The practicality of Telemedicine in Orthopaedics: Perspectives from a Developing Nation
Anil Kapoor, Bharath Patil*, Manharjot Singh Malhi, Ramesh Kalappagol, Naveen Mittal and Gagan DJ
Department of Orthopaedics, Government Medical College & Hospital Chandigarh, India
Submission: January 08, 2021;Published: January 19, 2021
*Corresponding author: Bharath Patil, Department of Orthopaedics, Government Medical College & Hospital Chandigarh, India
How to cite this article: Anil K, Bharath P, Manharjot S M, Ramesh K, Naveen M, et al. The practicality of Telemedicine in Orthopaedics: Perspectives from a Developing Nation. JOJ Orthoped Ortho Surg. 2021; 2(5): 555600. DOI:10.19080/JOJOOS.2021.02.5555600
Abstract
Background: Telemedicine is a new concept for the management of non-communicable diseases after the suspension of out-patient services due to COVID-19 pandemic. However, this is an evolving idea which requires further improvement.
Purpose of the study: The aim of this study was to highlight the issues faced by the patients and the treating doctors during telemedicine consultation.
Material methods: This was a pilot study conducted in the Department of Orthopaedics. A total of 558 patients who called for telemedicine consultation were enrolled in the study. The number of patients who were advised physical examination due to various reasons like non-availability of smart phones, patients who were unable to explain their problems or those requiring physical examination were noted.
Results: 405 out of 558 patients were managed successfully through the telemedicine services. However, 153/185 (27.5%) patients needed physical review. Out of these 153 patients, only 33 (21%) of them needed a clinical examination. Rest of them either did not have a smartphone or were not able communicate properly or were unable to send good quality radiographs.
Conclusion: Telemedicine can be an important tool during this COVID-19 pandemic; however, this field still requires many improvements and more so in a developing country like India where telemedicine is a new state of art concept.
Keywords: Telemedicine; COVID-19; Orthopaedics; Pandemic
Introduction
In the era of COVID-19 the focus of entire health system is on the prevention of infection and management of morbidities and mortalities related to COVID-19 infection. To accomplish this, aim various resources have been channelized throughout the world including the diversion of the specialist doctors from various branches [1,2]. Due to this diversion of medical resources, the routine out-patient department services were completely shut down. Many patients were unable to access and receive their routine medical care. To encounter this major problem many hospitals throughout the world opted for telemedicine services [3-5]. However, the scenario is different in developing countries like India where the people belonging to lower economic status are completely dependent on government hospitals for management of their ailments. Therefore, in developing countries telemedicine cannot be the solution for all the health-related problems due to illiteracy, non-availability of smart phones, difficulty in accessing to the internet and computers, and lack of awareness amongst the lower income people [6]. The present study was conducted with an aim to highlight the issues faced by the patients and the treating doctors during telemedicine consultation in India.
Material and Methods
The data for present study was collected prospectively from the Department of Orthopaedics. All the patients who contacted the health care system via telephones (landline or mobile phones), WhatsApp, E-mail and video-call were enrolled in the present study. The details of the diseases were listened to telephonically and patients were asked to send relevant reports and radiographs via online communication medium. The tools used by us included pictures of the radiographs, wound and incision site pictures, videos of patient’s gait, range of motion and pain scales. Patients were advised treatment according to his/her disease. And for the patients who could not explain their problems completely or those who did not have any access to smartphones/computers for sending multimedia pictures were advised to seek medical healthcare either at their local hospital or in the emergency department depending upon the severity of their illness.
Results
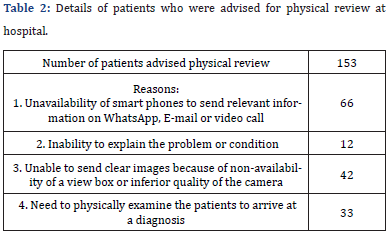
The mean age was 34.04±21.9 years. Of the 558 patients enrolled, 247 were males and 311 were females. Nearly 3/4th of the patients were successfully managed via telemedicine services, however 153 patients had to attend the hospital for various reasons as mentioned. (Table 1 & Table 2).

Discussion
The principle finding of the present study was that 12% of the patients could not be advised treatment because of lack of access to smart phones. Telemedicine program is a new concept for India [7], however, in western countries this practice has been going on for more than decades [8,9]. Such programs cannot be created over night as it requires a lot of public awareness and advertisement so that the services are being utilized by majority of the population.
A good infra-structure is required for effective and smooth running of these system and most important thing is to ensure the availability of resources on both sides that is the patients as well as the hospitals. Telemedicine can be very useful especially during these kind of pandemics as it protects both the doctors and patients from coming in contact with each other and other population by avoiding the need to travel to the hospitals and thus reducing the risk of infection. However, it is still not a foolproof method as there are large lacunae which prevent the effective running of this program and we believe there is still lot of scope for improvement in this system [10,11].
Following problems were faced by doctors and patients during this study which needs to be addressed.
Doctor’s considerations:
a) Lack of good internet connection on patient’s side leading to inferior quality of video.
b) Lack of Clinical examination which forms an important part of evaluation and therefore there are more chances of missing a condition leading to misdiagnosis and its medico-legal implications may deter adoption of telemedicine services by many health care providers [12-14].
c) On follow-up, lack of data from the previous visit, which used to form an important part in the disease management during the pre-COVID era and helped in continuation of care.
d) Difficulty in explaining the problems and symptoms related to the disease and inability to understand the treatment on telephones.
e) And the medico-legal implications of care and treatment provided Patient’s consideration:
a. Unavailability of smart phones and good internet connection amongst the lower income group.
b. Elderly patients who did not have social support and cooperation usually found it difficult in understanding the instructions given by the doctor.
c. Inability to send good quality x-ray pictures due to unavailability of x-ray view box.
However, these problems are faced throughout the world, but in developing countries they are magnified due to lack of resources and illiteracy [15]. Telemedicine is a new concept for Indian healthcare system which requires a good infrastructure and public awareness. Telemedicine can be an important tool even after COVID-19 era, however at present there is a lot of scope for improvement in this field in the form of promoting the so-called digital health. We believe the outreach to such services can be increased by publishing advertisements in the local newspapers and through television channels and videos which can be aired educating people, for example on how to utilize the new citizen centric initiative recently taken by the government the e– sanjeevani OPD module [16]. Infrastructure must be setup at every Primary Health Care facilities (PHC) and trained staff can be deployed for assisting people who are not well versed with using the technology or lack access to it and the trained doctors in the PHC will be able to better communicate and convey with the specialists from a tertiary care set-up and thus we can extend its reach to the neediest population like the rural and the small community pockets and provide health care to everyone.
Conclusion
Telemedicine can be an important tool during this pandemic situation in providing uninterrupted care to the patients, however this requires more improvement especially in countries like India where telemedicine is still a new evolving concept.
References
- Haut ER, Leeds I, Livingston DH (2020) The Effect on Trauma Care Secondary to the COVID-19 Pandemic: Collateral Damage from Diversion of Resources. Ann Surg 272(3): e204-e207.
- Horton R (2020) Offline: Don't let COVID-19 divert us completely. Lancet (London, England) 395(10236):1534.
- Vaishya R, Bahl S, Singh RP (2020) Letter to the editor in response to: telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. DiabetesMetab Syndr 14(4):687-688.
- Tanaka MJ, Oh LS, Martin SD, Berkson EM (2020) Telemedicine in the era of COVID-19: the virtual orthopaedic examination. JBJS 102(12):e57.
- Haider Z, Aweid B, Subramanian P, Iranpour F (2020) Telemedicine in orthopaedics and its potential applications during COVID-19 and beyond: A systematic review. J Telemed Telecare 1357633X20938241.
- https://www.hindustantimes.com/world-news/lack-of-mobile-phones-hits-healthcare-access-for-poor-oxford/story-4OI2GDBlse2IlXBGWp9pRK.html.
- Iyengar KP, Jain VK (2020) COVID-19 and the role of telemedicine in delivering health care.
- Wootton R (2001) Telemedicine. Bmj 323(7312): 557-560.
- Tarassenko L, Peggram C, Hayton P, Gibson O, George A et al. (2006) Telemedicine system. Google Patents.
- Iyengar K, Jain VK, Vaishya R (2020) Pitfalls in telemedicine consultations in the era of COVID 19 and how to avoid them. Diabetes & Metabolic Syndrome: Clinic Res Reviews 14(5): 797-799.
- Burroughs M, Urits I, Viswanath O, Simopoulos T, Hasoon J (2020) Benefits and shortcomings of utilizing telemedicine during the COVID-19 pandemic. Bayl Uni Medl Cent33(4): 699-700.
- Kuszler PC (1999) Telemedicine and integrated health care delivery: compounding malpractice liability. Am J Law Med. 25(2-3):297-326.
- Stanberry B (2006) Legal and ethical aspects of telemedicine. J Telemed Telecare12(4):166-175.
- Lateef F (2011) The practice of telemedicine: medico-legal and ethical issues. Ethics Med 27(1):17-24.
- Haenssgen MJ (2018) The struggle for digital inclusion: Phones, healthcare, and marginalisation in rural India. World Dev. 104:358-374.
- https://esanjeevaniopdin/






























