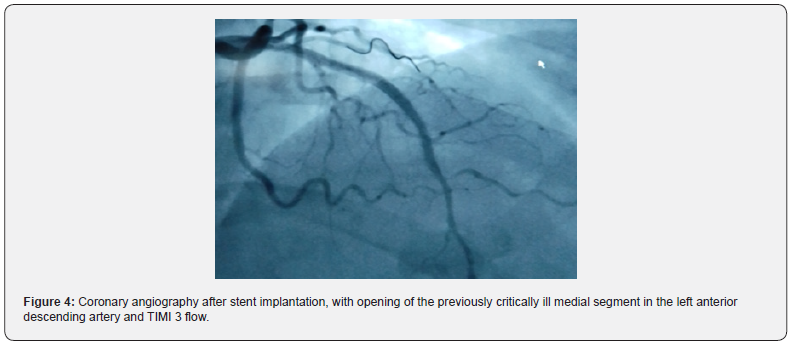
Subsequently, Coronary Angiography was performed, reporting left main coronary artery without lesions, anterior descending artery with a lesion in the distal middle segment of 99% with TIMI flow (Thrombolysis in myocardial infarction) [2], non-dominant circumflex artery without lesions, dominant right coronary artery without lesions Figure 2. It was decided to perform percutaneous transluminal coronary angioplasty (PTCA) in the middle distal left anterior descending artery and stent was implanted (Figures 3 & 4).

Conclusion
Severe vessel disease and successful percutaneous transluminal coronary angioplasty (PTCA) in the middle distal left anterior descending artery with TIMI 3 flow.
Definitive Diagnosis: The patient presents that symptoms suggest angina, electrocardiogram changes, and negative biomarkers. Therefore, it has been classified as a high-risk acute unstable angina.
Discussion
Wellens syndrome consists of the presence of an electrocardiographic pattern with changes in the T wave in the precordial leads, associated with previous symptoms of unstable angina [7]. The natural history is unfavorable, usually presenting a high incidence of recurrent symptoms and myocardial infarction, approximately 75% of patients will develop a large myocardial infarction in the next few days or weeks after the onset of symptoms [11].
Criteria for diagnosis or suspicion of this syndrome include:
i. History of old or recent chest pain.
i. Chest pain at the time of evaluation with normal electrocardiogram.
ii. Normal or slightly elevated cardiac enzymes.
iii. ST segment isoelectric or minimally elevated (<1 mm).
iv. Normal progression of the R wave in the precordial leads.
Biphasic or deeply inverted T waves in leads V2 and V3 and occasionally in V1, V4, V5 and V6 9,11.
In various studies [3,7,9 ,11] the absence of pathological Q waves in the precordial leads and loss of P waves are included as criteria. The authors consider that in cases of Wellens Syndrome with superimposed myocardial infarction, evidence of the pathological Q wave, in the same way this electrocardiographic pattern may or may not be accompanied by the P wave, depending on whether the patient presents sinus rhythm or arrhythmia.
Two electrocardiographic patterns can be evidenced:
1. WS type 1 or type A: corresponds to the minority of cases, presents greater specificity and consists of biphasic T waves in the precordial leads, mainly in V2 and V3. This carries a higher risk of mortality.
2. WS type 2 or type B: presents deep, symmetrical, inverted T waves (2mm or more) at the level of V2 and V3 11.
The patient in question went to the emergency department with symptoms suggestive of angina, changes in the electrocardiogram and negative biomarkers. Therefore, it has been classified as unstable angina and is an occasional presentation of acute coronary syndrome. This clinic corresponds to the majority of cases reported in the medical literature [7-9,12]. The electrocardiogram reported negative T waves in DI and AvL, V1, V4 -V6 and biphasic in V2-V3, classifying as Wellens pattern type A or type 1, which corresponds to the minority of cases (24%) [7] and is the one with the highest sensitivity and specificity [8]. The electrocardiographic changes presented in the clinical case described were evidenced in the absence of chest pain, and without elevation of cardiac enzymes, which is consistent with what has been reported by various authors [3,9,11].
In the literature consulted, several authors [5,8,12] state that the mechanisms associated with electrocardiographic changes are not entirely clear; but it has been proposed that they are related to a myocardium stunned by reperfusion, due to occlusion of the flow of the left anterior descending coronary artery that is spontaneously restored and it is believed that other elements apart from the coronary arteriosclerotic lesion can produce them, such as left ventricular edema, coronary spasm, right ventricular overload, microvascular disease, or nonspecific disorders of myocardial repolarization.
The authors of Torre Fonseca and Goire Guevara [3,5] agree that, in Wellens syndrome, the risk factors are shared with the traditional ones for coronary disease, such as: hypertension, diabetes mellitus, dyslipidemia, smoking, family history of coronary disease, obesity and sedentary lifestyle. In the clinical case under study, the patient presented a personal pathological history of Hypertension and Diabetes Mellitus. In the series presented by de la Torre Fonseca et al., 3 of a total of 14 patients with Wellens Syndrome, 10 were hypertensive, representing 71.4%, and 2 of them suffered from Diabetes Mellitus (14.3%).
During the fertile age of women, the protective action of estrogens increases high-density lipoproteins and favors the antiatherogenic effect, especially at the level of the coronary arteries, which explains why ischemic heart disease occurs less frequently and lasts an average of a decade after that in men [2]. This was revealed with different articles and papers such as the one presented by de la Torre Fonseca [3] and Bayón Fernádez [13]. Therefore, the case presented is peculiar as it is a 48-yearold female patient. Wellens syndrome suggests a severe occlusion in the proximal third of the left anterior descending artery (ADA), a branch of the left coronary artery [8]; however, in the coronary angiography of the clinical case in question, the lesion was evident in the distal middle segment.
Pharmacological therapy for Wellens Syndrome consists of antiplatelet drugs, antithrombotics, statins, and beta-blockers, although it should be noted that drug management is insufficient to prevent morbidity and mortality [5]. Treatment requires coronary angiography with urgent revascularization, since medical management improves symptoms, but revascularization will be required for definitive resolution [8] because if the patient is not taken to early revascularization, he or she may present left ventricular dysfunction, anterior myocardial infarction or sudden death [5].
To date, numerous cases have been published in which the presence of this diagnosis is related to unfavorable results in the angiographic study [3,8] in the case presented, the coronary angiography performed on the patient showed a lesion in the middle distal segment of the LAD of 99%. with TIMI 2 flow. Maintaining a high level of suspicion in all patients with clinical manifestations suggestive of ongoing myocardial ischemia with electrocardiographic and enzymatic patterns such as those described in this presentation will prevent them from progressing to serious or fatal complications, they will be offered better therapeutic possibilities and, At the same time, we will expand our knowledge based not only on literature, but on experience.
Conflict of Interest
The authors declare that there are no conflicts of interest.
Funding
The authors did not receive funding for the development of this article.
Authorship Contribution
SCC: Conceptualization, data curation, formal analysis, research, project management, writing-reviewing and editing.
JQC: Conceptualization, formal analysis, research, writing - original draft, writing-revision and editing.
KRCC: Conceptualization, formal analysis, research, writing - original draft, writing-revision and editing.
References
- Battilana Dhoedt JA, Cáceres de Italiano C, Gómez N, Lovera O, Centurión OA (2017) Perfil epidemiológico y retardo en la consulta de pacientes hospitalizados por síndrome coronario agudo. Mem Inst Investig Cienc Salud 15(2): 56-63.
- Ratia Vargas L, Santana Águila M, Etchegoyen López O, Piñeiro López R, Vila González JA. (2012) Caracterización del síndrome coronario agudo sin elevación del st en el centro dianóstico integral “José Gregorio Hernández” de Venezuela. Cor Salud 4(2).
- de la Torre Fonseca LM, Mederos Hernández J, Pérez Fernández A (2020) Caracterización del síndrome de Wellens y su relación como predictor de obstrucción grave de la arteria descendente anterior. Unidad de Cuidados Coronarios Intensivos Hospital Manuel Fajardo 2016-2017. CorSalu 11(4): 271-277.
- Vega Candelario R, Vega Jiménez J (2020) Alteraciones electrocardiográficas atípicas y estrategia invasiva en el síndrome coronario agudo sin elevación del segmento ST de alto riesgo. CorSalud 12(4): 481-484.
- Goire Guevara G, Arias Otamendy Y, Alberna Cardoso A (2022) Síndrome de Wellens, una forma grave de síndrome coronario agudo: informe de caso. Rev Inf Cient 98(3): 405-412.
- Ceballos Naranjo L, Torres Soto S, Cardona Vélez J (2018) Síndrome de Wellens: mucho más que una onda T. Arch Cardiol Méx 88(1): 64-67.
- Paredes A, Bittner A, Vergara I (2017) Dolor torácico y alteración electrocardiográ Rev Chil Cardiol 36: 154-157.
- Ramírez Chacón A (2016) síndrome de Wellens, un diagnóstico inusual y ominoso. Rev Méd Costa Rica Centroam 73(619): 329-332.
- Vergara Orduña FI, Macedo Calvillo L, Palacios Pérez E, Hernández Sánchez MM, Fonseca Tinoco NL (2018) Síndrome de Wellens, equivalente clínico de estenosis coronaria crí Med Int Méx 34(4): 658-661.
- Rodríguez LA, Rodríguez E, Gavilanes R, Gavilanes RC, Milord Y, et al. (2016) Presentación de un caso con síndrome de Wellens. Cor Salud 8(2): 132-135.
- Ramírez Chacón A (2016) Síndrome de Wellens, un diagnóstico potencialmente fatal. Rev Méd Costa Rica Centroam 70(620): 595–599.
- Carvajal CA, Ardila DJ (2015) Síndrome de Wellens: reconociendo el peligro. Rev Colomb Cardiol 22(5): 244-248.
- Bayón Fernández J, Alegría Ezquerra E, Bosch Genover X, Cabadés O Callaghan A, Iglesias Gárriz I, et al. (2022) Unidades de dolor torá Organización y protocolo para el diagnóstico de los síndromes coronarios agudos. Organización y protocolo para el diagnóstico de los síndromes coronarios agudos. Rev Esp Cardiol 55(2): 143-154.






























