Mid-term Quality of Syndesmosis Reduction According to the Method used for Fixation of an Acute Ankle Syndesmosis Rupture
Mélissa Laflamme1, Marie Claude Leblanc1, Anne Marie Bédard1 and Stéphane Pelet2,3*
1Department of Orthopedic Surgery, CHU de Québec-Centre Hospitalier de l’Université Laval (CHUL), Canada
2Department of Orthopedic Surgery, CHU de Québec-Hôpital Enfant-Jésus, Canada
3Centre de recherche FRQS du CHU de Québec-Hôpital Enfant-Jésus, Canada
Submission: August 27, 2019;Published: September 18, 2019
*Corresponding author: Stéphane Pelet, Department of Orthopedic Surgery, Centre de recherche FRQS du CHU de Québec-Hôpital Enfant-Jésus, Canada
How to cite this article: Mélissa Laflamme, Marie Claude Leblanc, Anne Marie Bédard, Stéphane Pelet. Mid-term Quality of Syndesmosis Reduction According to the Method used for Fixation of an Acute Ankle Syndesmosis Rupture. JOJ Orthoped Ortho Surg. 2019; 2(3): 555588. DOI: 10.19080/JOJOOS.2019.02.555588
Abstract
Background:Syndesmotic malreduction rate following an acute ankle syndesmosis rupture fixation vary widely between studies depending on the imaging modality chosen and the criteria used. The purpose of this study is to compare the rate of syndesmosis malreduction in patients surgically treated for an acute unstable syndesmosis rupture with either a 3.5mm quadricortical metallic screw or a suture-button device (Tightrope®, Arthrex, Naples, FL).
Methods: A prospective and retrospective cohort study was conducted to compare the rate of syndesmosis malreduction in patients surgically treated for an acute unstable syndesmosis rupture with either a 3.5mm quadricortical screw or a suture-button device. Patients enrolled in a previous prospective randomized trial were deemed eligible for this study. Sixteen patients in the static group and 14 patients in the dynamic group were enrolled in this study. The two groups were similar regarding demographic, social and surgical data. Mean follow-up was 3.7 (range 2.5-5.3) years. Radiographic and clinical measures were prospectively collected. The primary outcome measure was the rate of syndesmosis malreduction observed on a CT-scan of both ankles. Main functional measures were the Olerud-Molander and AOFAS scores.
Results: The malreduction rate measured on CT scan images was 1/14 (7.1%) for the dynamic implant and 3/16 (18.8%) for the static implant (p=.28). No correlation could be drawn between malreduction and functional outcomes at mid-term follow-up. There were significantly more cases of syndesmosis ossification in the screw fixation group.
Conclusion: The syndesmosis malreduction rate following fixation of an acute syndesmotic rupture is higher in the screw fixation group compared to the dynamic device group without reaching statistical significance. There is no negative impact of this malreduction on the mid-term functional outcomes. Studies with more patients and with longer follow-up periods are required to better assess those issues.
Level of evidence: II
Keywords: Syndesmosis Syndesmotic screw Dynamic fixation Syndesmosis malreduction
Introduction
Syndesmotic malreduction rate following an acute ankle syndesmosis rupture fixation vary widely between studies depending on the imaging modality chosen and the criteria used. Literature demonstrated malreduction rate between 16 and 52% [1,2]. This complication can lead to early degenerative changes of the tibiotalar joint as it modifies the weight-bearing surface area of the ankle joint. Interestingly, when the syndesmotic screw is removed, in most cases, the syndesmotic malreduction realigns to normal values [3]. As the suture-button device is dynamic, it is not known if this implant is more forgiving and offer a better alignment of the fibula in the tibial incisura with the micromotions allowed. The purpose of this study is to compare the rate of syndesmosis malreduction in patients surgically treated for an acute unstable syndesmosis rupture with either a 3.5mm quadricortical screw or a suture-button device. With the use of mid-term radiographic and clinical measures, the hypothesis that malreduction would impair functional outcome was also evaluated.
Materials and Methods
Study design
A prospective and retrospective cohort study was conducted at an academic Level I trauma center to compare the rate of syndesmosis malreduction in patients surgically treated for an acute unstable syndesmosis rupture with either a 3.5mm quadricortical screw or a suture-button device (Tightrope, Arthrex Inc, Naples, FL). Radiographic and clinical measures were prospectively collected. The primary outcome measure was the rate of syndesmosis malreduction observed on a CT-scan of both ankles. Main functional measures were the Olerud-Molander score and the AOFAS score. The hypothesis that malreduction would impair functional outcome was also evaluated.
Patient selection
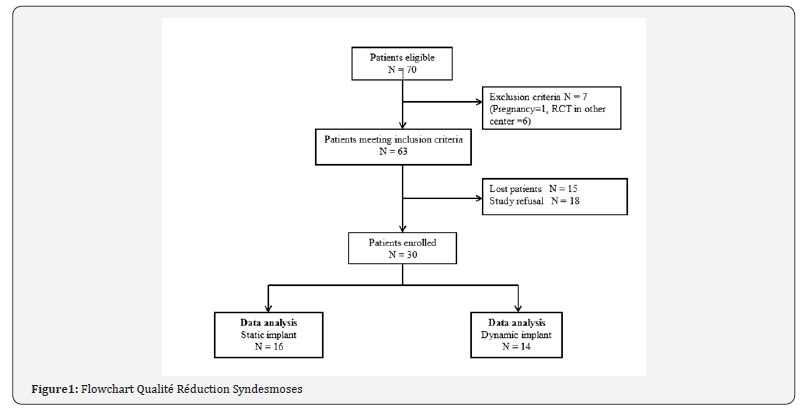
Patients enrolled in a previous prospective randomized trial (RCT) comparing the functional outcome after stabilization of an acute syndesmosis rupture with either a 3.5mm quadricortical screw or a suture-button device were deemed eligible for this study. After IRB approval and written consent, specific assessment was achieved through a bilateral ankle computed tomography, a series of functional tests (Olerud-Molander, AOFAS) and a physical examination. Measures were compared between patients with static syndesmosis fixation or dynamic fixation. Patients were excluded if they had: a new injury to the lower limb (ipsi- or controlateral) during the interval between the end of the RCT and the control visit, pregnancy, or if they were enrolled in another center for the previous RCT (in order to standardize CT measures) or unable to comply with the study protocol (e.g. cardiac impairment, mental retardation). (Figure 1) illustrates the flow diagram of the study.
Study procedure
Eligible patients were contacted by phone by one of the investigators to explain the study. Once a verbal consent was obtained, patients were invited to the hospital to receive further information and eventually participate in the study. Participant visits took place between June 2012 and January 2013. Duringthis single visit, each patient was given ample details about the study and any other information requested in order to obtain an informed written consent to participate in the study. The study had been previously approved by the institutional ethics review board and was conducted in accordance with guidelines for the conduct of research on human subjects.
Data collection
Retrospective data: Patient’s medical charts as well as research chart from the previous RCT were reviewed by one of the investigators. Demographic data, fracture characteristics, results of functional and clinical tests, and radiographic data were collected for each eligible patient.
Prospective data: A single blinded, independent, trained medical interviewer who was not involved in the study analysis evaluated the patients. All the data were collected during the single visit to the hospital. The specific assessment was achieved with the use of a CT-scan of both ankles, radiographic imaging of the ankle (AP, mortise and lateral views) and functional questionnaires.
Radiographic evaluation
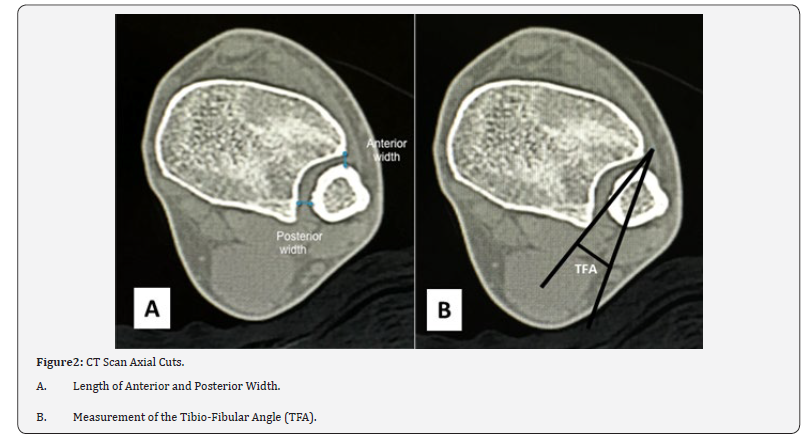
CT scan measures: Malreduction of the syndesmosis was assessed on CT-scan of both ankles with use of a standardized technique. Sequential 7-mm-thick axial cuts were taken fromthe same scanner machine (patient supine, both ankles tied) from the mid-shaft tibia to the subtalar joint. The measures were obtained 1cm proximal to the tibiotalar joint line: [4] the anterior width corresponds to the distance between the tip of the anterior tibial tubercle and the nearest point of the fibula, and the posterior width is the distance between the medial border of the fibula and the nearest point of the lateral border of the posterior tibial tubercle (Figure 2A). The residual diastasis (RD) is the mean of anterior and posterior differential width (difference between normal and injured side). Malreduction of the syndesmosis was defined as a mean RD ≥ 2mm [5]. Fibular rotation was measured with the tibio-fibular angle (TFA) on the same CT-scan axial cut. TFA is the angle between a line drawn between the anterior and posterior point of the incisura and a line drawn in the fibula representing its orientation [6] (Figure 2B). Malrotation of the distal fibula was proposed as a difference in the TAF between the two ankles ≥15 degrees [7].
Standard X-rays: Plain radiographs of both ankles were taken in the AP, mortise and lateral views. Fixation failure, loosening, degenerative changes and heterotopic ossifications were recorded. The reduction of the syndesmosis was assessed with the medial clear space (MCS) and the tibio-fibular clearspace (TFCS). MCS is considered normal if less than 4mm, and TFCS if less than 6mm on both AP and mortise views. Talocrural angle was also measured to make sure fibular length was adequate. Normal talocrural angle was established to be between 8 and 15 degrees. Two investigators read all scans and radiographs once. They were both blinded to the identity of the patient and its functional results. The mean of both values was used to define the quality of reduction of the syndesmosis. If a difference ˃2mm or 5 degrees was present between the two measures, two other independent measures were taken from the same investigators and the mean of the two closest values was used.
Measures of function: Ankle function was evaluated with the Olerud-Molander score (OM) [8] and the American Orthopedic Foot and Ankle Society score (AOFAS) for the ankle-hindfoot [9]. OM is the only reliable and validated score for ankle fractures in the literature [10]. It consists of nine functional items divided in three categories: subjective complaints (pain, stiffness and swelling), performances (stair-climbing, running, jumping, squatting) and impact on daily-living status (walking aids, work or activities of daily life). The scale ranges from 0 to 100 with 100 being the best functional result and 80 the lower limit for good functional results. A 15-point difference is considered clinically significant. The AOFAS score is not specifically validated for ankle fractures but is widely used by many surgeons for ankle and hindfoot problems [11]. It consists of objective and subjective parameters on a numeric scale allowing an evaluation of the function (seven criteria), alignment (one criteria) and pain (one criteria), for a maximum of 100 points. Ankle range of motion of both ankles was measured with a goniometer.
Statistical analysis: Data were processed and analyzed with Excel (version 2.0, Microsoft Office Professional 2007, Redmond, Washington). Continuous variables are reported as the mean and the standard deviation. Comparisons of proportions were based on the Fisher exact test. A t-test was used to comparethe functional results. All tests were two-sided, and the level of significance was set at p˂0.05 [12].
Results
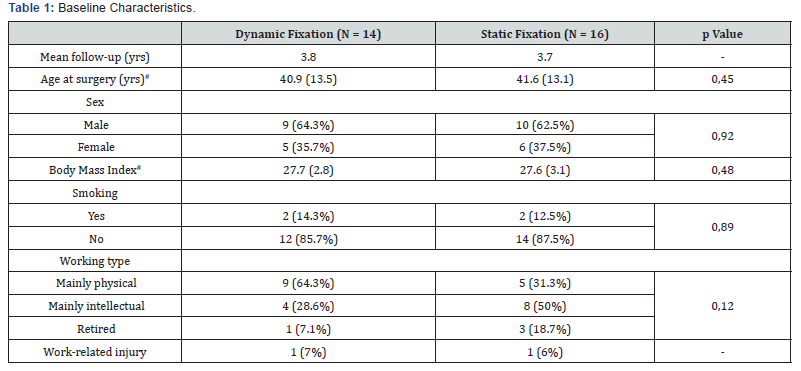
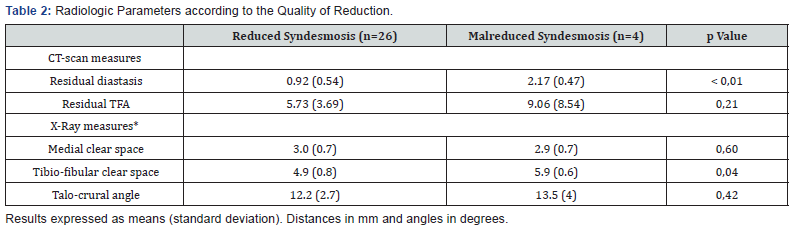
70 patients participated in the RCT. Seven were initially excluded (1 pregnancy, 6 from other centers). From the 63 left, 15 patients could not be reached and 18 refused to participate. Therefore, 30 patients were enrolled in the current study. Fourteen patients initially fixed with a Tightrope® (Arthrex, Naples, FL) and 16 patients treated with one 3.5mm quadricortical screw signed the consent form (Figure 1). Mean time between the surgery and the last evaluation was 3.7 years (range, 2.5-5.3). The demographic data between the two groups were similar for age at surgery, sex, body mass index (BMI), smoking and work-related injury. More patients in the dynamic fixation group performed a physical work (Table 1). Between the end of the RCT and this study, six patients had their screw removed (mainly for pain) and four patients their suture button removed (three for pain and skin irritation and one for superficial infection). Four patients presented a significant syndesmosis malreduction on the CT-scan according to our criteria: one patient (7.1%) in the dynamic fixation group (increased RD) and three patients (18.8%) in the screw fixation group (two with an increased RD and one with malrotation) (p=0,60). The mean RD in patients with a reduced syndesmosis is less than 1mm (0.92±0.54) and the mean TFA difference 5.73 degrees (±3.69). Interestingly patients with a malreduced syndesmosis on CTsan also have an increased tibio-fibular clear-space (p=0,04). Table 2 presents the radiologic findings according to the quality of reduction, and Table 3 the individual measures for the four patients with a malreduced syndesmosis [13].

Values expressed in mm for distances and degrees for angles.
Nr = randomization number; MCS = medial clear space
TFCS = tibio-fibular clear space
TCA = talo-crural angle
AW = anterior width
PW = posterior width
RD = residual diastasis
RTFA = residual tibio-fibular angle.
We observed a broken screw in seven patients, leaving only three patients with an intact screw at this mid-term followup. Interestingly there is no relationship between an absent or broken screw and syndesmosis malreduction (p=0,49). Broken suture-buttons cannot be seen on x-rays or CT-scan, but no displacement of the buttons (either on the medial or lateral side) was observed (when compared to the last radiographs from the RCT). An absent suture-button is not related to a malreduced syndesmosis (p=0,27). Partial ossification of the syndesmosis was significantly more common in the screw fixation group (n=9, 56.3%) compared to the dynamic fixation group (n=3, 21.4%; p=0,05) [14]. No synostosis was observed. Five patients showed a consistent osteolysis around the screw path, and only one in the dynamic fixation group (p=0,1). Patients in the dynamic fixation group presented a better clinical outcome at this mid-term follow-up for the Olerud-Molander score (96.7±5.3 vs 93.1±5.9, p=0,18) and the AOFAS (96.5±6.9 vs 92.3±5.0, p=0,1), without achieving statistical significance. The clinical scores were not influenced by the quality of reduction: Olerud-Molander reduced 96.4±.5.5 vs malreduction 100±0, p=0,32, and AOFAS reduced 96.2±3.9 vs malreduction 93.3±8.7, p=0,91.
Discussion
Since anatomic reduction of the syndesmosis after an acute rupture is the only predictor of functional outcomes, [15] needless to say that obtaining and maintaining anatomic reduction is a crucial aspect of the surgical procedure. Untreated or improper reduction of the syndesmosis injury will get to a loss of tibio-talar congruency, ankle instability and in the longterm, to invalidating degenerative changes. The prevalence of malreduction of the distal tibio-fibular joint varies greatly in the literature depending on the imaging modality and the criteria used and is much higher than previously thought. Schwarz [2] had 16% malreduction out of 37 patients fixed with screw on post-operative CT scan. In Gardner’s study, [16] 13 of their 25 patients (52%) had a malreduced syndesmosis on post-operative unilateral CT scan. Weening [15] had a 16% malreduction rate out of 51 patients on plain radiograph only. As for Mukhopadhyay, [5] 42% of their 19 patients had malreduction on bilateral CT scan. This prospective study compared the rate of malreduction of the syndesmosis after fixation with two different types of implants. Our results indicate that there are more syndesmosis malreduction with screw fixation compared to the dynamic fixation. Our possible explanation is that the suture-button allows for some micromotions that might help the positioning of the fibula more anatomically in its incisura if the fibular fracture is well reduced. This might be more forgiven to the surgeon than when the distal tibio-fibular joint is not perfectly reduced and rigidly fixed with a screw. Most biomechanical studies have previously demonstrated the advantages of the dynamic fixation of the syndesmosis with restoration of the physiologic movements mainly in the sagittal plan [16-20]. Other clinical studies demonstrated good clinical results with this implant. Coetzee, [21] with an underpowered randomized study, and Laflamme [22] in a randomized controlled trial, recently showed clinical advantages to the dynamic fixation compared to the screw.
Traditional radiographic measurements on AP and mortise views should not be relied on solely for determining the syndesmosis status and the mortise stability, [23] a principle that can reasonably be apply to post-operative syndesmosis fixation follow-up. Axial CT scan clearly shows the tibio-fibular relationship and can assesses coronal and sagittal translation as well as rotation whereas plain x-rays only show coronal malreduction. Ebraheim7 showed that all diastasis of at least 2 mm were visible on CT scan, but as much as 3 mm were not detectable on routine radiographs. Gardner [24] also showed the poor ability of radiographic measurements to assess the syndesmosis postoperatively with sensitivity of 31% and specificity of 83% compared to CT scan. Since subtle syndesmosis malreduction can increase the tibio-talar contact area to a great amount, imaging used must be able to detect small changes. As such, postoperative CT scan is a powerful tool in the diagnosis of postoperative malreduction of the syndesmosis. Some authors [25] now use routine postoperative CT scan bilaterally to assess the reduction and identify potential problems early. Our results confirm the results of previous studies. Naqvi [26] also showed a lower malreduction rate with the suture-button compared to screw fixation in his series of 46 patients. In fact, none ofthe patient fixed with the dynamic device were malreduced, compared to five patients in the screw fixation group (21.7%). To note, all of the patients in the screw fixation group had their screw removed at approximately 10 weeks, a major difference from our study where most of the screw stayed in place. We had three malreductions (18.8%) in the screw fixation group, two for an increased diastasis and one for a malrotation of the fibula in the incisura. Naqvi [26] did not evaluate the malrotation in his study, therefore his results might underestimate the true malreduction rate. He defined malreduction as more than 2mm difference between the normal and injured ankle in the posterior measurement alone. For the evaluation of the diastasis, our study used the identification points in Elgafy’s study [4] and the criteria defined by Mukhopadhyay [5].
This brings up the issue that there is no clear definition of what is a syndesmosis malreduction in the literature. Gardner [16] arbitrary determined that a 2mm difference between the anterior and posterior measurements in the injured ankle was diagnostic of a malreduction, but this does not consider the anatomical variability of the distal tibio-fibular joint. This might even have led to an overestimation of the real malreduction rate because of some possible false positive results as described by Mukhopadhyay [5]. Another measurement method comes from Elgafy’s publication [4]. With 100 CT scan of normal ankles, he stated that the mean width of the distal tibio-fibular syndesmosis anteriorly between the tip of the anterior tibial tubercle and the nearest point of the fibula was 2mm, and that the mean width of the distal tibio-fibular syndesmosis posteriorly between the medial border of the fibula and the nearest point of the lateral border of the posterior tibial tubercle was 4mm. Interestingly, Nault [6] had different numbers for the same measurements. Her values of 4 and 8mm for absolute distance between tibia and fibula anteriorly and posteriorly respectively are two times larger, but with the same ratio between both values. Their range of normal values is wide, with the anterior measurement between 1.5 and 6.4mm and the posterior value between 2.1 and 11.5mm.
As for rotational malalignment, we used Nault’s method, [6] but there are other ways to measure this parameter. Marmor’s technique [27] is the angle between a line drawn along the long axis of the fibula and a vertical line parallel to the posterior facet of the tibial incisura. The normal value in the article is 25.6±5.6 degrees (SD). No diagnostic criteria exist in the literature for this parameter either, but Vasarhelyi [7] stated that 15 degrees of malrotation may be significant using another method of measurement. He based his cut-off on the poorer functional results, but mainly according to the threshold for the femoral and tibial torsional malalignment. According to Nault, [6] the range of normal values for rotation vary between -1.1 and -15.1 degrees. We could not identify a difference in the functional scores between the reduced and the malreduced syndesmosis. Our small sample size is probably the main reason. This aspect was well demonstrated by many authors [26,15] and we agree with those results. Obtaining and maintaining anatomic reduction will lead to more physiologic load distribution and ankle biomechanics. The loss of reduction of the ankle syndesmosis can lead to mortise widening and osteoarthritis [28]. We identified a significant difference in the number of partial ossification of the syndesmosis between the two groups. The reason for this is unknown. The initial trauma or the osseous debris from the drilling cannot explain this difference because they are similar between the groups. Wikeroy [29] noted seven out of 48 patients with a synostosis on CT scan at a mean followup of 8.4 years after ankle and syndesmosis fixation. All those patients had poorer functional scores compared with patients without synostosis. All their patients had their syndesmosis disruption initially fixed with screw, and the number of cortices did not seem to play a role. None of our patients had a complete bony bridge, nor we could identify a difference in outcomes, but longer follow-up would be required. The main strength of this study is the reduction assessment with bilateral CT scan to take into account for the possible anatomic variabilities that were demonstrated in other studies [30]. Moreover, our cohort of patients comes from a prospective randomized study on the type of syndesmosis fixation in acute injury. We also acknowledge some limitations. First, trying to contact patients from a previous study raises the possibility of a significant selection bias, with either patient doing well, or the opposite, the one with the worst results coming for the follow-up evaluation. We therefore looked at our previous results and found that the patients with the worst functional results were equally represented in both groups. In fact, patients with the lower results represented 40% of the dynamic fixation group and 50% of the screw fixation group. According to the medical records and a questionnaire to the other participating centers, none of the patient not included in the study had another surgery for their ankle. The last radiographs from the previous study were also looked at, but the quality of the reduction of their syndesmosis with CT scan is unknown [31]. Also, since no CT scan in the initial postoperative period was performed, it was not possible to compare the initial postoperative reduction and the CT scan at the last follow-up. This is a small cohort of patients. Therefore, there is not enough power to show a significant difference between the two treatment groups. Also, a longer follow-up period would be required to be able to identify any difference in the functional outcomes between the patients with a reduced and a malreduced syndesmosis. We think this difference will appear with longer follow-up giving the poor results shown in previous studies [32,7] and the biomechanical necessity of syndesmosis’s integrity.
Conclusion
The syndesmosis malreduction rate measured on CT scan is higher in the screw fixation group compared to the dynamic fixation group without reaching statistical significance. Screwfixation leads to a higher number of partial ossifications of the syndesmosis which could become significant in the long term. There is no negative impact of syndesmosis malreduction on the mid-term functional outcomes. Studies with more patients and with longer follow-up are required to better assess those issues. A more precise and uniform definition of syndesmosis malreduction in the literature is also required.
References
- Gardner MJ, Demetrakopoulos D, Briggs S, Helfet DL, Lorich DG (2006) Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int 27(10): 788-792.
- Schwarz N, Köfer E (2005) Postoperative Computed Tomography–Based Control of Syndesmotic Screws. Eur J Trauma 31: 266-270.
- Song DJ, Lanzi J, GrothA, Drake M, Orchowski JR, et al. (2014) The effect of syndesmosis screw removal on the reduction of the distal tibiofibular joint: A prospective radiographic study. Foot Ankle Int 35(6): 543-548.
- Elgafy H, Semaan HB, Blessinger B, Wassef A, Ebraheim NA (2009) Computed tomography of normal distal tibiofibular syndesmosis. Skeletal Radiol 39(6): 559-564.
- Mukhopadhyay S, Metcalf A, Guha AR, Mohanty K, Hemmadi S, et al. (2011) Malreduction of syndesmosis-Are we considering the anatomical variation? Injury 42(10): 1073-1076.
- Nault ML, Hébert-Davies J, Laflamme GY, Leduc S (2013) CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma 27(11): 638-641.
- Vasarhelyi A, Lubitz J, Gierer P, Gradl G, Rösler K, et al. (2006) Detection of fibular torsional deformities after surgery for ankle fractures with a novel CT method. Foot Ankle Int 27(12): 1115-1121.
- Olerud C, Molander H (1984) A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg 103(3): 190-194.
- Kitaoka H, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, et al. (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15(7): 349-353.
- Riegels Nielsen P, Christensen J, Greiff J (1983) The stability of the tibio-fibular syndesmosis following rigid internal fixation for type C malleolar fractures: an experimental and clinical study. Injury 14(4): 357-360.
- Button G, Pinney S (2004) A meta-analysis of outcome rating scales in foot and ankle surgery: Is there a valid, reliable, and responsive system? Foot Ankle Int 25(8): 521-525.
- Cottom JM, Hyer CF, Philbin TM, Berlet GC (2008) Treatment of Syndesmotic Disruptions with the Arthrex Tightrope: A Report of 25 Cases. Foot Ankle Int 29(8): 773-780.
- Cottom JM, Hyer CF, Philbin TM, Berlet GC (2009) Transosseous Fixation of the Distal Tibiofibular Syndesmosis: Comparison of an Interosseous Suture and Endobutton to Traditional Screw Fixation in 50 Cases. J Foot Ankle Surg 48(6): 620-630.
- DeGroot H, Al Omari AA, Ghazaly El SA (2011) Outcomes of Suture Button Repair of the Distal Tibiofibular Syndesmosis. Foot Ankle Int 32(3): 250-256.
- Weening B, Bhandari M (2005) Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 19(2): 102-108.
- Klitzman R, Zhao H, Zhang LQ, Strohmeyer G, Vora A (2010) Suture-Button Versus Screw Fixation of the Syndesmosis: A Biomechanical Analysis. Foot Ankle Int 31(1): 69-75.
- Miller R, Weinhold P, Dahners L (1999) Comparison of tricortical screw fixation versus a modified suture construct for fixation of ankle syndesmosis injury: a biomechanical study. J Orthop Trauma 13(1): 39-42.
- Seitz WH, Bachner EJ, Abram LJ, Postak P, Polando G, et al. (1991) Repair of the tibiofibular syndesmosis with a flexible implant. J Orthop Trauma 5(1): 78-82.
- Soin SP, Knight TA, Dinah AF, Mears SC, Swierstra BA, et al. (2009) Suture-Button Versus Screw Fixation in a Syndesmosis Rupture Model: A Biomechanical Comparison. Foot Ankle Int 30(4): 346-352.
- Thornes B, Walsh A, Hislop M, Murray P, O'Brien M (2003) Suture-endobutton fixation of ankle tibio-fibular diastasis: a cadaver study. Foot Ankle Int 24(2): 142-146.
- Coetzee J, Ebeling P (2009) Treatment of syndesmoses disruptions : A prospective, randomized study comparing conventional screw fixation vs Tightrope fiber wire fixation-medium term results. SA Orthopaedic Journal 8(1): 32-37.
- Laflamme M, Belzile EL, Bédard L, van den Bekerom MP, Glazebrook M, et al. (2015) A prospective randomized multicenter trial comparing clinical outcomes of patients treated surgically with a static or dynamic implant for acute ankle syndesmosis rupture. J Orthop Trauma 29(5): 216-23.
- Nielson J, Gardner MJ, Peterson MG, Sallis JG, Potter HG, et al. (2005) Radiographic measurement do not predict syndesmotic injury in ankle fracture: an MRI study. Clin Orthop Relat Res 436: 216-221..
- Ebraheim N, Lu J, Yang H, Mekhail AO, Yeasting RA (1997) Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot Ankle Int 18(11): 693-698.
- Naqvi GA, Cunningham P, Lynch B, et al. (2012) Fixation of Ankle Syndesmotic Injuries. Am J Sports Med 40(12): 2828-35.
- Marmor M, Hansen E, Han HK, Buckley J, Matityahu A (2011) Limitations of Standard Fluoroscopy in Detecting Rotational Malreduction of the Syndesmosis in an Ankle Fracture Model. Foot Ankle Int 32(6): 616-622.
- Van den Bekerom MPJ, Hogervorst M, Bolhuis HW, van Dijk CN (2008) Operative aspects of the syndesmotic screw: Review of current concepts. Injury 39(4): 491-498.
- Wikerøy AK, Høiness PR, Andreassen GS, Hellund JC, Madsen JE (2010) No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fracture. J Orthop Trauma 24(1): 17-23
- Lindsjo U (1981) Operative treatment of ankle fractures. Acta Orthop Scand Suppl 189: 1-131.
- Peterson KS, Chapman WD, Hyer CF, Berlet GC (2015) Maintenance of reduction with suture buttonn fixation devices for ankle syndesmosis repair. Foot Ankle Int 36(6): 679-84.
- Thornes B, Shannon F, Guiney A, Hession P, Masterson E (2005) Suture-button syndesmosis fixation: accelerated rehabilitation and improved outcomes. Clin Orthop Relat Res 431: 207-212.
- Bava E, Charlton T, Thordarson D (2010) Ankle fracture syndesmosis fixation and management: the current practice of orthopedic surgeons. An J Orthop 39(5): 242-246.






























