Massive Transfusion Protocol (MTP) Started by Pre-Hospital Equipe: An Italian Experience
Simone Celi1*, Marco Botteri1 and Alberto Piacentini2
1AAT 118, ASST degli Spedali Civili di Brescia, Italy
2Cardio-thoracic ICU, Jilin Heart Hospital, China
Submission: August 01, 2019;Published: November 18, 2019
*Corresponding author: Simone Celi, AAT 118, ASST degli Spedali Civili di Brescia, Brescia, Italy
How to cite this article: Simone Celi, Marco Botteri, Alberto Piacentini. Massive Transfusion Protocol (MTP) Started by Pre-Hospital Equipe: An Italian Experience. JOJ Orthoped Ortho Surg. 2019; 2(3): 555590. DOI: 10.19080/JOJOOS.2019.02.555590
Abstract
Severe trauma is one of leading causes of death and injury in Europe. Administration of tranexamic acid (TXA), and blood products, in life-threatening traumatic shock has been already proven to be beneficial [1,2]. At our institution a massive transfusion protocol (MTP) has been developed. On scene triggering criteria are immediate administration of one TXA gram intravenously on scene, and alerting destination hospital for immediate availability need of ready blood products at arrival.
Keywords: Massive Transfusion Severe trauma blood products hemoglobin blood transfusion
Methods
prospective evaluation of all MTP activations over a 6 years period (October 2012-July 2018).
Criteria to identify major trauma patients are:
a) SBP < 90 mmHG with failure response to a fluid bolus
b) HR >110 bpm
c) active bleeding not controllable
d) penetrating trauma
e) 3th/4th ATLS shock classification
To reach the target, has been analyzed every case which patients with MTP activated have received blood products and mechanism of injury, age, sex, SBP, HR, hemoglobin, blood products transfused has been collected
Results
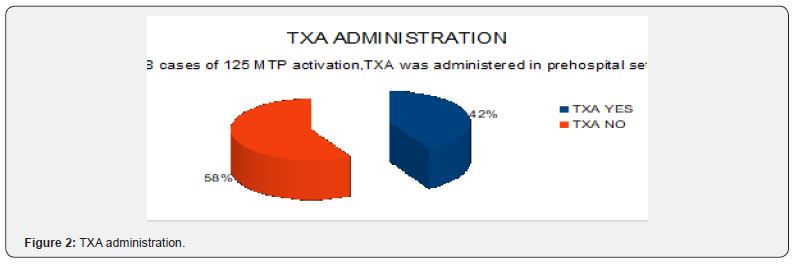
162 MTP total candidates, administration of TXA resulted in 68 patients (42%), 125 patients received blood products (77.1%) (Figures 1 & 2).
Specific functions of the teres minor include lateral or external rotation of the arm, rotating the head of the humerus outward [1]. This results in the abduction of the arm [1]. The infraspinatus muscle has similar functions to the teres minor and is shown to have higher activity than the teres minor during flexion, abduction, and scaption of the shoulder via EMG and MRI data [6]. Both muscles also contribute to the anterior stability of the glenohumeral joint when the shoulder is abducted andexternally rotated, restricting anterior translation of the humeral head on the glenoid and thus reducing strain on anterior joint structures [2]. The strength and function of the teres minor can be tested using the hornblower’s test or sign [10]. This is conducted with the examiner initially supporting the patient’s arm at 90 degrees of abduction in the scapular plane [11]. The elbow is then flexed to 90 degrees and the patient is asked to the rotate the forearm externally against resistance [12]. If the shoulder cannot be externally rotated in this position, it shows a positive hornblowers sign and indicates teres minor dysfunction [13]. Walch found that, in a study of 54 patients, the hornblower’s sign had 100% sensitivity and 93% specificity for teres minor damage [13]. In another study, it was also concluded that maximum external rotation in abduction of the arm is a reliable method to evaluate activity in the teres minor [14].

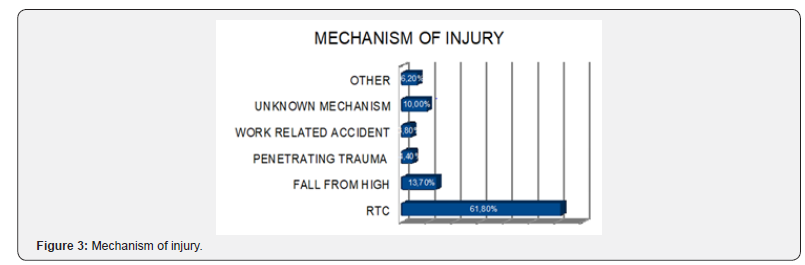
MOI
Road traffic collision (RTC) 61,8%, fall from height 13,7%, penetrating trauma 4,4%, work related accidents (3,8%), unknown mechanism 10%, medical conditions 2,4% and “other” 3,8%. Mean patient age 46 years (range 15-90). MTP erroneously activated in 4 patients due to medical causes.
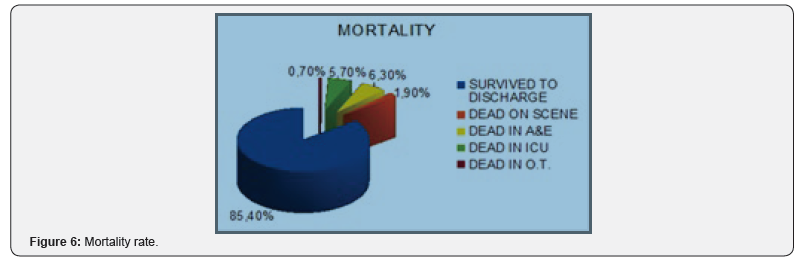
Mortality and morbidity
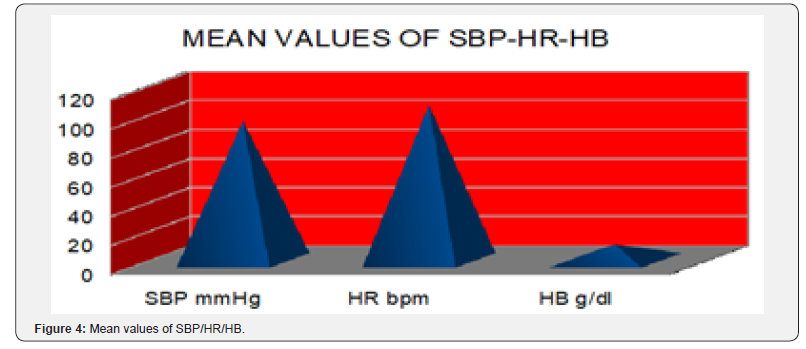
Patients survived to hospital discharge 85,4%, declared dead on scene (1,9%), died in A&E 6,3%, in ICU (5,7%) and in O.T. (0,7%) (Figure 3). Mean SBP was 96 mmHg (range 40-150), mean HR 107 bpm (range 32-180) (Figure 4).
Observed transfusion data
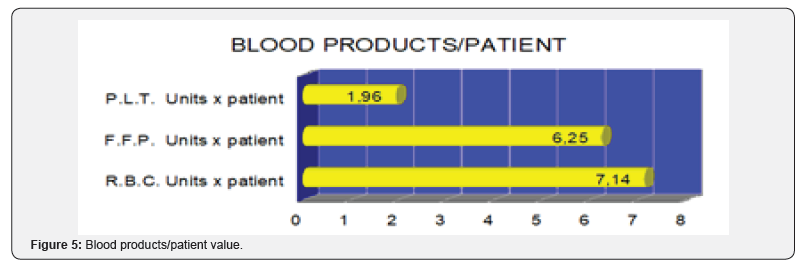
RBC (879) → 7.14 x patient
FFP (676) → 6.25 x patient
PLT (61) → 1.96 x patient (Figure 5 & 6).
Conclusion
Development of simple protocol allowed immediate identification of severely traumatized patients who required immediate resuscitation with blood products directly in emergency department.
References
- Shakur H, Roberts I (2010) Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomized, placebocontrolled trial. Lancet 376(9734): 23-32.
- Weaver AE, Hunter-Dunn C (2016) The effectiveness of a Code red transfusion request policy initiated by pre-hospital physician. Injury 47(1): 3-6.






























