Cauda Equina Syndrome Post Epidural Steroid Injection
Charles Ang Poh Thean1*, Zamzuri Bin Zakaria Mohamad2, Rajandra Kumar Karupiah3 and Mohd Shukrimi Awang4
1Medical officer, International Islamic University, Malaysia
2Department of Orthopaedic, International Islamic University, Malaysia
3Department of Orthopaedic, International Islamic University, Malaysia
4Department of Orthopaedic, International Islamic University, Malaysia
Submission: November 27, 2018;Published: December 13, 2018
*Corresponding author: Charles Ang Poh Thean, Medical officer, M.B.B.S, International Islamic University, Malaysia
How to cite this article: Charles A P T, Zamzuri B Z M, Rajandra K K, Md Shukrimi A. Cauda Equina Syndrome Post Epidural Steroid Injection. JOJ Orthoped Ortho Surg. 2018; 2(2): 555582. DOI: 10.19080/JOJOOS.2018.02.555582
Abstract
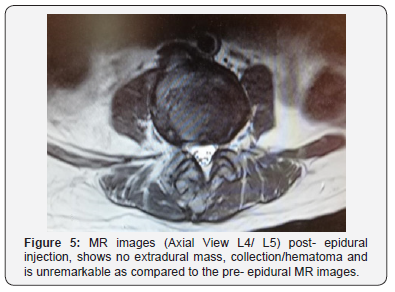
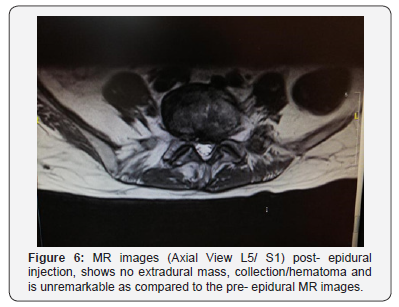
We report a case of a 62-year-old lady who developed cauda equina syndrome post- epidural steroid injection. She undergone an epidural injection to relieve her radiculopathy pain caused by underlying lumbar spinal canal stenosis L4/L5 and L5/S1. Post epidural injection she developed an acute bowel and bladder dysfunction, worsening pain and weakness over her bilateral lower limbs with saddle anesthesia which did not resolve after 6 days. Her repeated magnetic resonance imaging (MRI) post- epidural injection shows no evidence of extradural hemorrhage/collection and is unremarkable as compared to her pre- epidural magnetic resonance images. She undergone emergency laminectomy of L4/ L5 and L5/S1. Post laminectomy, her bilateral lower limb pain resolved, power restored, and she regained her bowel and bladder functions. The development of cauda equina syndrome post epidural injection have been reported as a rare complication and is commonly associated with local anesthetic toxicity, direct trauma of the needle to the spinal cord or the development epidural hematoma post injection. However, in this case there was no evidence of epidural hematoma both on magnetic resonance imaging and intraoperatively. Complete neurological recovery occurs following laminectomy suggesting the likely cause of cauda equina syndrome in this case is more to a mechanical compression.
Keywords: Lumbar spinal canal stenosis; Epidural injection; Cauda equina syndrome.
Introduction
Numerous cases have been reported on the development of cauda equina syndrome post spinal epidural injection. These reports have attributed local anesthetic neurotoxicity of both lignocaine and bupivacaine, direct trauma of spinal needle to spinal cord during penetration, compromise of blood supply to the cord and development of a spinal epidural hematoma causing mechanical compression as the cause of this complication. In this case, the patient did not have any neurological recovery even after 6 days of observation. More ever, all clinical and imaging evidence do not support any of these pathology as the causative factor prompting the surgeon to subject the patient for an emergency laminectomy.
Case presentation
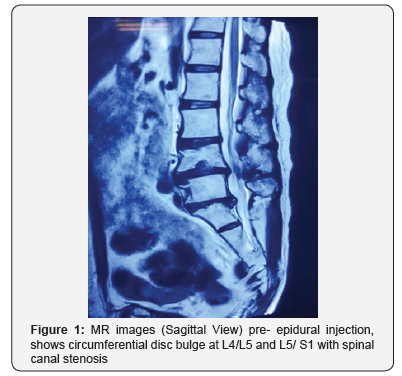
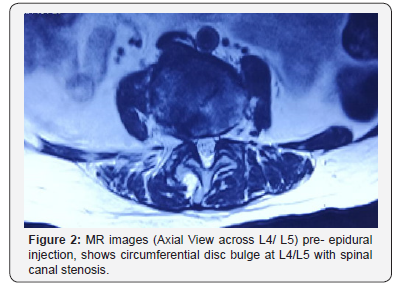
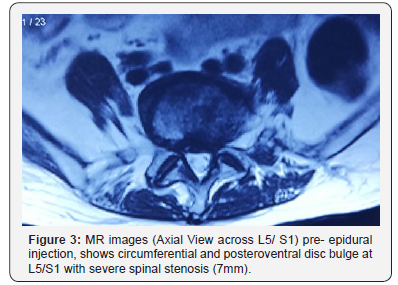
Ms M, a 62 year- old lady was diagnosed clinically with lumbar canal stenosis L4/L5 and L5/S1, she has been treated conservatively with pharmacological and physical therapy but failed. X- ray of the lumbosacral spine showed degenerative changes of the lower lumbar region. Magnetic resonance imaging (MRI) revealed worst stenosis at L5/S1 (Figure 1-3). She was subsequently scheduled for an epidural steroid injection. Prior to the epidural injection, she was able to ambulate unaided, the bowel and bladder functions were normal and clinically the neurological status of bilateral lower limbs was intact. Anepidural injection was performed at the level of L3/L4. A total of 1ml chirocaine (Levobupivacaine HCL 5.0mg) and 1ml diprospan (betamethasone dipropionate 5mg, betamethasone disodium phosphate 2mg) was given in a single attempt. No blood or cerebrospinal fluid was aspirated prior to administration of the drugs.
There was no pain or paresthesia during needle placement or drug injection. 12 hours post epidural injection she complained of worsening pain over her bilateral lower limbs, associated with weakness of her bilateral lower limbs and she was unable to pass urine. Neurological examination of the lower limbs revealed hypotonia, hypo-reflexia , reduced sensation from L4 level downwards, saddle anesthesia with the motor power of grade 2 from L4 below. There was no obvious collection/ bruising over the site of epidural injection. She was diagnosed with cauda equina syndrome as a sequela of the epidural steroid injection which was expected to resolve within the next 8hours as reported in previous case reports. Differential diagnosis at that point was the development of an epidural hematoma causing compression effect.
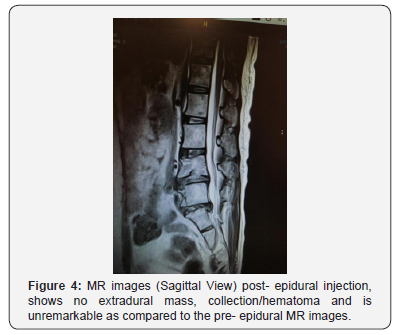
Her symptoms however continued to persist even after 24 hours to which an MRI was done to rule out epidural hematoma formation. The MRI reveals no extradural mass or hematoma collection. It was unremarkable as compared to the pre- epiduralinjection MR images (Figure 4-6). All other blood investigations and imaging was also normal. She subsequently underwent an emergency laminectomy of the L4/L5 and L5/S1 level after 6 days of observation for spontaneous neurological recovery. Intraoperative findings reveal no hematoma and upon laminectomy, the dura bulge outwards (Figure 7).
At day 4 postoperatively, she was able to ambulate unaided, peri- anal sensation was restored, anal tone returned, and bilateral lower limb reflexes was normal. There was no residual neurological deficit.

Discussion
Lumbar spinal stenosis is a lower back pathology commonly presenting with radiculopathy pain. Epidural steroid combined with analgesic injection have been practiced to help relieve lumbosacral radiculopathy pain as per in this case. However, some cases have been reported to develop complications namely cauda equina syndrome post epidural injection. Cauda equina syndrome (CES) occur due to the disruption of multiple lumbar and sacral nerve roots in the lumbar vertebral canal. Its main presenting symptoms are bladder, bowel and/ or sexual dysfunction, with sensory disturbance in the saddle area. The most common cause of CES is compression from a large central lumbar disc herniation at the L4-5 and L5-S1 levels [1].
Ayten Bilir et al. [2] reported a case of a 50-year-old lady who was given 2mls of 0.5% bupivacaine combined with 60mg of triamcinolone diacetate (total volume of 6mls). 3 hours post epidural she complained of perineal numbness, urinary retention and bilateral lower limb weakness. Neurology evaluation revealed loss of sensation over saddle area and medial aspect of her right leg. These symptoms spontaneously resolve completely over the next 8 hours. The author proceeds to conclude that this transient neurologic symptom may be caused by factors, such as accidental intrathecal injection, neurotoxicity of the agents, compromise of blood supply to the cord and loculation of the injected fluid
In 1999, a case report by C. C Loo et al. [3] reported 6 cases of cauda equina syndrome following administration of spinal analgesia with hyperbaric 5% lignocaine. 3 cases were most likely due to direct neurotoxicity. The other 3 cases were also probably due to LA neurotoxicity despite the lack of radiological evidence to exclude a mechanical compression. All these 6 patients suffered permanent neurological deficit even after an average follow up of 8 months. The author concluded that cauda equina syndrome can occur even with a single shot spinal anesthesia with 100mg or less of hyperbaric 5% lignocaine, even with the absence of maldistribution. He recommends that hyperbaric lignocaine should be given in concentrations not more than 2% at a total dose not exceeding 60mg. This report was supported by J C Gerancher [4] who reported a similar case of a 74 year old healthy man who developed cauda equina syndrome after receiving spinal analgesia of 100mg 5% lidocaine in 7.5% dextrose with 0.2ml of epinephrine for an elective inguinal hernia repair.
Kubina P et al. [5] reported 2 cases of cauda equina syndrome following spinal epidural anesthesia with bupivacaine plus glucose. The first case was given 3.6ml bupivacaine with glucose (5mg/mL) injected intrathecally. MRI later revealed spinal stenosis at L2- L3 level. The second case was given combined spinal- epidural analgesia. Spinal injection delivered 3.5ml plain bupivacaine (5mg/ mL) followed by an infusion of bupivacaine (2.5mg/ml) without glucose at 4mL/hour, which was gradually increased to 8mL/hour. Both cases developed permanent neurological deficit. The author concluded that the first case was due to the undiagnosed spinal stenosis and the second case was uncertain, citing possibility of combination of needle trauma at the time of injection, contaminants in the bupivacaine ampule, and the use of continuous bupivacaine infusion of 0.25% for more than 42hours. These 2 cases were supported by Chabbouh et al. [6] who reported another case of persistent cauda equina syndrome with no identifiable facilitating condition following an uneventful single spinal administration of 0.5% hyperbaric bupivacaine 12.5mg. He concludes that this permanent neurological deficit was due to local anesthetic toxicity adding that LA toxicity occurs mainly in the cauda equina because the sacral root sheaths are
a) Relatively longer (and larger for S1) than neighboring lumbar roots,
b) Devoid of protective sheaths, and
c) Due to their dorsal position in the thecal sac (especially L5, S1 and S2), making this area more exposed to hyperbaric anesthetic pooling.
The development of an epidural hematoma from the injection can cause local compression leading to cauda equina syndrome. Khaled M. Kebaish et al. [7] reported of such case. The development of a spinal epidural hematoma can be easily diagnosed by clinical evaluation combined with an MRI. This is supported by a report of 11 cases and literature review of 16cases by M. Boukobza et al. [8], who describes the specific MRI features of an epidural hematoma.
As for the steroid component that was injected in this case as the causative factor of the development of cauda equina syndrome. A literature search found 2 case reports by Scott D. Hodges et al. [9] who reported cervical epidural steroid injection with intrinsic spinal cord damage. He contributed the permanent neurological deficit to either, direct spinal cord injury by the penetrating needle, adverse effect of neural tissue exposure to the injection, or a combination of both factors.
From this extensive discussion it is shown that the development of cauda equina syndrome following spinal epidural injection occur due to
a) Local anesthetic neurotoxicity of both lignocaine and bupivacaine,
b) Direct trauma to the spinal cord during penetration,
c) Compromise of blood supply to the cord,
d) Loculation of the injected fluid,
e) The development of a spinal epidural hematoma.
All these cases resulted in permanent neurological deficit with only one case reported to have spontaneous full neurological recovery after 8hours. In our case however, there was no spontaneous neurological recovery even after 6 days, MRI and intra- operative findings shows no evidence of an epidural hematoma.
Clinically no evidence suggesting direct trauma to the spinal cord during the injection as it was done with patient fully conscious and there was no blood or cerebrospinal fluid aspirated prior to the administration of the drugs, no pain or paresthesia during needle placement or drug injection and a single attempt only was done. Only 1ml chirocaine (Levobupivacaine HCL 5.0mg) was administered, thus the complication of LA toxicity is less likely. In addition to all this, the return of full neurological recovery following laminectomy of the L4/L5 and L5/S1 level points more to a mechanical pathology as the cause of the cauda equina syndrome.
Conclusion
In conclusion, in such similar cases should no spontaneous neurology recovery occurs, an emergency laminectomy should be considered as the benefit clearly outweighs the risk as evident by this case. The authors deduce that the possible cause of cauda equina in this case is due to possible loculation of the injected fluid or collection of the sediment of the epidural cocktail (Figure 8) within the epidural space of the lumbar region. Although only minimal fluid injected (2mls) it is significant enough to cause compression effect as the spinal canal is already severely stenosed (7mm). However more similar cases need to be reported to prove this theory.

Informed consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Lavy C, James A, Wilson-MacDonald J, Fairbank J (2010) Cauda equina syndrome. Obstetric Anesthesia digest 30(1): 16-17.
- Bilir A, Gulec S (2006) Cauda equina syndrome after epidural steroid injection: A case report. J Manipulative Physiol Ther 29(6): 492.e1-492.e3.
- Loo CC, Irestedt L (1999) Cauda equina syndrome after spinal anaesthesia with hyperbaric 5% lignocaine: A review of six cases of cauda equina syndrome reported to the Swedish Pharmaceutical Insurance 1993- 1997. Acta Anaesthesiol Scand 43(4): 371-9.
- Gerancher JC (1997) Cauda equina syndrome following a single spinal administration of 5% hyperbaric lidocaine through a 25- guage Whitacre needle. Anesthesiology 87(3): 687- 689.
- Kubina P, Gupta A, Oscarsson A, Axelsson K, Bengtsson M (1997) Two cases of cauda equina syndrome following spinal- epidural anesthesia. Reg Anesth 22(5): 447-450.
- Chabbouh T, Lentschener C, Zuber M, Jude N, Delaitre B, et al. (2005) Persistent cauda equina syndrome with no identifiable facilitating condition after an uneventful single spinal administration of 0.5% hyperbaric bupivacaine. Anesth Analg 101(6): 1847-1848.
- Boukobza M, Guichard JP, Boissonet M, George B, Reizine D, et al. (1994) Spinal epidural hematoma: report of 11 cases and review of the literature. Neuroradiology 36(6): 456-459.
- Khaled KM, Awad JN (2004) Spinal epidural hematoma causing acute cauda equina syndrome. Neurosurg Focus 16(6): e1.
- Hodges SD, Castleberg RL, Miller T, Ward R, Thornburg C (1998) Cervical epidural steroid injection with intrinsic spinal cord damage. Spine 23(19): 2137-2142.






























