Incidence of Clinical Venous Thromboembolism in Spinal Trauma with and without Spinal Cord Injury
Nabil Alageli A1* and Aheed Osman2
1Department of Orthopaedics, Tripoli University Hospital, University Road, Tripoli, Libya
2Midlands Centre for Spinal Injuries, The Robert Jones & Agnes Hunt Orthopaedic Hospital, Oswestry, UK
Submission: July 12, 2021;Published: July 29, 2021
*Corresponding author: Nabil Alageli A, Department of Orthopaedics, Tripoli University Hospital, University Road, Tripoli, Libya
How to cite this article: Nabil Alageli A, Aheed O. Incidence of Clinical Venous Thromboembolism in Spinal Trauma with and without Spinal Cord Injury. JOJ Orthoped Ortho Surg. 2021; 3(1): 555604.DOI: 10.19080/JOJOOS.2021.03.555604
Abstract
Introduction: the risk of venous thromboembolism (VTE) after Spinal injuries was largely realised but the true incidence of which is still variable and unclear.
Patients & method: We retrospectively reviewed the charts of 374 consecutive patients who sustained traumatic spinal injury and admitted acutely to a comprehensive care spinal injuries centre. 159 patients had spinal trauma with spinal cord injury (SCI) and 215 were neurologically intact. The majority of these patients were treated non-surgically and received the same thromboprophylactic regimen started within a median of 2 days post injury. The incidence of clinical VTE (deep Vein thrombosis DVT & Pulmonary Embolism PE) was determined and some risk factors discussed.
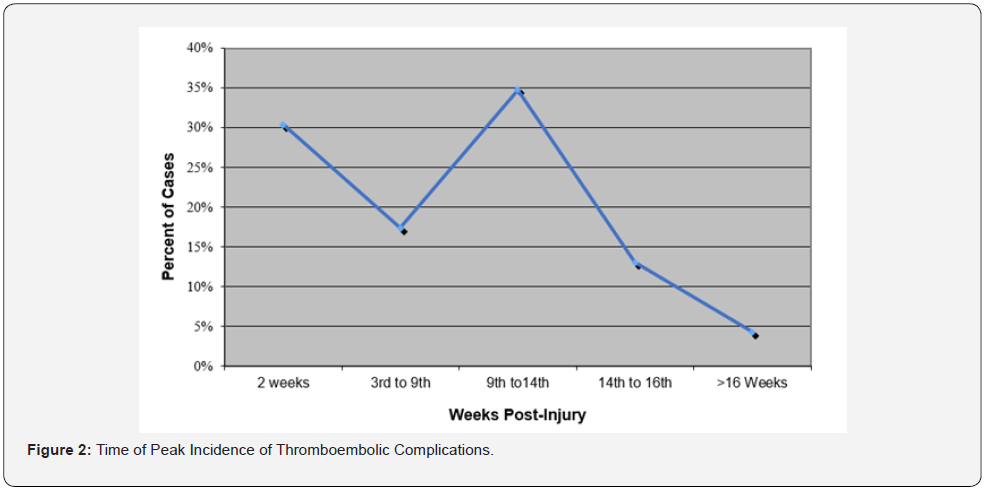
Results: Among the neurologically intact group one patient developed clinical PE (0.5%). Out of 159 patients with SCI, 23 developed clinically evident VTE (14.5%), 15 had DVT (11.9%), 4 PE (5%) and 4 had both DVT & PE). There was no fatality. Complete SCI lesions were associated with higher incidence of VTE compared to incomplete lesions, 17.6 % & 11% respectively (p<0.001). We found two peaks of thromboembolic episodes the first during the first 2 weeks after injury (30% of cases), the second after the 8th week post injury (38% of cases).
Conclusion: Spinal cord injury is associated with high risk of venous thromboembolism and the risk increases with the severity of cord insult. While spinal column injury is shown to be associated with a relatively low risk in this series. The risk is reduced with strict adherence to thromboprophylactic regimen which we suggest continuing for at least 12 weeks for SCI patients.
Keywords: Spinal injury; Spinal cord injury; Pulmonary embolism; Deep vein thrombosis; Venous thromboembolism; Thromboprophylaxis
Introduction
For several decades, the potentially fatal outcome from VTE in spinal cord injuries, was realised, Tribe in 1963 [1,2] showed PE to be the cause of death of 37% of those dying within 3 months of SCI (without prophylaxis). Green et al, reported 4% mortality due to PE with thromboprophylaxis [3,4]. De Vivo [5] reported PE as the cause of death in 9.7% of 496 SCI patients in the first year after injury Waters et al [7] reported an incidence of 14% clinically evident DVT in 909 patients with acute spinal cord injury (SCI), they noted no difference between the surgically and non-surgically treated groups (13% Vs 15% respectively). The incidence of PE was equal for both groups at 5%. In our comprehensive care centre for spinal injuries, a thromboprophylactic regimen of a combination of pharmacological (LMWH/Warfarin) and mechanical means is implemented on all patients with spinal injuries with or without neurological deficit. We evaluate the results of this regimen and discuss variations in incidence by age groups, gender, level and presence or absence of neurological deficit and its severity.
Patients and Methods
Subjects
We reviewed the clinical notes and the centre database system, of all newly admitted patients over a 3-year period. The total number of new patients admitted to the centre during the period of study was 467 patients
We included patients who sustained trauma to the spine, admitted within 2 weeks from injury and commenced on anticoagulation prophylaxis within 72 hours (n=374). Ninetythree patients were excluded as they did not fulfil the above criteria (34 were non-traumatic and 59 were traumatic but admitted late or did not complete treatment). There were 215 patients of spinal column injury and no neurological deficit (ASIA E) and 159 patients with SCI resulting in either complete (ASIA A) or Incomplete (ASIA B, C or D) paralysis.
Prophylactic Measures
All patients were commenced on Low Molecular Weight Heparin (Tinzaparin) within 72 hours of injury. Patients were subsequently started on Warfarin (AVK) once they were able to take oral medication. The INR (International Normalization Ratio) was regularly monitored to maintain adequate prophylactic levels (target INR level of 2.0, range 2 to 3). Warfarin was discontinued after an average period of 7. 6 weeks from injury and patients were monitored for evidence of VTE until discharge. Passive exercises by physiotherapy and nursing staff were carried out daily; Elasticated Compression (TED) Stockings were applied from the day of admission unless there was a contra-indication. Patients were monitored for clinical evidence of VTE daily. If suspected, the diagnosis was confirmed or refuted by Ultrasound / ipsilateral venography for DVT and Ventilation–Perfusion (V/Q) Lung Scan for PE. Postmortem examination was carried out for all causes of death. The data was analysed using Excel spreadsheet and SPSS statistical package, Chi Square test was used for measuring independence of variables, ANOVA and t-test were used to compare variances and means, with 95% confidence interval (CI).
Results
The Neurologically Intact Group
215 patients fulfilled the criteria for inclusion, these were 141 (67%) males and 74 (33%) females, the mean age was 38.6 (STD±19.9) years with an average period of in-hospital stay of 34 (STD±24) days. One patient, aged 70 years, developed symptoms and signs of pulmonary embolism, confirmed by a V/Q lungs scan, 11 days post injury. He had fracture L1 vertebra treated by surgical stabilization. None of the patients in this group developed clinically detectable DVT. (Table 1).
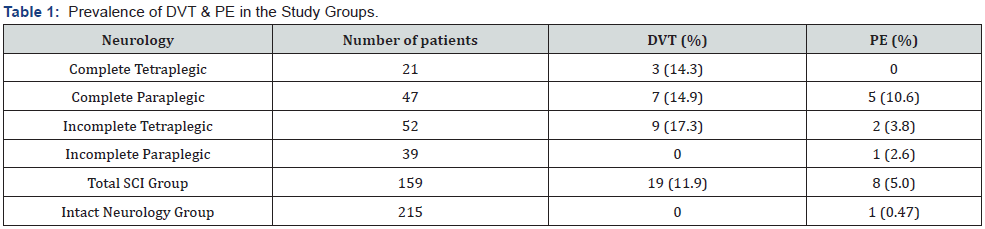
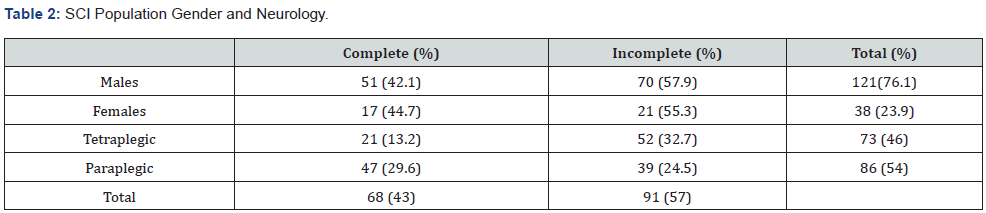
The Spinal Cord Injury (SCI) Group
The median time to admission to the centre after injury was 2 days. There were 73 cervical, 60 thoracic and 26 lumbar vertebral injuries with an injury to the spinal cord or cauda equina. The mean age was 40.7 years (Range: 14-88 years), there were 121 (76 %) males and 38 (24%) females. Sixty-eight patients (43%) had complete injuries and 91 (57%) had incomplete neurological loss (Table 2). Ninteen patients developed clinically manifest DVT, confirmed by venography, a prevalence of 11.9%. Four of these patients developed signs of PE confirmed with Ventilation/ Perfusion lung scan. Four other patients had confirmed clinical PE without clinical signs of DVT. The total prevalence of PE was 5% (Table 1). No fatal PE occurred in the treated patients. There were 8 deaths during the study period. All underwent a post-mortem examination. PE was the cause of death of one patient who was 81 years old with central cord syndrome who died on the second day post injury, the same day he was transferred to the spinal centre.
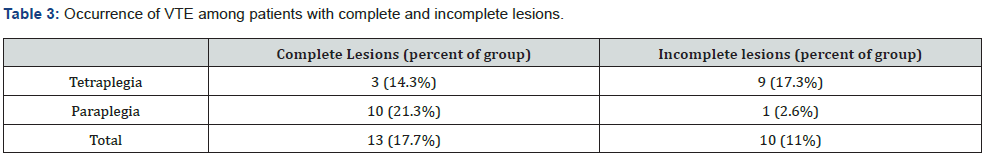
He had not received thromboprophylactic treatment and was not included in this sample. When analysed by age, the prevalence of VTE was found to be higher in the age group between 40 to 60 years. There was however no statistically significant correlation between age and incidence of VTE (Figure 1). When analysed by gender, it was noted that DVT occurred more commonly in males (13.2%) than females (7.9%) while PE occurred in equal frequency in both sexes. Overall, there was no statistically significant difference in incidence of VTE between males and females. Patients with complete lesions had a higher occurrence of VTE (17.7%) than those with incomplete lesions (11%). The difference was statistically significant (p<0.001); the highest occurrence of PE was in the complete paraplegia group (21.3%) (Table 3). Two peaks of thromboembolic episodes were noticed, the first during the first 2 weeks after injury (30% of cases), the second after the 8th week post injury (38% of cases) (Figure 2), after discontinuing thromboprophylaxis.

Discussion
Regimens instituted for thrombo-prophylaxis, still vary widely from simple TED stockings to the insertion of vena cava filters. Data from the model system in North America, reports fatal PE to be the third most common cause of death in the first year after SCI [5]. Green et al also reported fatal PE in 2 of 41 (5%) and 2 of 48 (4%) SCI patients [3,4]. The consortium for spinal cord medicine guidelines stated that combination treatment prophylactically is more efficient than a single method [7]. Low Molecular Weight Heparins (LMWHs) are the most commonly prescribed chemical thromboprophylactic agents, alone or in combination with mechanical means. Oral anti vitamin K (AVK) is still being used in some spinal injuries centers in the UK especially for the long-term prophylaxis. Thumbicat et al . [8] suggested that it remains a safer option than Enoxaparin in the SCI population. In our experience a combination regimen of LMWH/Warfarin, with mechanical means was effective in preventing fatal PE and in reducing VTE morbidity. There were two peaks for the incidence of VTE. The first within two weeks from injury. The incidence rises again after the 8th week post injury following discontinuation of thrombo-prophylaxis in this series. This is similar to the finding by Thumbicat et al. [ 8]. Green et al . [3] also reported one fatal PE out of 33 patients, 2 weeks after discontinuation of thromboprophylaxis. We therefore suggest that thromboprophylaxis continues for at least 12 weeks post injury or until discharge in high-risk patients (vide infra). This recommendation was also made in 2004 by the seventh ACCP conference on antithrombotic and thrombolytic therapy [ 9]. We have shown that the prevalence of VTE was highest among the complete paraplegic patients (21.3%) and lowest among the incomplete or minimal deficit patients (2.6%). Our findings confirm earlier reports by Chen et al . [10] and Ragnnarson K et al . [11]. The great majority of patients without neurological deficit were treated with bed rest for a period of 4-6 weeks in this series. There was only one out of 215 patients in this group who developed PE a few days after surgical stabilization. We have found no other reports in the English literature about the incidence of thromboembolism in neurologically intact patients treated conservatively with 4-6 weeks of bed rest. The significant statistical difference in incidence between the neurologically intact and the neurologically impaired (p<0.01) suggests that the effects of the neurological impairment such as paralysis, and possibly also the neurological impairment itself, are the major risk factors for the development of VTE. Bed rest alone with adequate prophylaxis against VTE does not seem to increase the risk of VTE in patients with spinal injuries with and without neurological impairment.
References
- Tribe CR (1963) Causes of Death in Early and Late Stages in Paraplegia. Paraplegia 1: 19-47.
- Walsh JJ, Tribe CR (1965) Phlebo-thrombosis and Pulmonary Embolism in Paraplegia. Paraplegia 3: 209-213.
- Green D, Chen D, Chemiel JS, Olsen NK, Berkowitz M et al. (1994) Prevention of Thromboembolism in Spinal Cord Injury; Role of low molecular weight heparin. Arch Phys Med Rehabil 75(3):290-292.
- Green D, Twardowski P, Wei R, Radmaker AW (1994) Fatal pulmonary embolism in spinal cord injury; Chest 105(3): 853-5.
- De Vivo MJ. Krause JS. Lammertse DP (1999) Recent Trends in Mortality and Causes of Death among Persons with Spinal Cord Injuries. Arch Phys Med Rehabil 80(11): 1411-1419.
- Waters RL, Meyer PM, Adkins RH, Felton D (1999) Emergency, Acute, and Surgical Management of Spine Trauma. Arch Phys Med Rehabil 80(11): 1383-1390.
- (1997) Consortium for spinal cord medicine, Prevention of Thromboembolism in Spinal Cord Injury, Washington (DC) Paralysed Veterans of America.
- Thumbicat P, Poonnoose PM, Balasubrahmaniam, Ravichandran G, McClelland (2002) A comparison of Heparin/Warfarin and Enoxaparin Thromboprophylaxis in Spinal Cord Injury: The Sheffield Experience. Spinal Cord 40(8): 415-420.
- Geerts WH, Pineo GF, Hett JA, Bergqvist D, Lassen MR et al. (2004) Prevention of Venous Thromboembolism, the seventh ACCP cnference on antithrombotic and thrombolytic therapy; Chest 126(3): 338S-400S.
- Chen D, Apple DF, Hudson LM, Bode R (1999) Medical complications during acute rehabilitation following spinal cord injury – Current experience of the model systems; Arch Phys Med Rehabil 80(11): 1397-1401.
- Ragnarsson KT, Hall KM, Wilmont CB, Carter RE Management of pulmonary, cardiovascular and metabolic conditions after spinal cord injury. In: Stover SL.
- Bergqvest D, Lowe GD, Berstad A, Haas S, Hirsh J et al. (1992) Prevention of venous thromboembolism after surgery: a review of enoxaparin, Br. J. Surg 79: 495-498.
- Merli GJ, Crabbe S, Pharm D et al. (1993) Aetiology, Incidence and prevention of Deep Vein Thrombosis in Acute Spinal Cord Injury Arch. Phys. Med. Rehab 74: 1199-1205.
- (1986) Consensus Conference, Prevention of Venous Thrombosis and Pulmonary Embolism J Am Med Ass, 256: 744-749.
- Kim SW, Charallel JT, Park KW, Bauerle LC, Shang CC et al. (1994) Prevalence of deep Vein Thrombosis in patients with chronic Spinal Cord Injury. Arch Phys Med Rehabil 75(9): 965-968.
- Fletcher DJ, Taddonio RF, Byrne DW (1995) Incidence of acute care complications in vertebral column fracture patients with and without spinal cord injury; Spine 20(10): 1136-46.






























