Cervical Spondylotic Radiculopathy: Early Result from a Conservative Therapy
Zamzuri Z* and Lei Peng S
Department of Orthopaedics, International Islamic University Malaysia, Malaysia
Submission: November 27, 2018;Published: May 23, 2019
*Corresponding author: Zamzuri Zakaria, Department of Orthopaedics, Traumatology & Rehabilitation, Kulliyyah of Medicine, International Islamic University Malaysia, Jalan Hospital Campus, Kuantan, Pahang, Malaysia
How to cite this article: Charles APT, Md Shukrimi A, ED SIMOR K, Satriya SHA, Faun HY. Is Conservative Approach a Better Option for Primary Treatment of Closed Tibia Fractures in Albers- Schonberg Disease? a Case Report. JOJ Orthoped Ortho Surg. 2018; 2(2): 555583. DOI: 10.19080/JOJOOS.2019.02.555583
Abstract
Introduction: Patients who had cervical spondylotic radiculopathy without major motor deficit and no evidence of cord compression will have good outcome with non-operative measures. The aim of this study was to determine the severity of degenerative changes on plain radiograph among the patients with cervical spondylotic radiculopathy, their rated outcomes following conservative treatment and to evaluate correlations between pain score with: 1) neck disability index, 2) severity of degenerative changes of the cervical spine and 3) different level of root compression.
Methods: This is an observational cohort study recruiting all patients with a clinical diagnosis of cervical spondylotic radiculopathy treated conservatively between December 2016 and January 2018. One-way ANOVA, paired sample test, and Pearson’s correlation test were used for correlation analyses. The total of 29 patients was used to achieve the power of 80% at 0.05 significance level, in detecting a difference of five score from a mean of 28.6 with an estimated standard deviation of 9.2, using a two-sided one-sample t-test.
Results: Neck disability index (NDI) and pain score showed significant correlation after conservative treatment (p<0.001). However, this was not observed between pain score and radiographic severity grade, or between pain score and different level of nerve root compression.
Conclusion: Patients with cervical spondylotic radiculopathy treated conservatively showed favorable clinical outcomes.
Keywords: Cervical spine Conservative treatment Degenerative spine Radiculopathy.
Introduction
Cervical spondylotic radiculopathy is a common cause of neck pain and disability, especially in elderly mainly due to wear and tear of the cervical spine, referred as arthritis or spondylosis. In younger patient, cervical radiculopathy occurs mainly due to herniated nucleus polposus. Cervical spondylotic radiculopathy is define as a clinical condition when the nerve in the degenerative cervical spine is compressed or irritated where it branches away from the spinal cord, usually with varying degrees of sensory, motor and reflex changes as well as dysesthesias and paresthesia’s related to nerve root(s) without evidence of spinal cord dysfunction (myelopathy) [1]. Clinically the signs elicited from patients differ depending on the level of compression. Patient usually presented with unilateral limb radiating pain which associated with numbness or weakness. However, absence of radiating pain unable to exclude nerve root compression. Patient’s history and clinical examination are essential to diagnose cervical spondylotic radiculopathy.
Conservative management for the cervical spondylotic radiculopathy reported good to excellent outcomes in up to 90% of patients [2]. The treatment included oral analgesics, cervical traction, neck immobilization, physiotherapy, behavior modification and various combinations of those. Surgical treatments are reserve to those who failed conservative treatment. The objective of the study is to evaluate the clinical outcomes of patient who were treated conservatively in Hospital Kuala Lumpur and Hospital Tengku Ampuan Afzan by using a Neck Disability Index (NDI).
Materials and Methods
This cross-sectional study was performed by reviewing patients and medical records of patients whom had been presented with symptoms and signs of cervical spondylotic radiculopathy at Hospital Kuala Lumpur and Hospital Tengku Ampuan Afzan Kuantan from 1st December 2016 until 31st January 2018. Inclusion criteria were; (1) patients aged 30 to 70 years old with clinical findings of cervical spondylotic radiculopathy, (2) had underwent cervical plain radiograph and treated conservatively, and (3) attended regular follow ups for at least complete three months. Patients who had congenital stenosis of cervical spine, rheumatoid arthritis, history of cervical spine fracture, infection or malignancy, or previous cervical spine surgery were excluded. The initial pain score, range of neck movement, neurological status, and details of theradiculopathy were recorded. The Atlas of Standard Radiograph of Arthritis (1963) grading was used to grade the severity of the degeneration of the cervical spine;
a. grade 1: slight anterior wear of vertebral lip
a. grade 1: slight anterior wear of vertebral lip
b. grade 2: anterior osteophytes
c. grade 3: anterior osteophytes and narrowing of disc
d. grade 4: anterior osteophytes, disc narrowing and sclerosis of vertebral plates.
The clinical outcomes were evaluated using an NDI Questionnaire. The questionnaire consists of 10 item of patient’s self-reported neck pain related disability. These include degree of pain, personal care, lifting, reading, headaches, concentration, work, driving, sleeping, and recreation. Each of the 10 items was scored 0 to 5 with a maximum total score of 50. The total score will be categorized into no disability (score 0 to 4), mild disability (score 5 to 14), moderate disability (score 15 to 24), severe disability (score 25 to 34) and complete disability (score of above 34). The total core was also converted to a percentage score by multiplying it by two. The NDI scores were documented on the first meeting and three months after conservative treatment. All the patients were treated with analgesics, and anticonvulsants such as pregabalin were added if there was presence of any neuropathic symptoms. The physical therapy for neck exercise was done at the rehabilitation unit following a standard treatment protocol. Statistical analyses performed using SPSS software version 20. Parametric data was analyzed using descriptive analyses (means and standard deviations), and independent t-test. Correlation test was performed with paired sample test, ANOVA, and Pearson correlation coefficient. Statistically significant was taken at p <0.05.
Results
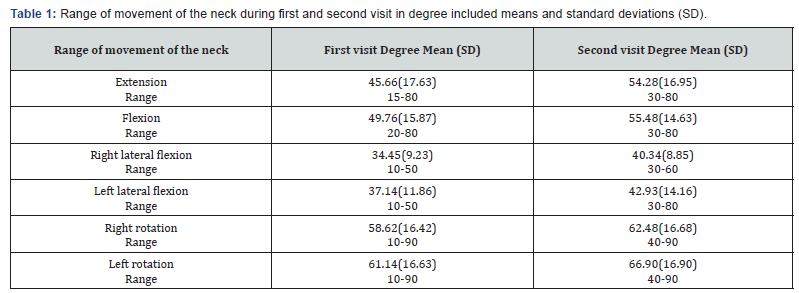
There was a total of 29 patients who received conservative treatment. These include 20 females and 9 males with age ranging from 33 to 69 years. The number of patients recruited was adequate to achieve the power of 80%, at 0.05 significance level. The pain score during the first visit was in range of 2 to 10 and improved after three months of conservative treatment to a range of 0 to 6. The range of the neck movement also showed improvement after three months of conservative management (Table 1). Majority of patients (41%) had grade 2 degenerative changes with only one patient out of the entire cohort of patients had grade 4 degenerative changes on plain radiograph. The mean pain score for first assessment was 5.34±2.0 and 3.24±1.5 after three months.
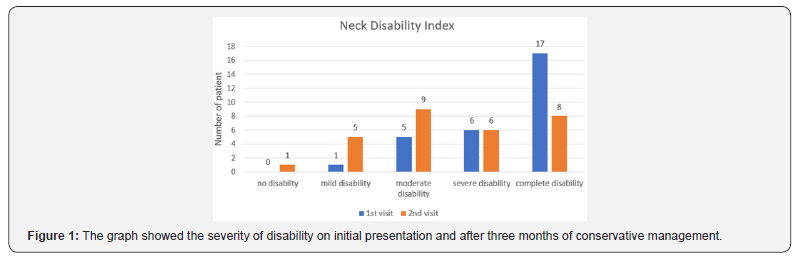
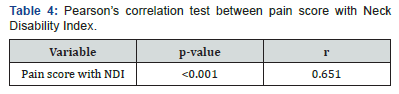
The number of patients with no disability and mild to moderate increased at 3 months, for severe disability the number did not change at 3 months follow up. However, the number of patients for complete disability was reduce from 17 to 8 patients after 3 months of follow up (Figure 1). Neck disability index mean on first assessment was 41.45±15.1 and 26.52±18.4 after three months. The results showed significant correlation between pain and neck disability index after three months of conservative treatment (p< 0.001) (Table 2).
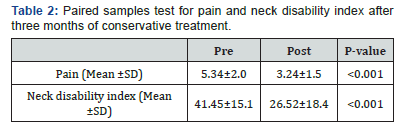
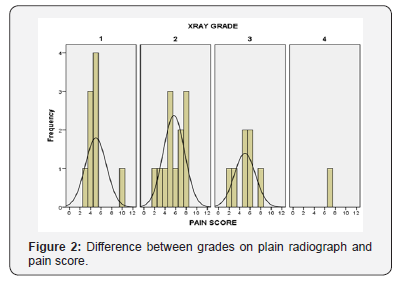
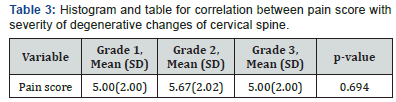
The associations between pain and severity of degenerative changes of cervical spine were evaluated based on histogram normally distribute. One-way ANOVA was used to compare mean different between grades on plain radiograph and pain score (Figure 2). The results showed there was no significant association between grade on plain radiograph and pain score (p-value = 0.694) (Table 3). On the other hand, significant positive correlation (r=0.651) between pain score and NDI was observed based on Pearson correlation (p-value <0.001) (Table 4). The independent sample t-test was conducted to evaluate the correlation between pain score and the different levels of nerve root compression. Results obtained showed no significant correlation.
Discussion
The annual incidence of cervical radiculopathy (CR) has been reported by Radhakrishnan et al. [3] to be 83 cases per 100,000 people, about 107.3 per 100,000 for men and 63.5 per 100,000 for women, with an increased prevalence noted in the fifth decade of life. They are experiencing an acute episode of unilateral radiculopathy without major motor deficit, no evidence of disease progression to cord compression if absent at the initial presentation. A variety of conditions can lead to nerve root compression in the cervical spine. The exiting nerve root can be compressed by soft disk herniation or through encroachment by surrounding degenerative or hypertrophic bony elements [4]. In either case, a combination of factors, such as inflammatory mediators (e.g., substance P), changes in vascular response and intraneural edema contribute to the development of radicular pain. Patients with chronic neck pain associated with spondylosis is typically bilateral, whereas neck pain associated with radiculopathy is more often unilateral. Pain radiation varies depending on the involved nerve root, although some distributional overlap may exist. Absence of radiating extremity pain does not preclude nerve root compression. At times, pain may be isolated to the shoulder girdle. Similarly, sensory or motor dysfunction may be present without significant pain. Symptoms are often exacerbated by extension and rotation of the neck (Spurling sign), which decreases the size of the neural foramen. The classic patterns of cervical radiculopathy based on the affected nerve root.
There were 29 patients, 19 Malays, 6 Chinese and 4 Indians were participated in this study. The age of the patients was ranging from 33 to 69 years old with mean age of 49 years old. Predominantly there were more female patients, 69% (20 patients) as compared to male patients, 31% (9 patients). In the study by Tanaka et al. [5], 300 patients with cervical radiculopathy who visited them between 1989 and 1996, 66% were in their 40s and 50s. Their mean age at the first visit was 51 years. The sex ratio of the patients reported in different studies is highly variable but in our study the radiculopathy was more common in women as well as in the study by Tanaka et al [5]. There was no scientific data why women were prone to have cervical radiculopathy and we postulated that in our community women were more concern about the pathology compared to men. All patients presented with a radiographic picture of cervical spondylosis. The severity of degenerative changes on plain radiograph among patients revealed majority in Grade 2 which was 41% (n=12) and minority in Grade 4 which was only 3.4% (n=1). MRI of the cervical spine was done only in patient with a significant radicular pain and neurological deficit. In this study the diagnosis of cervical spondylotic radiculopathy was made mainly on the clinical ground based on the history and physical examination.
The mean neck disability index was improved after 3 months of treatment. The paired samples test for pain andneck disability index after 3 months of conservative treatment showed significant correlation with a p <0.001 and similar result was observed on the Pearson correlation test. However clinically only the group of complete disability showed a significant improvement in the number of patients compare to the other group. It is very difficult to conclude the that the patient was improved with a conservative management in view of the small number of our patient and a short duration of follow up which was only three months. We were aware of the weakness of our study. In the classic study by Lees and Turner [6] with a longterm follow-up (2-19 years) of 51 patients with radiculopathy, 45% had only a single episode of pain without recurrence, 30% had mild symptoms, and only 25% had persistent or worsening symptoms. No radiculopathy patient progressed to myelopathy in this series. In the other study patients were treated within 2 months after the onset, symptoms were improved generally marked until 4 months after treatment but was less so thereafter [5].
There was no statistically significant between pains with the severity of degenerative changes on plain radiograph in this study. This combination does not necessarily indicate a causeeffect relationship between degenerative and patient with cervical radiculopathy. Braakman et al. [7] stated that there was a poor correlation between the amount of spondylotic change seen on the radiographs and the degree of neurological deficit. The results of this study agree with previous studies that the severity of cervical degeneration is not correlated with the degree of pain perceived [8-10]. Gore et al. [11] completed an investigation in 205 patients previously seen for a neck complaint. A follow up radiographic examination was conducted after a minimum of ten years to assess for subsequent spinal degeneration. The results concluded no significant relationship between the degree of spinal degeneration and patient symptoms at either initial presentation or at follow up.
Radiculopathy caused by degenerative disease most often affects the cervical root segments 5 to 8. Epidemiologic studies have shown that the C7 root (C6-7 herniation) was the most commonly affected, followed by the C6 (C5-6 herniation) and C8 (C7-T1 herniation) nerve roots. In our study, clinically C6 nerve root was the most affected nerve root among the patients, follows by C7, C5 and C8. However, there was no correlation between pain with different level of nerve root compression. Thedistribution of the cervical nerves was segmental in character and there was a definite overlap of the nerve supply to adjacent segments in any given skin area. Irritation of a nerve root may cause pain and paresthesia anywhere along the segmental distribution of the nerve. Furthermore, the reflex phenomenon of pain, causes painful irritation along the segmental distribution of the nerve or nerves which supply that muscle. The segmental distribution of the cervical nerve roots, their sensory overlap and the reflex phenomenon of pain make the exact localization of nerve root irritation somewhat difficult. While, the pain itself was very subjective and had its own experienced individually.
Conclusion
Cervical radiculopathy is a prominent symptom of degenerative cervical disease. The neck pain experienced by patient does not correlate with the severity of the degenerative changes of the cervical spine.
References
- Korinth MC (2008) Treatment Evolution in Management of Cervical Disc Disease - current status and trends. Zentralbl Neurochir 69(3): 113-124.
- Caridi JM, Pumberger M, Hughes AP (2011) Cervical Radiculopathy: A Review. HSS Journal 7(3): 265-272.
- Radhakrishnan K, Litchy WJ, O Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 117(Pt2): 325-335.
- McCormack BM, Weinstein PR (1996) Cervical spondylosis-An update. West J Med 165: 43-51.
- Tanaka Y, Kokubun S, Sato T (1998) Cervical radiculopathy and its unsolved problems. Current Orthopedics 12: 1-6.
- Lees F, Turner JWA (1963) Natural history and prognosis of cervical spondylosis. British Medical Journal 2(5373): 1607-1610.
- Braakman R (1994) Management of cervical spondylotic myelopathy and radiculopathy. J Neurol Neurosurg Psychiatry 57: 257-263.
- Bovim G, Schrader H, Sand T (1994) Neck pain in the general population. Spine 19(12): 1307-1309.
- Laplante BL, DePalma MJ (2012) Spine osteoarthritis. Am Acad Physical Medicine and Rehabilitation. 4(5): S28-36.
- French SD, Walker BF, Cameron M, et al (2003) Risk management for chiropractors and osteopaths: imaging guidelines for conditions commonly seen in practice. Aust Chir Osteo 11(2): 41-48.
- Gore DR, Sepie SB, Gardner GM, Murray PM (1987) Neck pain: a long-term follow up of 205 patients. Spine (Phila Pa 1976) 12(1): 1-5.






























