Camptodactyly Arthropathy Coxa Vara Pericarditis Syndrome: A Report of Two Cases in Syria
Haya Swilem1*, Mhd Kutaiba Albuni1, Nour Seilin1, Noor Badin1 and Mohammed Al Lababidy1 and Basheer Khalil2<
1Faculty of Medicine, Damascus University, Syria
2Division of Rheumatology, Department of Pediatrics, Damascus University, Syria
Submission: June 17, 2019;Published: July 24, 2019
*Corresponding author: Haya Swilem, Faculty of Medicine, Damascus University, Damascus, Syria, Mazzeh Street, Damascus, Syria
How to cite this article: Haya S, Mhd Kutaiba A, Nour S, Noor B, Md A Lababidy, et al. Camptodactyly Arthropathy Coxa Vara Pericarditis Syndrome: A Report of Two Cases in Syria. JOJ Orthoped Ortho Surg. 2018; 2(2): 555585. DOI: 10.19080/JOJOOS.2019.02.555585
Abstract
Camptodactyly-arthropathy-coxa vara-pericarditis Syndrome (CACP) is a rare condition presents with camptodactyly, non-inflammatory arthropathy, progressive coxa vara and occasionally non inflammatory pericarditis. CACP syndrome can be diagnosed at birth or during early childhood. At first, CACP syndrome may be confused with juvenile idiopathic arthritis (JIA) because both diseases have similar symptoms. The treatment options for both diseases are different which makes the distinction between the two of high importance. We present a case two cases of CACP syndrome in two female sibling’s sisters with healthy consanguineous parents that has have distinctive radiological and histological evidence of this rare condition. The younger one presented with camptodactyly, flexion contracture of the fingers with restricted motions, swollen joints and gait disturbance. By return to her medical family history we found that her older sister has suffered from similar symptoms. The older girl was mistakenly diagnosed with JIA and put on methotrexate and corticosteroids without any improvement. Therefore, we reevaluated her condition and suspected of CACP syndrome for the two girls. And that reflect the importance of the awareness of CACP syndrome as a possible differential diagnosis of JIA in all patients who present with non-inflammatory arthropathy to avoid unnecessary and severe side effects of JIA treatment. treatments and their side effects.
Introduction
CACP syndrome is a rare autosomal recessive disorder. It has a set of clinically variable features that include fixed flexion deformity of the interphalangeal joints (camptodactyly), non-inflammatory arthropathy, deformity of the hips (coxa vara) with or without non-inflammatory pericarditis and pericardial effusion. Other characteristic features may include nuclear cataract in both eyes and protein-losing enteropathy resulting from constrictive pericarditis [1-2]. CACP syndrome was first described in 1986 [3].
Despite its rarity, many cases from different ethnic populations especially in the Middle East and North Africa have been reported [3-5]. The pathophysiology of CACP syndrome is not completely understood. CACP patients suffer from loss of function mutation in PRG4 gene which is located on chromosome band 1q25-31 [4]. This gene is responsible for lubricin production (a surface mucinous glycoprotein that contributes to the lubrication of synovial joints, protects cartilage surfaces and inhibits synovial cell overgrowth) [6]. CACP symptoms overlap with Juvenile Idiopathic Arthritis (JIA) as the two disorders have similar clinical and radiological manifestations. The treatment options for JIA include NSAIDs, DMARDs, biologic modifiers and corticosteroids. CACP patients do not respond to these therapies but rather they managed symptomatically with physical therapy. Surgical intervention may be recommended if severe, refractory symptoms have developed [7]. This report shows the importance of clinical, laboratory and radiological findings of CACP syndrome in two female siblings that can help in early diagnosis of CACP syndrome and allow differentiation from other inflammatory diseases to not manage those patients with unnecessary treatments.
Case Report
Patient 1
A 5-year-old girl with healthy consanguineous parents presented to Children’s Hospital of Damascus University with camptodactyly of both hands. This flexion contracture was noticed by her parents since her first year. She suffered from swollen joints and gait disturbance that got worse in the recent seven months. Physical examination showed camptodactyly deformity of the 2nd, 3rd, 4th and 5th fingers at the proximal interphalangeal (PIP) joints of both hands (Figure 1) and swollen knees and ankles without other signs of inflammation like tenderness or erythema (Figure 2). Flexion and extension of both ankles were limited. In addition, hip abduction was restricted. Eyes examination was unremarkable and vital signs were within normal limits. Laboratory findings of CBC, CRPand ESR were in normal ranges. Liver and renal function assays were unremarkable. Immunologic studies were normal for ANA immunofluorescence, anti dsDNA and RF. IgG (12.2 g/l), IgA (1.4 g/l), IgM (1.1 g/l) all were within normal ranges. There was no clinical evidence for pericarditis.


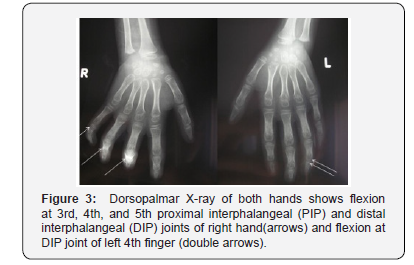
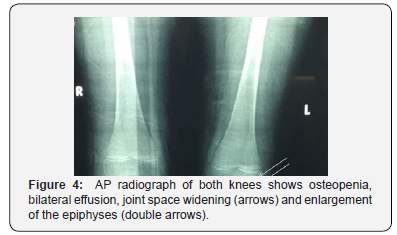
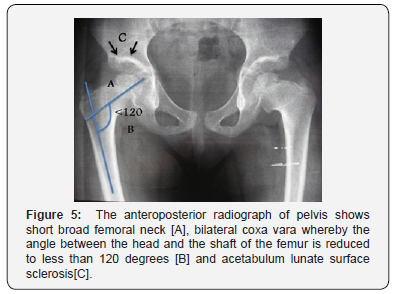
Cardiac ultrasound showed no abnormalities or effusion. Plain X-ray of both hands showed flexion at 3rd, 4th and 5th proximal interphalangeal joints (PIP) and distal interphalangeal joints (DIP) of right hand and flexion at DIP joint of the left 4th finger (Figure 3). Knees X-ray showed osteopenia, bilateral effusion, swelling of soft tissues, joint space widening, and epiphyseal widening of both knees (Figure 4). Pelvis X-ray showed short broad femoral neck, bilateral coxa vara and acetabulum lunate surface sclerosis (Figure 5). Knee ultrasound revealed large bilateral joint effusions.
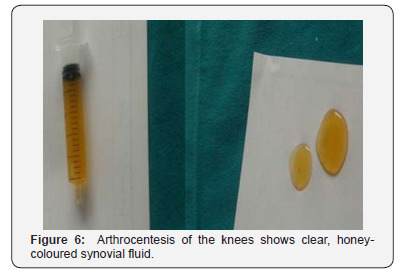
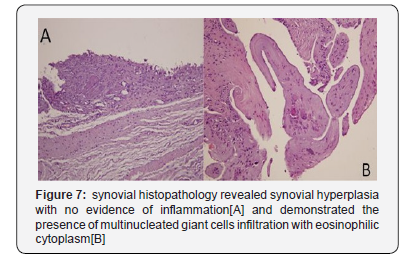
Arthrocentesis of the knees showed clear honey-coloured synovial fluid that consisted of 4 white blood cells and 20g/ dl of albumin (Figure 6). Synovial histopathology revealed synovial hyperplasia and the presence of multinucleated giant cells infiltration with eosinophilic cytoplasm (Figure 7). After the diagnosis of CACP syndrome was confirmed, the patient was discharged along with physiotherapy. Surgical procedures were suggested if severe and refractory symptoms were observed. Developed.
Patient 2
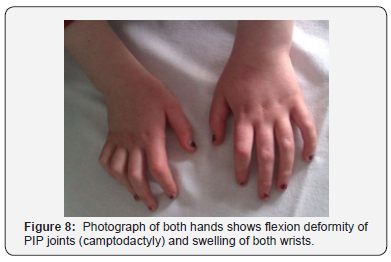
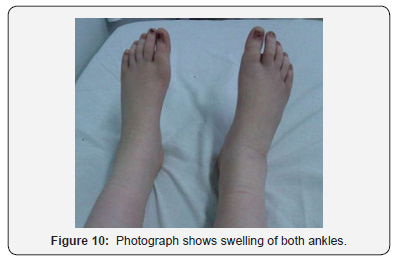
An 11-year-old girl (the older sister of patient 1) presented to Children’s Hospital of Damascus University with swollen joints, morning stiffness and lower back pain that is better not relieved with rest and worse with activity. Since the age of two, her parents have noticed bilateral knee swelling without redness or fever followed by progressively walking difficulties with waddling gait. During the next three years, swelling in small joints of hands, wrists, feet and ankles have developed. There was no fever, loss of appetite, weight loss or night sweating. She was mistakenly diagnosed with Juvenile Idiopathic Arthritis (JIA) at an outside clinic and was put on steroids. She had several side effects from the treatment with no improvement in her symptoms. At the age of 11 years and after we diagnosed her little sister to have CACP syndrome, the girl (patient 2) came to our hospital for reevaluation. On examination, she had camptodactyly at the2nd, 3rd, 4th and 5th proximal interphalangeal (PIP) joints of both hands (Figure 8). Swollen wrists, knees and ankles without inflammatory signs were present (Figures 8-10). There were also some limitation in extension and flexion of wrists joints and limitation in abduction and internal rotation of hip joints. Knees examination showed valgus deformity without limited motions. Schober test was normal.

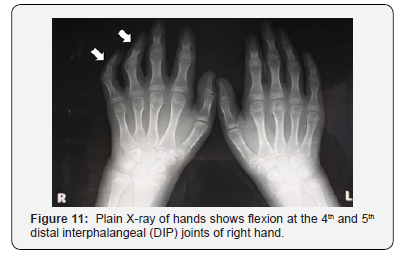
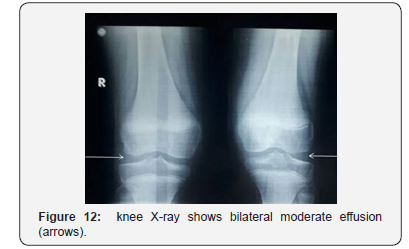
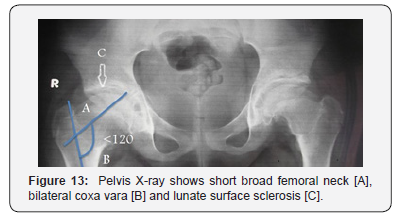
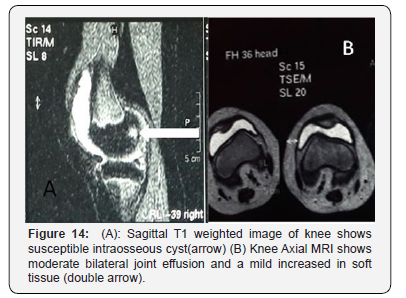
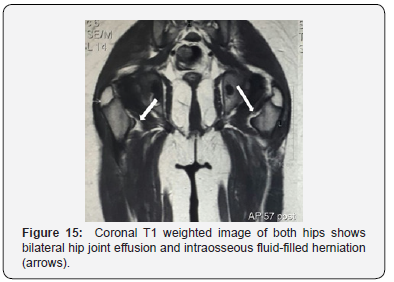
Laboratory tests revealed normal ranges of CBC, ESR, CRP, Albumin, Creatinine, Urea, electrolytes. Anti-CCP, RF, ANAwere all negative. Cardiac ultrasound showed no effusion. Knee ultrasound showed bilateral moderate effusion. Plain radiograph of both hands showed flexion at the 4th and 5th distal interphalangeal (DIP) joints of the right hand (Figure 11). Knees X-ray (Figure 12) and pelvis anterior-posterior radiograph (Figure 13) showed similar findings to her younger sister. Knees MRI revealed a mild increased in soft tissue, moderate bilateral joint effusion and intraosseous filled-fluid herniation (Figure 14). Hip MRI showed moderate effusion and susceptible intraosseous cysts without erosions (Figure 15). She was discharged along with acetaminophen (15 mg/k) with the possibility of surgery if severe symptoms have developed..
Discussion
CACP is a rare disease characterized by a combination of multiple clinical symptoms that usually begin at birth or in thefirst months of life [8]. The name of the disease comes from the main symptoms (camptodactyly), which is derived from the ancient Greek words kamptos (bent) and daktylos (finger), noninflammatory joint disease (arthropathy), deformity of the hip whereby the angle between the head and the shaft of the femur is reduced to less than 120 degrees (coxa vara) and in 20-30% of cases it may include an abnormal accumulation of fluid in the pericardial cavity (pericardial effusion) or lungs (pleural effusion) [8].
CACP syndrome is an autosomal recessive disease caused by mutations in proteoglycan 4 gene which encodes for a glycoprotein called lubricin that protects the cartilages from damage by erosions [9]. Diagnosis is based on clinical findings, synovial fluid aspiration and a synovial biopsy [9], in addition to genetic testing which can confirm the diagnosis [10]. This report focuses on two sisters with CACP syndrome who were born to healthy consanguineous parents. The parents have six children; two girls were born with CACP syndrome, and four healthy boys, in addition to three non-consecutive abortions. The latter suggests that the parents are highly suspected to be carriers of other genetic diseases.
Clinical manifestations varied between the two siblings as patient 2 was first admitted with bilateral knee joints swellingthat later progressed to involve other joints such as wrists and ankles. The wrist is usually the first joint to be affected and is the most common influenced joint [8-11]. Patient 1 was first presented with Camptodactyly, swelling of knees and ankles joints, and difficulty in walking that developed later. She denied the presence of pain. Per contra, her older sister, patient 2, complained from a low back pain that was attributed to coxavara. A study of 12 cases with CACP showed that the presence of pain was limited to only 4/12 [8] which supports the presence of pain is usually a late or rare symptom. There was no evidence of pericardial effusion and echocardiogram revealed normal myocardial function.
Knee ultrasound revealed a slight amount of noninflammatory fluid in patient 1, while a large amount of effusion showed in the knee of the younger sister, patient 2, and this would show the difference in the progress of symptoms. our patients have at least a swollen joint with non-erosive arthropathy. The noninflammatory course of the disease was evident by normal inflammatory markers. The mutations in proteoglycan 4 gene may manifest as calcification of structures adjacent to the ankle, an increase in space between the patella and femur and osteopenia of the patella and the head of the humerus.
Radiological appearances confirm the diagnosis of CACP. Knees X-ray showed osteopenia, bilateral effusion, swelling of soft tissues, joint space widening, and epiphyseal widening of both knees. Knee MRI image of the older sister, patient 2, showed intraosseous cysts inside the bone, without bone erosion [12].
The synovial fluid analysis revealed the absence of inflammatory features which is an additional clue to the noninflammatory nature of the syndrome. Typically, the synovial histopathology biopsy shows diffuse hyperplasia of the synovial membrane as well as multi-nucleotide giant cells and eosinophilic deposits without signs of inflammation [13]. Camptodactyly is a common symptom in CAPC but might a part of other diseases such as Blau syndrome, SLE, and juvenile idiopathic arthritis, which makes the diagnosis very challenging especially in the sitting of absent genetic testing.
JIA is a diagnosis of exclusion that is based on clinical features and radiographic findings of the disease which have some similarities with CACP syndrome. CACP syndrome and JIA share many features, both diseases can present early in life (around 3.5 years), and both commonly present with camptodactyly and arthropathy that involves large joints. Despite the inflammatory nature of JIA, there are some cases can present with late onset of fever that can’t be detected at the time of admission and mild elevation in inflammatory markers that can be easily confused with a co-occurring bacterial or viral incident. The older girl was first diagnosed with juvenile idiopathic arthritis and put on methotrexate and corticosteroids treatment without any improvement, This unnecessary treatment had led to many side effects that stopped after the cessation of the treatment,therefore understanding the existence and structure of this disease are really substantial [14].
Conclusion
Consanguinity and early onset camptodactyly provide important clues for the right diagnosis but poor genetic analysis abilities (where) make the definite diagnosis of CACP an absolute challenge. These are the first two cases of CACP that presented to Children’s Hospital of Damascus University in Syria, which makes it important to raise the awareness of CACP syndrome as a possible differential diagnosis of JIA in all patients who present with non-inflammatory arthropathy to avoid unnecessary and severe side effects of JIA treatment.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- NA Akawi, BR Ali, Lal Gazali (2012) A novel mutation in PRG4 gene underlying camptodactyly-arthropathy-coxa vara-pericarditis syndrome with the possible expansion of the phenotype to include congenital Birth Defects Res A Clin Mol Teratol 94(7): 553-556.
- B Peters, JHM Schuurs-Hoeijmakers, J Fuijkschot (2016) Protein-losing enteropathy in camptodactyly-arthropathy-coxavara-pericarditis (CACP) syndrome. Pediatric Rheumatology 14(1): 32.
- RM Laxer, BJ Cameron, D Chaisson (1986) The camptodactyly-arthropathy-pericarditis Syndrome: case report and literature review 29(3): 439-444.
- SA Bahabri, WM Suwairi, RM Laxer (1998) The camptodactyly-arthropathy-coxa vara-pericarditis syndrome: clinical features and genetic mapping to human chromosome 1. Arthritis and Rheumatology 41(4): 730-735.
- Albuhairan SM, Al-Mayouf (2013) Camptodactyly-arthropathy-coxa vara-pericarditis syndrome in Saudi Arabia: clinical and molecular genetic findings in 22 patients. Semin Arthritis Rheum 43(2): 292-296.
- GD Jay, JR Torres, ML Warman (2007) The role of lubricin in the mechanical behavior of synovial fluid, Proc. Nat Acad Sci 104(15): 6194–6199.
- M Taşar, Z Eyileten, F Kasımzade (2014) Camptodactyly-arthropathy-coxa vara-pericarditis (CACP) syndrome. Turk J Pediatr 56(6)): 684-686.
- Faivre L, Prieur AM, Le Merrer M (2000) Clinical variability and genetic homogeneity of the camptodactyly-arthropathy-coxa vara-pericarditis syndrome. Am J Med Genet 95(3): 233-236.
- Kakkar RM, Soneji S, Badhe RR (2013) Camptodactyly-arthropathy-coxa vara-pericarditis syndrome: important differential for juvenile idiopathic arthritis. J Clin Imaging 3(24).
- Ciullini Mannurita S, Vignoli M, Bianchi L (2014) CACP syndrome: identification of five novel mutations and of the first case of UPD in the largest European cohort. Eur J Hum Genet 22(2): 197-201.
- Albtoush OM, Taib AA, Manzalawi KA (2017) Camptodactyly-Arthropathy-Coxa Vara-Pericarditis Syndrome with Shoulder Joint Involvement: A Case Report with Literature Review. RöFo 190(9): 856-858.
- R Vutukuru, KK M Reddy (2016) Pathognomonic acetabular cysts in camptodactyly-arthropathy-coxa vara-pericarditis (CACP) syndrome. Indian J Med Res 143(6): 834.
- Marcelino J, Carpten JD, Suwairi WM (1999) CACP, encoding a secreted proteoglycan, is mutated in camptodactyly-arthropathy-coxa vara-pericarditis syndrome. Nat Genet 23(3): 319-322.
- Offiah AC, Woo P, Prieur AM (2005) Camptodactyly-arthropathy-coxavara-pericarditis syndrome versus juvenile idiopathic arthropathy. AJR Am J Roentgenol 185(2): 522-529.






























