The management of Adjuvan Radiotherapy for the Heterotopic Ossification Prophylaxis
Bora Uysal*, Hakan Gamsiz and Murat Beyzadeoglu
Department of Radiation Oncology, University of Health Sciences, Turkey
Submission: February 21, 2022;Published: March 11, 2022
*Corresponding author: Bora Uysal, Department of Radiation Oncology, University of Health Sciences, Gulhane Medical Faculty, Turkey
How to cite this article: Bora U, Hakan G, Murat B. The management of Adjuvan Radiotherapy for the Heterotopic Ossification Prophylaxis. JOJ Orthoped Ortho Surg. 2022; 3(2): 555608.DOI: 10.19080/JOJOOS.2022.03.555608
Abstract
Background: We analysed 38 heterotopic ossification patients retrospectively and gave results about recurrence, efficiency and adverse events. Purpose of the study: Our goal is to identify postoperative radiotherapy is effective or not in heterotopic ossification prophylaxis.
Material methods: 38 patients receiving image‑guided RT (IGRT) for heterotopic ossification at our department between January 2010 and November 2020 were assessed retrospectively. Inclusion criteria’s were eastern cooperative oncology group performance status of 0–1, no previous RT history and connective tissue disease.
Results: Of the total 38 patients, 14 patients (36.8%) were female, and 24 patients (63.2%) were male. The median age was 52 years (39-65). The median follow‑up duration was 26 months (20-36 months). 90 percent of heterotopic ossification was located at hip of patients whereas 10% was at elbow.
Conclusion: Preoperative or postoperative radiotherapy for preventing heterotopic ossification should be offered to the patients. We concluded that postoperative single dose 7 Gy is enough for patients, and it is safe and efficient method.
Keywords: Heterotopic ossification; Radiotherapy; Surgery
Introduction
Frequent complication of acetabular fracture, hip trauma or arthroplasty is heterotopic ossification (HO). If soft tissue around hip starts to be ossified, HO occurs then. Transformation from mesenchymal cells to osteoblasts and mature bone is the appearing of HO after trauma. Femoral head and hip are the common affected area of HO. The etiological or risk factors are still unknown whereas HO is mostly seen in men who has a Paget, ankylosan spondilitis or osteoarthritis. No pain but stiffness of hip is typical symptom of HO. Radiographic diagnosis is a popular situation incidentally or after trauma. HO prophylaxis should be offered to the patients at risk after surgery. Indomethacin which is nonsteroidal anti-inflammatory (NSAID) is effective for reducing risk of HO. Mesenchymal cells are suppressed after prostaglandin synthase inhibition via NSAIDs. Cyclo-oxygenase-2 inhibitors do not have an approval for prophylaxis according to the studies. Bisphosphonates are the other alternative that delaying mineralization of osteoid. Contemporary radiotherapy is used by experts for malignant and non-malignant diseases such as HO. Prevention of HO after arthroplastic surgery is applied via radiotherapy. First use of radiotherapy in HO is in 1970’s. Preoperative or postoperative single dose of 7-8 Gy is beneficial for the risky region. The most important issue is the delivering time within 24 hours preoperatively and 72 hours postoperatively. Comparative evaluation of NSAIDs and radiotherapy offered similar results about HO prophylaxis. One metanalysis showed better results with radiotherapy compared to NSAIDs but another is concluded with no significant difference between two alternatives. Cost-effectiveness of RT is another issue discussed with recent studies.
Material and Methods
38 patients receiving image‑guided RT (IGRT) for heterotopic ossification at our department between January 2010 and November 2020 were assessed retrospectively. Inclusion criteria’s were eastern cooperative oncology group performance status of 0–1, no previous RT history and connective tissue disease. Informed consent of all patients was obtained before the treatment, and the study was performed in compliance with the Declaration of Helsinki principles. Planning CT images were acquired to delineate the critical structures and gross tumor volume, clinical target volume (CTV), and planning target volume (PTV) for all patients. GTV and CTV were the same. CTV was established as a joint of hip or elbow including surgical materials. PTV was created by adding 0.5 cm to the CTV (figure 1). IGRT plans were generated for RT with image guidance. Supine positioning was used for treatment planning. Planning CT images with 5‑mm slice thickness were acquired. The planning CT images were sent to the contouring station through network. Advantage Sim MD simulation and localization software (Advantage Sim MD, GE, UK) were used for the delineation of the organs at risk and treatment volumes. All RT plans were generated using Precise PLAN (Elekta, UK) treatment planning system. CTV coverage was maintained between 95% and 107% for all RT plans. Dose‑volume histograms were thoroughly assessed by the treating radiation oncologist and radiation physicist before treatment. All patients received single 7 Gy fraction after surgery within 72 hours. RT was delivered by synergy (Elekta, UK) linear accelerator with the capability of daily online set‑up verification under image guidance with kilovoltage cone‑beam CT (kv‑CBCT) and (X‑ray Volumetric Imaging [XVI], Elekta, UK). 6-18 mv photon energy was used. All patients were treated after online verification of setup by the use of kV‑CBCT and XVI. Statistical analysis Statistical Package for the Social Sciences, version 16.0 (SPSS, Inc., Chicago, IL) software was used for the data analysis with the level of significance set at p < 0.05. Age, gender, heterotopic ossificans location, follow‑up time, adverse events and recurrence were comparatively assessed.
Results
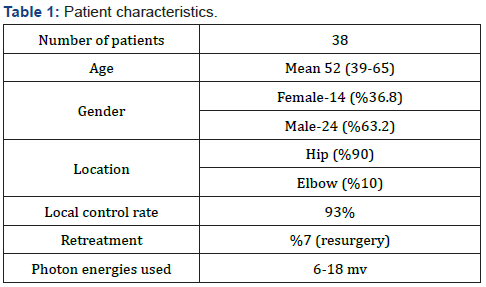
Patient characteristics are shown in table 1. Of the total 38 patients, 14 patients (36.8%) were female, and 24 patients (63.2%) were male. The median age was 52 years (39-65). The median follow‑up duration was 26 months (20-36 months). 90 percent of heterotopic ossificans was located at hip of patients whereas 10% was at elbow. Local control rate after combined treatment was 93%. The patients who relapsed were retreated with surgery and no recurrence afterwards. Adverse events were analysed 3 monthly for all patients after combination treatment. Grade 1 erythema was shown in 25 percent of all group whereas no grade 2 or more dermatological adverse effect were seen in this population. Joint stiffness was seen in 10 percent of group, and they were treated with physical therapy and oral medications.
Discussion
Perioperative radiotherapy is effective after hip surgery or trauma to prevent heterotopic ossification. Randomized trials firstly compared low or medium dose radiotherapy to find effective BED (biological effective dose) then focused on which scheme was better including preoperative or postoperative radiotherapy. Total 17.5 Gy in 3 fractions was better than 10 Gy in 2 fractions and no difference was shown between preoperative or postoperative radiotherapy groups [1]. Radiation induced malignancy is another issue and also a rare complication with lower doses of radiotherapy. One case that was delivered 7 Gy for heterotopic ossificans prophylaxis 11 years ago was presented with osteosarcoma near to the radiotherapy field afterwards. The risk assesment should be made for patients before radiotherapy planning [2, 3]. Lower doses such as 500 cgy may be effective to prevent heterotopic ossification compared to 1000 cgy. One pilot study by Padgett et al showed that no significant differences were seen between 5 Gy and 10 Gy groups after total hip arthroplasty Success rates were 93% and 97% in groups respectively [4]. Between 6-10 Gy total dose was used for the 9 cases to prevent heterotopic ossification specifically in the elbow region. None had radiological recurrence nearly after 1 year follow-up. Functional scores and outcomes indicated high therapeutic efficacy of prophylactic irradiation [5]. Hip location is moderately more frequent for improving heterotopic ossification after trauma or surgery compared to elbow or any site. In a 52 patient case series, researchers applied postoperative radiotherapy and nonsteroidal anti-inflammatory drugs together. It was safe and efficacious in preventing development of heterotopic ossificans in the elbow region [6]. Kantarowitz et al showed that preoperative radiotherapy should be offered to the patients because of more patient discomfort and radiation staff resource utilization with postoperative radiotherapy. They applied 7-8 Gy in one fraction along with 4-20 mv photons to the anteroposterior and posteroanterior weighed location [7]. Failure rate was only 8% in one study by Robinson et al. Postoperative single 6 or 7 Gy was applied to the patients after surgery. They found favorable functional and radiographic results with this analysis. All patients had flexion or extension limitations at baseline, but these were functionally improved after postoperative radiotherapy [8]. The prolongation of the timing radiotherapy and surgery is a challenging issue to be solved. Heterotopic ossification development was increased from 10 % to 90 % if patients treated not in three days after surgery but after 21 days [9, 10]. Reirradiation is another topic for preventing heterotopic ossificans. If heterotopic ossificans occur after surgery, second surgery is discussed by experts and postoperative or preoperative radiotherapy is offered to this group as a safe and efficient modality according to the literature [11].
Conclusion
Preoperative or postoperative radiotherapy for preventing heterotopic ossification should be offered to the patients. We concluded that postoperative single dose 7 Gy is enough for patients, and it is safe and efficient method.
References
- Seegenschmiedt M, Keilholz L, Martus P (1997) Prevention of heterotopic ossification about the hip: final results of two randomized trials in 410 patients using either preoperative or postoperative radiation therapy. Int J Radiat Oncol Biol Phys 39(1): 161-171.
- Farris M, Chowdhry V, Lemke S (2012) Osteosarcoma following single fraction radiation prophylaxis for heterotopic ossification. Radiat Oncol 7: 140.
- Mourad W, Packianathan S, Shourbaji R (2012) Radiation induced sarcoma following radiation prophylaxis of heterotopic ossification. Pract Radiat Oncol 2(2):151-154.
- Padgett D, Holley K, Cummings M (2003) The efficacy of 500 cgy radiation in the prevention of heterotopic ossification after total hip arthroplasty: a prospective, randomized, pilot study. J Arthroplasty 18(6): 677-686.
- Heyd R, Strassmann G, Schopohl B (2001) Radiation therapy for the prevention of heterotopic ossification at the elbow. J Bone Joint Surg Br 83(3): 332-334.
- Strauss J, Wysocki R, Shah A (2011) Radiation therapy for heterotopic ossification prophylaxis after high-risk elbow surgery. Am J Orthop 40(8): 400-405.
- Kantarowitz D, Muff N (2010) Preoperative vs postoperative radiation prophylaxis of heterotopic ossification: a rural community hospital’s experience. Int J Radiat Oncol Biol Phys 77(5): 1493-1499.
- Robinson C, Polster J, Reddy C (2009) Postoperative single fraction radiotherapy for prevention heterotopic ossification of the elbow. Int J Radiat Oncol Biol Phys 06:72.
- Mourad W, Packianathan S, Shourbaji R (2012) A prolonged time interval between trauma and prophylactic radiation therapy significantly increases the risk of heterotopic ossification. Int J Radiat Oncol Biol Phys 82(3): 339-344.
- Childs H, Cole T, Falkenberg E (2000) A prospective evaluation of the timing of postoperative radiotherapy for preventing heterotopic ossification following traumatic acetabular fractures. Int J Radiat Oncol Biol Phys 47(5): 1347-1352.
- Lo T, Healy W (2001) Reirradiation for prophylaxis of heterotopic ossification after hip surgery. Br J Radiol 74(882): 503-506.






























