Is Conservative Approach a Better Option for Primary Treatment of Closed Tibia Fractures in Albers- Schonberg Disease? a Case Report
Charles Ang Poh Thean1*, Mohd Shukrimi Awang2, ED SIMOR KHAN3, Satriya Sabir Husin Athar4 and Faun Hao Yan5
1Medical officer, International Islamic University, Malaysia
2Department of Orthopaedic, International Islamic University, Malaysia
3Orthopaedic Surgeon, International Islamic University Malaysia (IIUM)
4Orthopaedic surgeon, International Islamic University Malaysia
5House officer, Hospital Selayang, Malaysia
Submission: November 27, 2018;Published: January 18, 2019
*Corresponding author: Charles Ang Poh Thean, Medical officer, International Islamic University, Malaysia
How to cite this article: Charles APT, Md Shukrimi A, ED SIMOR K, Satriya SHA, Faun HY. Is Conservative Approach a Better Option for Primary Treatment of Closed Tibia Fractures in Albers- Schonberg Disease? a Case Report. JOJ Orthoped Ortho Surg. 2018; 2(2): 555583. DOI: 10.19080/JOJOOS.2019.02.555583
Abstract
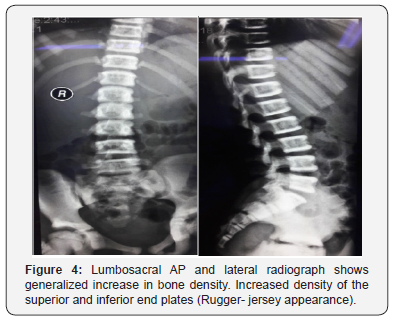
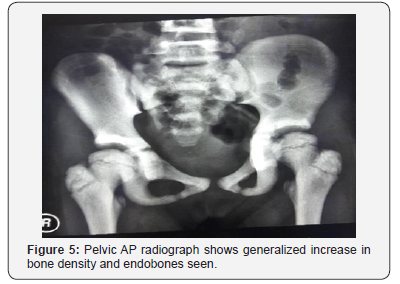
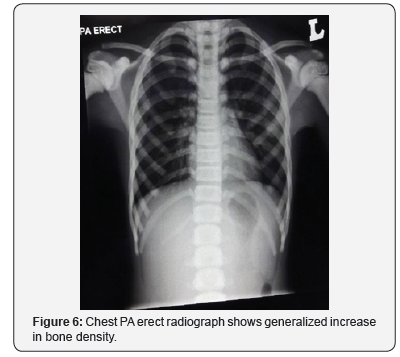
Albers- Schonberg disease is an extremely rare genetically inherited disorder. Also known as Autosomal dominant Type II osteopetrosis, it is usually diagnosed incidentally. Due to the rarity of the disease, the condition is often missed and under- diagnosed. This is a case report of an eight- year old Malay girl that was diagnosed retrospectively after developing complications to the initial treatment given. Due to the underlying undiagnosed osteopetrosis rendering her prone for infections, a simple minimally invasive percutaneous K-wiring of her left tibia for a closed fracture was complicated with osteomyelitis causing significant morbidity. On retrospective review, her blood and radiographic investigations reveals low hemoglobin, raised alkaline phosphatase, rugger- jersey appearance of her spine radiograph, sclerosis over the base of skull and endo bones seen in her pelvic radiograph. She undergone wound debridement, and sequestrectomy a total of three times and was treated with intravenous antibiotics for six weeks and oral antibiotics for another six weeks. Despite the adequacy of surgical and antibiotic therapy, at one year follow up she still complains of on and off left proximal tibia pain significant enough to affect her daily activity. Therefore, it is important to make known the existence of this condition and double consider if surgical intervention is really needed or conservative approach will be a better option for primary treatment.
Keywords: Albers- Schonberg disease; Autosomal dominant Type II osteopetrosis; Rugger- jersey spine; Endo bones in pelvis.
Introduction
Autosomal dominant osteopetrosis type II (ADO II) was first described by Albers- Schonberg in 1904. It is reported to be the most common form of osteopetrosis with the estimated prevalence of 5.5 in 100,000 [1]. The pathognomonic radiological findings of ADO II are “rugger- jersey spine”, endo bones in pelvis and increased sclerosis of skull base. The CICN7 mutation is said to be the cause of Albers- Schonberg disease. Pathological fractures and increased susceptibility to bone infections due to leukocyte malfunction and decreased in bone blood supply [2], are common complications associated with ADO II. Knowing this complication, should all closed tibia fractures in Albers- Schonberg disease be primarily treated via conservative method instead of surgical intervention which render them susceptible to infection?
Case presentation
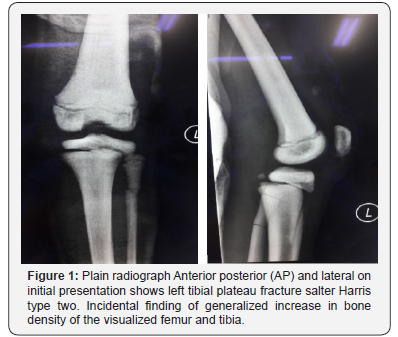
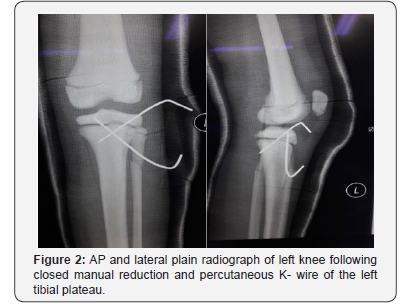
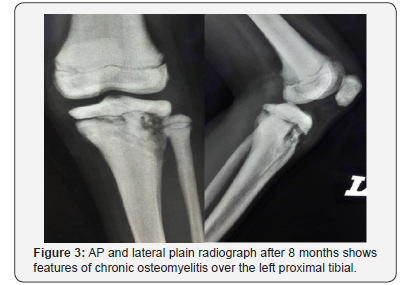
Ms A, an eight- year old girl met in a road traffic accident (motorcycle versus car). She was the pillion rider on a motorcycle rode by her sister. While making a U-turn, the front of their motorcycle was hit by a car at the speed of 30-40kmPH causing them to lose control of the motorcycle and she fell sideways landing on her left knee. There was no direct impact to her. She presented to the emergency department with complain of left knee pain, swelling and inability to weight bare. She was diagnosed with closed left tibial plateau fracture salter Harris type two and proximal third fibula fracture (Figure 1). She underwent closed reduction and percutaneous K-wiring of her left proximal tibia (Figure 2) which subsequently was complicated with osteomyelitis (Figure 3). On retrospective review of her initial plain radiograph, it was noticed to show generalized increase in bone density.
On further history taking she was born term, birth weight of 3.1kgs with no significant antepartum, delivery or postpartum history. Her growth development is consistently just below the fiftieth percentile and her growth milestones were all normal. No history of failure to thrive or recurrent infections. No historyof easy bruising. She doesn’t complain of frequent episodes of nasal stuffiness. Her vision and hearing were normal. She doesn’t experience any symptoms and signs of anemia. No history of blood transfusion or fractures (besides current presentation). She has two brothers, both of which had suffered from a fracture of their upper limb from sports injury.
On examination, her height is at the fiftieth centile. There are no abnormal facies, no cranial anomalies, no frontal bossing, no hydrocephalus, no abnormal eye moments/ nystagmus. No bruises, purpura and no pallor seen. Abdominal examination reveals no hepatosplenomegaly. Her hemoglobin was 10.5 (low), hematocrit 34, WBC 6.13 and platelets 381. Serum calcium and phosphate levels were normal, alkaline phosphatase elevated. Plain radiographs reveal rugger- jersey appearance of her spine (Figure 4), “end bones” seen within her pelvis (Figure 5) and chest radiograph shows generalized increase in bone density (Figure 6).
Due to the complication (osteomyelitis) of the initial surgery. She had to undergo wound debridement, and sequestrectomy a total of three times and treated with intravenous antibiotics for six weeks and continued with oral antibiotics for another six weeks. Total duration of admission to ward was seven weeks. She was followed up at two weeks upon discharge, the wound was healing well with healthy granulation, no discharge. She was unable to fully extend her left knee (flexion deformity of ten degrees), to which she was subjected for aggressive physiotherapy. At six weeks post discharge, the wound closed up, no more sinus or discharge and the flexion deformity improved to six degrees. She however still complains of pain over her leftproximal tibia on weight bearing and ambulation. Despite the adequacy of surgical and antibiotic therapy, at three months, six months and one year follow up she still experience pain over her left proximal tibia, significant enough to affect her daily activity (she refuses to walk, run and stand for long period). Pain is described as dull aching constant pain localized to the proximal tibia, no joint line tenderness. She also suffered permanent fixed flexion deformity of her left knee of six degrees.
Discussion
Osteopetrosis, or Marble bone disease/ Osteosclerosis is a rare inherited disorder of the bone with defective osteoclast function resulting in failure of bone resorption. As a result, bone modeling and remodeling is impaired. This in turn causes increase skeletal fragility (bone dissolve and break) despite increased bone mass (radio dense), prone to bone infections, hematopoietic insufficiency, nerve entrapment syndromes and growth impairments. Estimated prevalence of osteopetrosis is 1 in 100000 to 500000 worldwide. [3] It is classified into three groups. The Juvenile malignant, Intermediate and Autosomal dominant type I and II. The Juvenile type, if not promptly treated is usually fatal within the first few years of life. The intermediate type usually presents during the first decade of life and follows the autosomal dominant (adult) type disease course. Life expectancy of the adult type is full but associated with many orthopedic related issues [4]. It presents with a wide spectrum of clinical variants due to the heterogenicity of genetic defects [5]. Mild form may be assymptomatic. However, serious forms can cause stunted/ deformed growth, increase chances of fracture, abnormal cortical bone morphology, abnormal vertebral bodies, anaemia, recurrent infections, hepatosplenomegaly, blindness, cranial nerve paralysis and even hearing and visual impairment [6].
The Autosomal Dominant osteopetrosis (ADO)/adult type, is also known as Albers-Schonberg disease. Sufferers are usuallyasymptomatic. Some may develop scoliosis and multiple bone fractures. Based on the basis of radiographic, biochemical, and clinical features, there are two types of adult osteopetrosis. Type I is associated with low fracture risk and normal serum acid phosphate. Radiographically, the spine and pelvis are relatively normal and only the skull shows marked sclerosis mainly at the vault. Type II on the other hand is associated with high risk of fracture and very high serum acid phosphate levels. Radiographically, skull shows sclerosis mainly at the base, spine shows rugger- jersey appearance and endobones are seen in the pelvis
This case is the typical presentation of an Albers- Schonberg disease (ADO II) and is strongly associated with increase susceptibility to bone infection, therefore is conservative approach a better option for primary treatment of all closed tibia fractures in these patients? Dahl N et al. [7] states that although ADO II fractures are pathological, fracture healing with conservative treatment are not affected. Armstrong DG et al. [8] reported that out of twenty- nine cases of tibia fractures, majority were successfully treated conservatively. Bhargava A et al. [2] states that the rate of surgical complications is high as increased bone hardness generates heat during drilling causes bone necrosis and breakage of drill bit. In addition, bone brittleness can lead to intra-operative fractures. All this causes a difficult operation thereby prolonging the operative time and further increases the risk of post-operative infection. He proceeded to conclude that most long bone fractures response well to conservative treatment and surgery is only considered following failure of conservative treatment. Sen RK et al. [9] states that conservative treatment produces satisfactory results although healing rate is often prolonged, but this prolonged healing is also seen with internal fixation.
Conclusion
Learning from this case and all other cited cases, the author would like to suggest that conservative approach remains the mainstay for the treatment of closed fractures in patients suffering from Albers- Schonbery disease due to the high infection rate associated with this condition.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Bollerslev J (1987) Osteopetrosis. A genetic and epidemiological study. Clin Genet 31(2): 86-90.
- Bhargava A, Vagela M, Lennox CM (2009) Challenges in the management of fractures in osteopetrosis! Review of literature and technical tips learned from long- term management of seven patients. Injury 40(11): 1167-1171.
- Malik P, Punia H, Aggrawal A (2010) Osteopetrosis: A case report.Indian J Dent Sci2: 24-26.
- Filho AM, Domingos AC, Freitas DQ, Whaites EJ (2005) Osteopetrosis: A review and report of 2 cases. Oral Dis 11: 46-4
- Shapiro F (1993) Osteopetrosis: Current clinical considerations. Clin Orthop Relat Res 294: 34-44.
- (2017) Albers-Schonberg disease- Check Orphan.
- Dahl N, Holmgren G, Holmberg S, Ersmark H (1992) Fracture patterns in malignant osteopetrosis (Albers-Schonberg disease). Arch Orthop Trauma Surg 111(2): 121-123.
- Armstrong DG, Newfield JT, Gillespie R (1999) Orthopedic management of osteopetrosis: results of a survey and review of the literature. J Pediatr Orthop 19(1): 122-132.
- Sen RK, Gopinathan NR, Kumar R, Saini UC (2013) Simple reproducible technique in treatment for osteoporotic fractures. Musculoskelet Surg 97(2): 117-121.






























