Traumatic Bilateral Hip Dislocation
Fadi Albulayhishi*, Anas Abbas, Faisal Alrefaei and Mohammed Alghamdi
Department of orthopedics, Saudi German hospital, United Arab Emirates
Submission: July 30, 2022;Published: August 12, 2022
*Corresponding author: Fadi Albulayhishi, Department of orthopedics, Saudi German hospital, United Arab Emirates
How to cite this article: Fadi A, Anas Abbas, Faisal A, Mohammed A. Traumatic Bilateral Hip Dislocation. JOJ Orthoped Ortho Surg. 2022; 3(2): 555610.DOI: 10.19080/JOJOOS.2022.03.555610
Abstract
Bilateral traumatic hip dislocations are extremely rare. Most of these are related to acetabular or proximal femoral fractures. most have attributed the cause to high-velocity motor crashes. A case is reported of asymmetrical bilateral traumatic hip dislocation with an associated fracture of the acetabulum and femoral head occurring in a young adult with no previous history of hips abnormality.
Background: Traumatic hip dislocation is a serious injury with a high risk of death and morbidity. When the head of the femur is driven out of the acetabulum of the pelvis, it is called a traumatic hip dislocation. Depending on the type of damage, the femur head might be pushed anteriorly or posteriorly. According to the research, posterior dislocations are the most common type of dislocation, with anterior dislocations accounting for just 8-15 percent of all dislocations. Simultaneous asymmetrical bilateral hip dislocations, with one hip displaced anteriorly and the other posteriorly, are an uncommon occurrence, accounting for around 0.01 percent to 0.02 percent of all joint dislocations [1]. Other significant pelvic ring injuries or femoral fractures are commonly connected with this incident. Motor vehicle crashes were responsible for the bulk of the reported cases. Hip dislocations are medical emergencies that must be addressed as soon as possible to avoid long-term consequences. To provide the greatest outcome for the patient, prompt examination and treatment is required, as well as recognition of any problems.
Keywords: Bilateral; Traumatic hip; Femoral fractures; Dislocations; Lower limbs; Catastrophic
Introduction
Traumatic hip dislocation occurs when the ball of the hip joint is pushed out of its socket. The most common causes of this injury include car accidents, high-impact falls, work injuries, and sports injuries. Car accidents are the leading cause of hip dislocations. Traumatic hip dislocation is an uncommon but dangerous condition that can result in significant morbidity and mortality when triggered by high-energy trauma. In automobile accidents, hip joint injuries can range from mild injury with no functional repercussions to catastrophic fractures and dislocations. The position of the hip at the time of impact, as well as the vectors and strength of the forces, influence the dislocation’s orientation and whether it’s a fracture-dislocation or a pure dislocation [2]. Hip dislocations occur posterior in 90 percent of cases. Associated injuries are prevalent, and they can affect the ultimate result. Femoral head, neck, and shaft fractures, acetabular fractures, pelvic fractures, knee injuries, ankle and foot injuries, or a combination of these injuries are among them.
To rule out common associated injuries that might result in long-term morbidity, a complete trauma investigation is required. Early reduction within 6 hours is the cornerstone technique for reducing the complication of avascular necrosis. A hip dislocation or fracture dislocation is an orthopedic emergency. The time of presentation and, more importantly, the correction of the hip dislocation are key in treating this injury and preventing long-term effects such as avascular necrosis of the femoral head and late osteoarthritis of the hip [3]. Hip dislocations in the posterior orientation are the most common, notwithstanding their rarity. Because posterior hip dislocation requires such a large amount of force, it almost often occurs as a result of serious trauma. This is the most common event when the hip is flexed, and the knee is driven backward by an impact on the dashboard in an automobile accident [4]. A posterior hip dislocation occurs when axial stress is transmitted from the femur to the hip joint during hip adduction. A typical consequence of posterior dislocation is fractures of the acetabulum’s posterior lip and/or injury to the acetabular labrum.
Changing the hip’s position from extension to flexion causes a wall of the acetabulum or column fracture (in adduction). It’s unusual to have a posterior dislocation of the hip joint with an acetabular fracture. Early discovery, quick, and sustained decrease are the cornerstones of successful management. When diagnosis and treatment are delayed, complications and morbidity are unavoidable. The length of time between injury and therapy, the kind of fracture-dislocation, the consistency and stability of the reduction, and the degree of the damage all influence the eventual outcome [5]. Two novel classification algorithms for posterior dislocation have been developed. Epstein’s type 5 dislocation comprises four types of femoral head fractures, according to Pipkin:
a. A fracture below the fovea that does not damage the weight-bearing area of the skull is classified as type I.
b. type II: a weight-bearing surface of the skull fractured above the fovea.
c. Type III fractures have a femoral neck fracture in addition to a type I or II fracture.
d. type IV: acetabulum fracture with a type I or II fractures.
This instance shows a traumatic posterior hip dislocation with a femoral head fracture (Pipkin type2). A pipkin fracture with dislocation is, in most cases, a serious injury with a poor prognosis. Many of these cases are the result of car accidents that occur during a patient’s adolescence or early adulthood, when he or she is too young for a total hip arthroplasty. CT scans will detect fragile bone fragments or huge osteochondral fragments that must be surgically mended since an X-ray diagnosis is never enough to determine a treatment decision.
Pain, deformity, muscle spasms, and the inability to move the hip are all symptoms of hip dislocation. The patient will be unable to stand or support his or her weight on the hip. An abnormal hip and leg posture, as well as physical abnormalities, will be discovered during a medical examination. In posterior hip dislocations, the hip will be short and internally rotated, with the foot pointing inside toward the body’s midline [5].
Clinical Manifestation
During the clinical examination, the affected lower extremity is commonly shortened, adducted, and internally rotated. In most cases, AP pelvic x-rays will be sufficient for diagnosis, but simultaneous acetabular fractures will necessitate a CT scan. Because the femoral head and the acetabulum do not have typical joint congruency in both anterior and posterior dislocations, they may appear to be the same. In a posterior dislocation, the femoral head is typically displaced posteriorly, superiorly, and laterally to the acetabulum, as well as internally rotated, so the lesser trochanter is frequently covered on the AP view. The posteriorly displaced femoral head in a well-centered AP film will seem smaller than the contralateral hip due to geometric magnification, and vice versa.
For posterior hip dislocations, there are surgery and nonoperative therapy options. Both management approaches seek for a rapid reduction. Several studies have found that the amount of time the hip is dislocated increases the likelihood of complications, notably avascular necrosis in the native hip. Most orthopedic surgeons recommend a reduction duration of fewer than 6 hours, while some study shows that less than 12 hours may be critical; nonetheless, as the reduction time grows, the frequency of secondary issues increases significantly [6]. Anterior hip dislocations are typically caused by a significant force, such as trauma, or by an improperly positioned total hip arthroplasty. A stressful circumstance, such as a vehicle accident or a fall, causes the hip to be forced into abduction with external rotation of the thigh. Anterior hip dislocations are characterized by a shortened leg with the foot externally rotated or pointing away from the body’s midline.
Depending on the position of the femoral head, anterior hip dislocations are characterized as pubic or superior (type 1) or obturator or inferior (type 2) (type 2). Obturator dislocation of the hip in adults is unusual. The intrinsic stability of the joint, its deep placement in the pelvis, and the presence of strong ligaments and powerful muscles around the articulation all contribute to its rarity [7]. The importance of early detection and treatment in the treatment of serious injuries cannot be overstated. Obturator hip dislocations are a very uncommon complication that affects less than 5% of all traumatic hip dislocations. The presence of a strong anterior capsule and Bigelow’s Y-shaped ligament may contribute to a lower rate of anterior dislocation. The powerful abduction, external rotation, and flexion of the hip joint causes them to form. Road traffic incidents produced the majority of anterior obturator dislocations in the hip since the dislocating force was created by quick deceleration. Hip dislocation is a significant orthopedic emergency that requires immediate medical attention. Closed reduction under general anesthesia is the preferred therapy for traumatic obturator hip dislocations. Reduce must be done within 6 hours of the shock to avoid avascular necrosis. This is seen in 50% of cases if the hip is decreased longer than six hours after the event [8]. Because it is irreducible by closed reduction, hip dislocation of the obturator necessitates open reduction by an ileo-inguinal procedure. Open reduction with rectus femoris muscle relaxation was documented by Toms et al. Traction is recommended for three to six weeks after a hip dislocation to allow the capsular to heal, followed by progressive mobility and loading. Imaging of the femoral head’s vasculature is necessary to rule out indentation fractures and monitor the vasculature.
Case Presentation
A 31-year-old male who was the unrestrained driver in the front of a car going at high speeds and had no prior history of pelvic damage. At the time of the accident, the patient was sitting on the front console and was not in the correct seating position; there was no head injury or rollover. He was sent to the nearest hospital right away. The patient was awake, aware, and attentive upon arrival at the emergency room, and reported bilateral hip discomfort after first examination and stabilization. The right lower extremity was shortened and externally rotated, whereas the left lower extremity was in a relative internal rotation and seemed longer than the contralateral side, indicating asymmetric bilateral hip dislocations. Both lower limbs were judged to be neurovascularly sound, with normal feeling and palpable distal pulses.
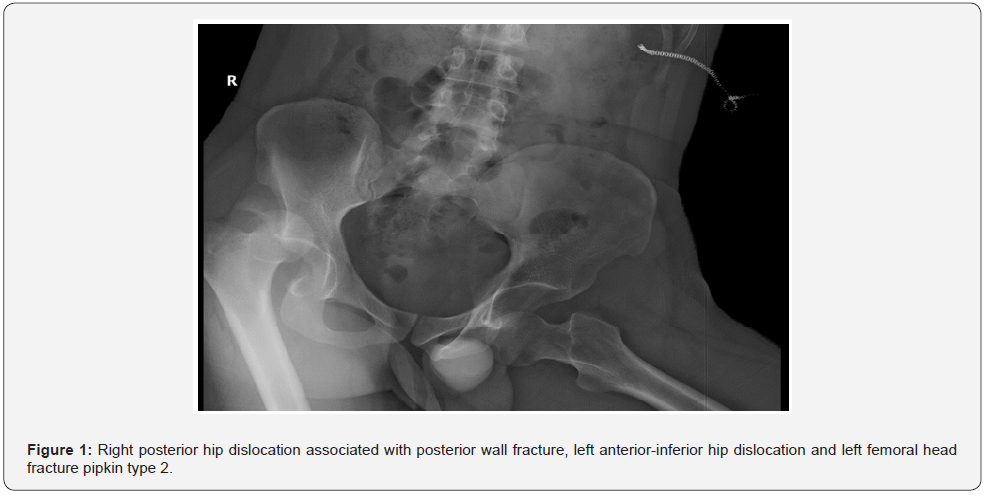
An AP pelvic radiograph revealed a right posterior hip dislocation with posterior wall fracture, a left anterior-inferior hip dislocation, and a pipkin type 2 left femoral head fracture (Figure 1). The patient was then consciously sedated at the emergency room. With sufficient anesthesia, a conventional in-line traction approach was used to try to reduce the right posterior hip dislocation by stabilizing the pelvis with hip and knee flexion, moderate traction, and hip adduction and internal rotation. Following the successful reduction of the right hip, the left anterior-inferior dislocation was treated using in-line axial and external rotation, as well as abduction.
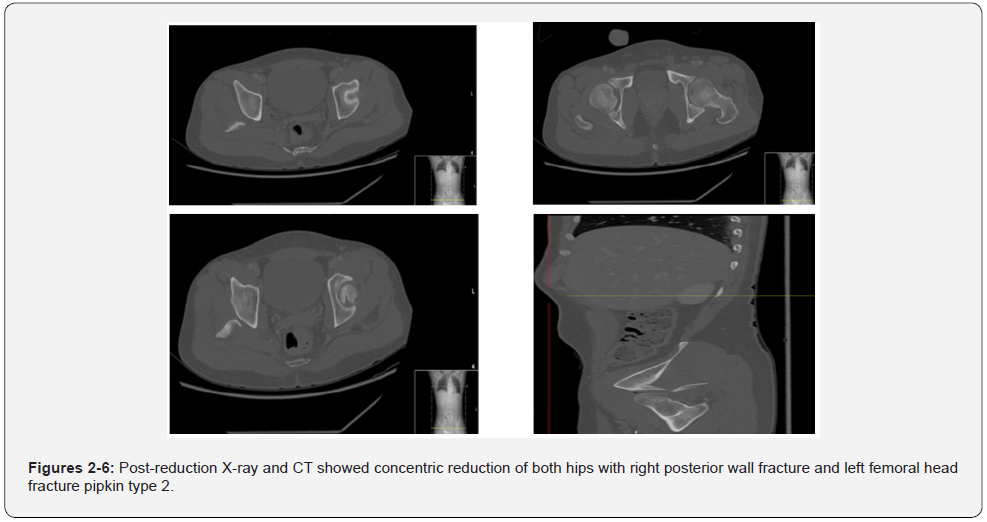
He appears to have retained his pre-reduction neurovascular state, with symmetric leg lengths. The hips were next checked, and the left hip was found to be stable, with concentric reduction of the head maintained, while the right hip was determined to be unstable. An after-reduction A CT scan and an X-ray revealed concentric reduction of both hips, as well as a right posterior wall fracture and a pipkin type 2 left femoral head fracture Figures (2-6). The patient was moved to the surgical room the same day after giving informed permission. The patient was put in the right lateral decubitus posture after receiving general anesthesia. One hour before the skin incision, he was given 2 gm of intravenous cefazolin for surgical prophylaxis. A posterior hip approach was used to begin treatment. We used K. wires to lessen the posterior wall fracture and keep it minimized. After that, we installed a 3.5mm reconstruction buttress plate. After that, the hip was checked and determined to be stable, with concentric decrease of the head maintained. We next turned our attention to the left hip, where we discovered that it was stable and that a little portion of the femur head had been conservatively treated. Following surgery, the patient was deemed non-weight bearing. From day one, we recommended a 45-degree semi-sitting position, static quadriceps strengthening activities, and passive ROM for the knee. At the six-week mark after surgery, follow-up x-rays revealed stable fixation. Partially weight bearing using a walker was common at the time.
Treatment
A dislocated hip is treated by attempting to reposition it by inserting the femoral head into the hip socket. Because of the discomfort and muscular spasms caused by the injury, sedation and muscle relaxation medicines are frequently used to allow the hip to be moved. The femoral head is replaced back into the acetabulum using traction on the leg. Closed reduction is what it’s called. The principles of reduction for posterior dislocations include flexion, internal rotation, and adduction of the hip. In-line traction with the hip and knee flexed to 90 degrees, followed by mild internal to external rotation, is used to decrease posterior dislocations. There are numerous distinct strategies for reduction: the Allis maneuver, the Bigelow maneuver, and the Captain Morgan approach.
Anterior dislocations need the same linear tension on the femur; however, due to the femoral head lying on the anterior surface of the pelvis in most instances, flexion of the hip is not typically achievable. Obturator dislocation 26 and public dislocation are the two forms of anterior dislocation known. For reduction, hip extension, in-line traction, and external rotation are typically required. In the case of a public dislocation, flexion of the hip is typically not feasible, necessitating hyperextension and in-line traction. Hip flexion, adduction, and external rotation are commonly used to minimize obturator dislocation. Axial traction is done once the head is freed from the obturator foramen. For patient comfort and to overcome the strong surrounding hip muscles, department-specific anesthesia is essential.
Even when a patient is under general anesthesia, the hip may not be able to be moved. A CT scan may be required to check for tiny bone fragments that have cracked (broken off) from the acetabulum, as well as portions of torn ligament or cartilage that obstruct the relocation. In this case, an orthopedic surgeon must perform an open reduction to remove any foreign items from the joint before reducing or replacing the hip into its socket. Arthroscopic surgery is sometimes used to achieve this.
Discussion
Traumatic hip dislocation is a critical emergency that requires immediate orthopedic evaluation and treatment. Hip dislocations are hazardous injuries that can cause long-term consequences such as avascular necrosis and posttraumatic osteoarthritis. They are particularly prevalent in young patients who have been exposed to high-energy trauma, and they are growing more common as a result of motor vehicle accidents, which account for 62 percent to 93 percent of all hip dislocations. Femoral neck fractures, on the other hand, are more likely in elderly people, unless they also have systemic illness. Patients with traumatic hip dislocation should get a thorough assessment by the trauma department due to the increased risk of additional injuries, particularly in the event of a motor vehicle collision. In 67 percent of patients with hip dislocation caused by a vehicle collision, non- orthopedic injuries were found, including 24 percent with closed-head injuries, 21 percent with craniofacial fractures, 21 percent with thoracic injuries, and 15 percent with abdominal injuries. Because of the hip’s inherent stability due to its osseous, labral, ligamentous, and muscular anatomy, dislocations frequently occur in conjunction with acetabulum or femoral head fractures. Dislocations without accompanying fractures may be less common than previously thought, thanks to the widespread use of computed tomography (CT) and its ability to detect microscopic fractures that may not have been seen on earlier radiographic scans. In 1821, a hip dislocation happened, which is considered to have influenced the current malpractice environment.
Hip dislocations are characterized in a variety of ways, some of which are very consistent. If a femoral head fracture is present, the Pipkin classification of femoral head fractures is commonly used, however neither radiologists nor orthopedic surgeons routinely diagnose hip dislocations using any one approach. Nonetheless, familiarity with the most widely used classification methods enhances understanding of the outcomes that have the most influence on patient care. The case recounted here involves a 31-year-old man who was the unrestrained front driver of a car traveling at high speeds and had no prior history of pelvic injuries. The patient was seated on the front console at the time of the accident and was not in proper seating posture; there was no head injury or rollover. In a rush, he was brought to the nearest hospital. He was sent to the hospital’s emergency room. The ATLS protocol was utilized at the time of arrival. Any victim with major injuries should have their airway, breathing, and circulation checked. During the secondary survey, the pelvic girdle and hip must be evaluated. The assessment should involve inspection, palpation, active/passive range of motion, and a neurovascular examination. The patient had a patent airway with good bilateral air intake on initial examination. His vital signs were stable at the time, and a physical examination confirmed that everything in his head and neck, chest, belly, and spine was in functioning order. The patient was awake, conscious, and observant, and he expressed soreness in both hips. The right lower extremity was shortened and externally rotated, whereas the left lower extremity was internalized and appeared longer than the contralateral side, demonstrating asymmetric bilateral hip dislocations. Asymmetric bilateral hip dislocations, in which one hip dislocated posteriorly while the other dislocated anteriorly, are a rare injury type that account for 0.01 percent to 0.02 percent of all joint dislocations. According to the earliest published case report in the international literature in 18451, an accidental overturning of a waggon packed with furniture resulted in a right posterior superior dislocation and a left anterior-inferior dislocation. Since that initial case report, there have been 104 examples of this uncommon injury, with discussions concentrating on the mechanism of damage, treatment, and injury outcomes; the most recent case series lists just 34 total incidents in the English language.
Hip dislocations are medical emergencies that must be addressed as soon as possible to avoid long-term consequences. Because native hip injuries are so severe, it’s vital to start enhanced trauma life support as soon as possible. Even if the damage is low-energy, a thorough examination should be carried out to rule out any fragility or concurrent injuries. The reason for dislocation (after total hip replacement versus native) and the kind of dislocation will be determined by a thorough history and physical examination (posterior vs anterior). In the case of a suspected hip dislocation, a physical examination is necessary. Closed reductions can be hampered by soft-tissue injuries and ipsilateral lower-limb injuries. Closed reduction may increase these concurrent ailments, therefore it’s critical to recognize them early. Because the knee is employed as a lever in decreasing the hip, an injury to the ipsilateral knee must also be checked out.
Because high-energy trauma might induce secondary injuries, a practitioner should do a neurovascular examination after obtaining the patient’s medical history and physical examination before attempting closed reduction. The most frequent nerve disorders associated with posterior hip dislocations are sciatic nerve damage (which occurs in 10% of cases) and peroneal branch and lumbosacral root injury. Examine the dorsiflexion of the ankle and toes to detect if the sciatic nerve has been injured.
A typical neurovascular complication associated with anterior dislocations is injury to the femoral nerve, artery, or vein. The sciatic nerve can be lacerated, stretched, or squeezed in an acute manner, and then encased in heterotopic ossification. The value of a neurologic evaluation right after an injury cannot be emphasized. Closed reduction should be performed as soon as feasible once a nerve injury is discovered to prevent nerve distortion caused by a dislocated femoral head or displaced acetabular fracture. The recommendations for further nerve damage therapy after a hip has been lowered have caused a lot of discussion. At least some nerve function recovery occurs in 60 percent to 70% of patients, with no obvious link to injury or therapy type. Patients who have had a sciatic nerve injury should begin therapy as soon as possible, with the goal of avoiding equinus foot deformity. Magnetic resonance neurography may be beneficial for the first evaluation of individuals with this damage in the future. Both of the suspect’s lower limbs, however, were found to be neurovascularly intact, with normal sensation and palpable distal pulses after investigation. Imaging is essential for detecting and treating hip dislocations, both at the time of presentation and after attempts at reduction. The radiologist must understand imaging signals that guide hip dislocation treatment in order to assist prompt diagnosis, characterization, and transmission of clinically meaningful outcomes. An AP radiograph of the pelvis was taken. Although the presence of a hip dislocation may be subtle, the majority of hip dislocations should be detectable on a complete AP pelvic radiograph evaluation. Lateral views can assist in determining the kind of dislocation. Right posterior hip dislocation with posterior wall fracture, left anterior-inferior hip dislocation, and pipkin type 2 left femoral head fracture were discovered on a pelvic radiograph.
A reduction technique to restore the bone to its correct position is the first line of treatment for a dislocated hip. Closed reduction is the term for this process. A variety of closed reduction methods make use of traction-countertraction and back-and-forth internal and external femur rotations. Any dislocated hip should be decreased as soon as feasible. Attempt to impart a reduction within six hours. Many others, on the other hand, have questioned the conventional wisdom of a six-hour concentric reduction. Letournel and Judet found no significant change in osteonecrosis when patients were given lower doses for up to 72 hours. These individuals are usually in a great deal of discomfort. With the possibility of subsequent injuries in mind, the initial analgesia should be delivered. A standard in-line traction strategy was used to try to minimize the right posterior hip dislocation, which comprised pelvic stabilization with hip and knee flexion, mild traction, and hip adduction and internal rotation. In this method, the patient is placed on a stretcher in a supine position. The practitioner should place himself next to the affected hip. Have an assistant stand at waist level on the unaffected side. PSA was given (procedural sedation and analgesia). The hip and knee are both flexed to 90 degrees. To administer axial(inline) traction, pull upward and maintain these flexions throughout the procedure. By standing on the stretcher, you may get more leverage. With the initial help, apply manual downward pressure on both iliac spines (countertraction to the hips), or fasten the patient to the stretcher with both. Maintain and gradually increase hip traction during the procedure. Begin and maintain a little amount of internal and external femur rotation (i.e., slowly wag the foot laterally and medially). If the proximal thigh does not diminish, apply lateral traction to the proximal thigh with arms or sheets. If reduction fails, abduct the femur to its maximum extent and have the third helper push down on the affected iliac spine with one hand while guiding the femoral head into the acetabulum with the other. When the reduction is complete, there may be an audible “clunk.”
“After effectively reducing the right posterior hip dislocation, attention was turned to the left anterior-inferior dislocation. To reduce anterior hip dislocations, in-line traction and external rotation are commonly utilized, with an assistant periodically pushing on the femoral head or pulling the femur laterally to promote reduction. Obturator dislocation is usually treated using hip flexion, adduction, and external rotation. Once the head is free of the obturator foramen, axial traction is used. Obturator dislocation is usually treated using hip flexion, adduction, and external rotation. With the patient in a supine position, the physician either enters the bed or stands alongside it. While an assistant stabilizes the pelvis, the surgeon grasps the ipsilateral leg at the knee and applies traction in the direction of the deformity. With this move, Toms, Dawson, and Dingley’s suggestions may be adopted. Among these are adduction, external rotation, and hip flexion. If the patient has a public dislocation, hip hyper-extension will be necessary. Patients should be positioned with a cushion or device between their knees, with their legs immobilized in slight abduction. The usage of cold packs and analgesics is required. X-rays should be obtained after the reduction, and the patient should be hospitalized for additional orthopedic care. While the patient is sedated, the degree of flexion, adduction, and rotation should all be documented. A hip abduction brace may be beneficial to a patient who continues to disregard safeguards. Following closure reduction, his leg lengths seemed symmetric, and he maintained his pre-reduction neurovascular condition. The hips were next examined; the left hip was found to be stable, with concentric head reduction maintained, whereas the right hip was found to be unstable.
A CT scan was performed to determine the fracture associated with these dislocations after the displaced bone was returned to its natural position. The most critical component in clinical success is fracture reduction accuracy. It is, however, difficult to maintain intra-articular fracture fragment reduction until firm union occurs. Unless the intercalary osteochondral fragments are given extra support, maintaining anatomical reduction after substantial comminution is more difficult. Furthermore, once the overlying posterior wall component is reduced, migration of potentially mobile intervening osteochondral fragments may occur. A two-level reconstruction method, on the other hand, appears to provide the necessary stable fixation and has been connected to the best posttraumatic osteoarthritis and clinical prognostic outcomes. Before the bone graft material is placed in the two-level surgery, these intra articular fragments are temporarily held in place by 1.6-mm Kirschner wires. For final attachment, Kirschner wires are replaced by 2.0-mm mini-screws or, preferably, 1.5-mm bioabsorbable pegs, which are generally 40 mm in length. In large osteochondral fragments, several wires can be inserted to allow sequential exchange to the final fixation, lowering the risk of reduction loss during the exchange procedure. The overhanging posterior wall fragment can be reduced and fixed without displacing the underlying osteochondral components, completing the two-level fixation construct. This is how the best results may be obtained.
When treating fractures with poor bone quality, such as osteomalacic or osteoporotic fractures, devices that provide relative stability are favored. These include bridge plates, buttress plates, and intramedullary nails, to name a few. It’s also vital to maintain the whole bone to avoid future fractures]. Under direct monitoring, a ball-spike pusher and K-wires for provisional stabilization should be employed to reduce the fracture. Prior to final reduction, any marginal fracture impaction should be addressed. Lag screws can be placed perpendicular to the fracture plane if necessary to maintain reduction. A buttress plate is used to secure the structure. A 3.5 mm or two pelvic reconstructive plate may be necessary. The plates usually have six to eight holes and must be undercounted before being used. When the screws are installed, the plate adapts to the bone and provides the necessary buttress effect. The plate must be properly balanced along the posterior wall fragment in order for the plate’s force to be contained. The screws should be placed such that they are facing away from the joint. Two screws in the proximal area of the plate and two screws in the distal section of the plate are usually sufficient for fixation. After the posterior wall fragment has been reduced, the limb should be tested for range of motion to check whether there are any restrictions. Fluoroscopic imaging should also be used to check the screws’ extra-articular placement.
Conclusion
Dislocation of the hip is a well-described occurrence that results in femoral head dislocation from the acetabular socket following high-energy trauma or postoperatively after total hip replacement. Car accidents account for the vast majority of hip dislocations. Hip dislocations are usually characterized by the direction in which the femoral head dislocated, either anterior or posterior. A posterior dislocation happens 90% of the time when there is axial force on the femur, usually with the hip flexed and adducted axial load via the flexed knee. The location of the hip influences the severity of the acetabular damage. Anterior dislocation is caused by femoral head impaction or chondral damage, and it usually happens when the hip is in abduction and external rotation.
Hip radiographs can be used to detect the direction of dislocation, and CT scan studies can be used to check for any related injuries. To provide the best outcome for the patient, prompt examination and treatment, including recognition of any problems, are required. Treatment consists of an immediate reduction to reduce the danger of avascular necrosis, followed by a CT scan to check for any accompanying injuries that may necessitate surgery (loose bodies, femoral head fractures, acetabular fractures).
References
- (2022) EBSCOhost Traumatic Hip Dislocation.
- Onyemaechi NO, Eyichukwu GO (2011) Traumatic hip dislocation at a regional trauma center in Nigeria. Niger J Med. 20(1): 124-130.
- Shaw KA, Hire JM, Cearley DM (2020) Salvage Treatment Options for Painful Hip Dislocations in Nonambulatory Cerebral Palsy Patients. J Am Acad Orthop Surg 28(9): 363-375.
- Hougaard K, Thomsen PB (1989) Traumatic hip dislocation in children. Follow up of 13 cases. Orthopedics 12(3): 375-378.
- (2022) Posterior Hip Dislocations: A Cadaveric Angiographic Study: Journal of Orthopaedic Trauma.
- Steppacher SD, Albers CE, Siebenrock KA, Tannast M, Ganz R (2013) Femoroacetabular Impingement Predisposes to Traumatic Posterior Hip Dislocation. Clin Orthop Relat Res 471(6): 1937-1943.
- Laorr A, Greenspan A, Anderson MW, David Moehring H, McKinley T (1995) Traumatic hip dislocation: early MRI findings. Skelet Radiol 24(4): 239-245.
- Rodríguez-Pérez M, Dávila-Parrilla A, Rivera L, Olivella G, Muñiz A, et al. (2020) Socioeconomic Factors Influencing Self-reported Outcomes After Posterior Wall Fractures of the Acetabulum: Lessons Learned From a Hispanic Population. J Am Acad Orthop Surg Glob Res Rev 4(10): e20.00162.






























