Quantitative Analysis of Bone Allograft Utilization in Laminectomies and Discectomies: A Study from a Tertiary Care Hospital in South East Michigan
Imran Moinuddin*, Peter Millward and Craig Fletcher
Department of Pathology and Laboratory Medicine, Beaumont Hospital, USA
Submission: June 07, 2018; Published: July 30, 2018
*Corresponding author: Imran Moinuddin, Department of Pathology and Laboratory Medicine, Beaumont Hospital, USA, Email: imranahmed80@gmail.com
How to cite this article: Imran Moinuddin, Peter Millward, Craig Fletcher. Quantitative Analysis of Bone Allograft Utilization in Laminectomies and Discectomies: A Study from a Tertiary Care Hospital in South East Michigan. JOJ Orthoped Ortho Surg. 2018; 1(5): 555574. DOI: 10.19080/JOJOOS.2018.01.555574
Abstract
Bone grafts have been used in orthopedic reconstructive procedures for over a hundred years. Use of autografts is considered to be the ideal choice, but limited availability and associated complications makes their use unfeasible in all orthopedic reconstructive procedures. Alternatives such as allografts and bone graft substitutes were introduced in 1980’s. Although the use of bone allografts in U.S.A has increased over the last few years, compilation of data to quantify their utilization is still lacking. We performed a retrospective chart review study to quantify the bone allograft utilization in laminectomies and discectomies performed at Beaumont Hospital Royal Oak between October 1, 2017 and December 31, 2017.
We determined the type and quantity of bone allografts that were issued for each of the included 79 laminectomies and 55 discectomies. This was followed by quantitative analysis of the specific bone allograft used for each included procedure in addition to calculating the “tissue crossmatch to transplant ratio”. Amongst 79 cases of laminectomies, the bone allograft that was issued and used in highest quantity was Crushed Cancellous (CRC). Amongst 55 cases of discectomies, Grafton Putty (GRP) was issued and used in highest quantity. Trinity Elite Medium (TRN-M) was issued for highest number of laminectomy cases (45.5%) and was also used in most number of laminectomy cases (44.3%). GRP was issued for and used in most cases of discectomies (69% and 63.6% respectively). Judicious use of allografts during orthopedic reconstructive procedures can help in minimizing tissue wastage and in reducing health care cost burden.
Keywords: Allografts; Laminectomies; Discectomies; Utilization; Bone substitutes
Abbreviations: TRN-M: Trinity Elite Medium; TRN-S: Trinity Elite Small; GRP: Grafton Putty; GRM: Grafton Matrix; ALF: AlloFuse; CRC: Crushed Cancellous; ALS: AlloStem; MAP3: Multipotent Adult Progenitor 3; CSP: Cervical Spacer; UNI: UniLIF; BI4: Bio4
Introduction
Use of bone grafts in orthopedic reconstructive procedures has been in practice for over a hundred years [1]. Autograft is considered to be the ideal option in these procedures; however, limited availability of bone autografts and the associated bone and donor site morbidity was the driving force behind the introduction of bone allografts in early 1980s [2]. A well-established bone dispensing service at the level of community hospitals seems to be imperative due to the increasing volume of orthopedic reconstructive procedures being performed now. Beaumont Hospital in Royal Oak, Michigan has one of the largest tissue and bone dispensing services in the country maintaining strict traceability of the tissues. Despite the increasing use of bone allografts in U.S.A, there is still a lack of data in literature to quantify the utilization of bone allografts. We performed a retrospective chart review study to quantify the utilization of different bone allografts used in laminectomies and discectomies performed at Beaumont Hospital Royal Oak between October 1, 2017 and December 31, 2017.
Materials and Methods
After obtaining the required Institutional Review Board approval from Beaumont Research Institute, we extracted 153 cases of laminectomies and discectomies performed at Beaumont Hospital Royal Oak between October 1, 2017 and December 31, 2017 using the Beaumont Health EMR system. Out of these 153 cases, 19 cases that involved both laminectomy and discectomy in the same operative procedure were excluded. We then reviewed the remaining 134 cases of spine surgeries (79 cases of laminectomies and 55 cases of discectomies) to determine:
- The quantity and type of vendor specific bone allografts that were requested and issued for each of the 134 cases of laminectomies and discectomies,
- The amount / quantity of the specific bone allograft that was used for each included procedure,
- “Tissue crossmatch to transplant ratio” and
- Tissue wastage. Statistical analysis was performed by the biostatistics department at Beaumont Hospital Royal Oak using the chi-square for proportion comparisons to determine the association between the proportion of bone allografts used and the type of orthopedic procedure involved (laminectomies vs. discectomies).
- Tomford WW (2000) Bone Allografts: Past, present and future. Cell and Tissue Banking 1: 105-109.
- Mohd S, Yusof N, Ramalingam S, Mansor A (2017) Knowledge on Bone Banking among Participants in an Orthopaedic Conference: A Preliminary Survey. Malays Orthop J 11(2): 1-6.
- Kinaci A, Neuhaus V, Ring DC (2014). Trends in Bone Graft Use in the United States. Orthopedics 37(9): 783-788.
- Fischer CR, Cassilly R, Cantor W (2013) A systematic review of comparative studies on bone graft alternatives for common spine fusion procedures. Eur Spine J 22(6): 1423-1435.
- Keating JF, McQueen MM (2001) Substitutes for autologous bone graft in orthopaedic trauma. J Bone Joint Surg Br 83(1): 3-8.
- Bucholz RW (2002) Nonallograft osteoconductive bone graft Substitutes. Clin Orthop 395: 44-52.
- Bostrom MP, Seigerman DA (2005) The clinical use of allografts, demineralized bone matrices, synthetic bone graft substitutes and osteoinductive growth factors: a survey study. HSS J 1(1): 9-18.
- Meermans G,Roos J ,Hofkens L,Cheyns P (2007) Bone banking in a community hospital. Acta Orthop Belg 73(6): 754-759.
- Hernigou P (2015) Bone transplantation and tissue engineering, part III: allografts, bone grafting and bone banking in the twentieth century. Int Orthop 39(3): 577-587.
- Czitrom AA, Gross AE, Langer F, Sim FH (1998) Bone banks and allografts in community practice. Instr Course Lect 37: 13-24.
Results
The bone allograft that was issued and used in highest quantity in the 79 reviewed cases of laminectomies was Crushed Cancellous (CRC) followed by Trinity Elite Medium (TRN-M). A total of 127 CRC units were issued for laminectomies and out of these, 110 CRC units were used. In comparison, the bone allograft that was issued and used in highest quantity in the 55 reviewed cases of discectomies was Grafton Putty (GRP). A total of 74 units of GRP were issued for discectomies and out of these, 43 GRP units were used. A detailed breakdown of different allografts utilized in laminectomies and discectomies is shown is table 1 and table 2 respectively.
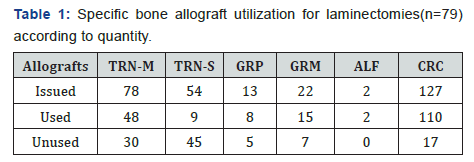
TRN-M: Trinity Elite Medium; TRN-S: Trinity Elite Small; GRP: Grafton Putty; GRM: Grafton Matrix; ALF: AlloFuse; CRC: Crushed Cancellous
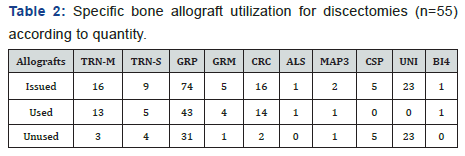
TRN-M: Trinity Medium; TRN-S: Trinity Small; GRP: Grafton Putty; GRM: Grafton Matrix; CRC: Crushed Cancellous; ALS: AlloStem; MAP3: Multipotent Adult Progenitor 3; CSP: Cervical Spacer; UNI: UniLIF; BI4: Bio4
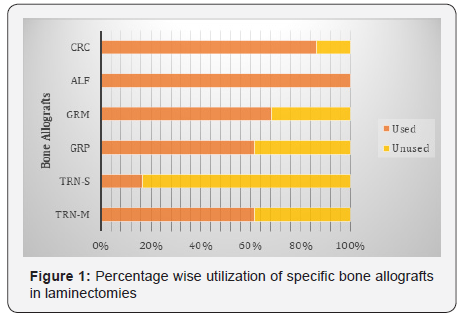
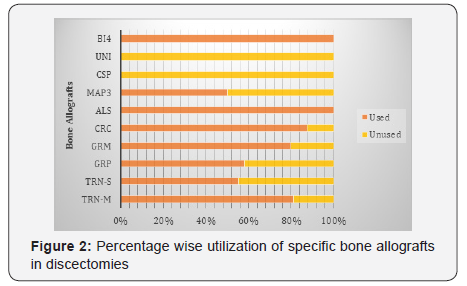
Amongst the main bone allografts issued for laminectomies, more than 80% of issued CRC units were used; whereas close to 65% of issued units of TRN-M and GRM were used. Amongst the main bone allografts issued for discectomies, close to 90% of issued CRC units were used; whereas almost 80% of issued TRN-M units were used and almost 60% of issued GRP units were used. Figures 1 & 2 represent percentage wise usage of different allografts in laminectomies and discectomies respectively. The unused units were returned back to our tissue service, except for those that got wasted after being issued for the procedure. Out of all the bone allografts issued for laminectomies, one TRN-M unit got wasted. Similarly, out of all the bone allografts issued for discectomies, one TRN-S unit got wasted (Figures 1 & 2).
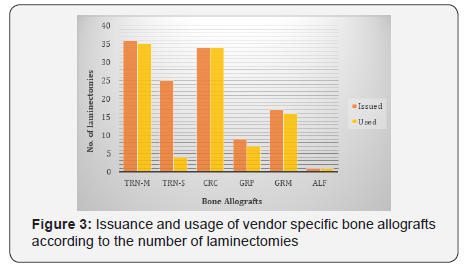
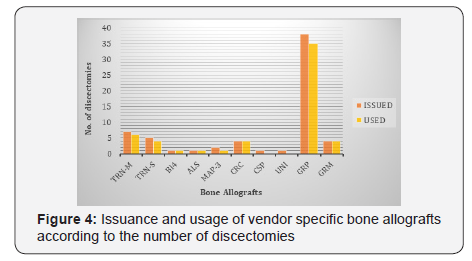
Amongst the 79 reviewed cases of laminectomies, TRN-M either alone or in combination with another allograft was issued for most cases of laminectomies (36 out of 79 cases; 45.5%), followed by CRC either alone or in combination with another allograft (34 out of 79 cases; 43%). TRN-M either alone or in combination with another allograft was also the tissue that was used in most cases of laminectomies (35 out of 79 cases; 44.3%) followed by CRC (34 out of 79 cases; 43%). These findings are shown in (Figure 3). Out of all bone allografts utilized in discectomies, GRP was issued for most cases of discectomies (38 out 55 cases; 69%); while ALS, BI4, CSP and UNI were each issued for least number of discectomies (1.8%). Out of all the bone allografts issued for discectomies, GRP was used in most number of discectomies (35 out 55 cases; 63.6%); while CSP and UNI were not used in any of the discectomy cases. These findings are shown in Figure 4. The proportion of bone allografts used in laminectomies versus discectomies was statistically significant (p = 0.025) (Figure 4).
Discussion
Bone grafts and bone graft substitutes are used to provide structural support and to augment bone healing. Autologous, allogeneic, and artificial bone grafts each have their own advantages and drawbacks. New operative techniques in addition to advancement in allografts and synthetic bone grafts over the last few decades have influenced the selection of bone grafts used in orthopedic reconstructive procedures [3]. Autologous bone graft is considered the prime option, but it still carries the risk of bone and donor site morbidity [4]. In addition, limited availability of autologous bone grafts is a barrier in their utilization particularly in orthopedic procedures that require large amounts of bone grafts [5]. Limited quantity of autologous bone grafts in addition to increasing number of orthopedic reconstructive procedures being performed now has led to a higher demand for bone allografts and bone graft substitutes. The number of bone grafting procedures performed each year in the United States is estimated to be around 500,000 to 600,000 [6]. Approximately 1400 products are available in the international market for use as bone fillers, but an optimal bone graft substitute with little or no associated complications and risks does not exist at this time [4]. Consensus regarding the use of a specific type of bone graft for any orthopedic procedure still does not exist [7].
Despite the increasing use of bone allografts in U.S.A, there is still a lack of data in literature to quantify the utilization of bone grafts. S Mohd et al. [2] in 2017 also acknowledged that there was still a lack of data to assess the awareness and understanding of orthopedic community about bone banking in Malaysia [2]. Results from an awareness survey conducted by S Mohd et al. [2] regarding tissue banking and bone grafts showed that 82.5% respondents were aware about tissue banking, however only 12.5% knew about the existence of tissue banks in Malaysia [2].
Meermans G et al. [8] in 2007 evaluated the indications and results of the allograft utilization from the local bone bank and concluded that out of 131 allografts stored in the bone bank, only 20 were discarded [8]. In our study, out of 295 bone allograft units issued for laminectomies, only one TRN-M unit got wasted. Similarly, out of 152 bone allograft units issued for discectomies, only one TRN-S unit got wasted. The concept of bone banking originated in early 20th century and bone allograft utilization has increased in popularity since then [9]. The need for establishment of bone bank in community hospitals is supported and justified by the increasing volume of orthopedic reconstructive procedures being performed in community hospitals over the last few years [10]. Community hospital bone banks can prove to be a very beneficial and cost-effective tool for the healthcare structure in general, if guidelines to ensure proper screening of donor bone and dependable preservation of bone grafts are followed strictly [10].
Conclusion
Our study results showed that 4 main vendor specific bone allografts (CRC, TRN-M, TRN-S and GRM) were issued for laminectomies; whereas GRP was found to be the only main vendor specific bone allograft that was requested and issued for discectomies. Our study demonstrated that the “tissue crossmatch to transplant ratio” was 1.5 for laminectomies and 1.85 for discectomies. We conclude that judicious use of allografts during orthopedic reconstructive procedures and increased awareness about bone allografts amongst orthopedic and neurospine community can be helpful in minimizing the tissue wastage, thereby ensuring adequate availability of these tissues in addition to reducing the health care cost burden.
Conflict of Interest
Authors do not have any potential conflict of interest.






























