Functional Results of Total Hip Arthroplasty for Ankylosed Hip
Yildiz Analay Akbaba2*, Ata Can1 and Fahri Erdogan3
1Department of Surgery, Istanbul Surgery Hospital, Istanbul, Turkey
2Department of Physiotherapy and Rehabilitation, Istanbul University, Turkey
3Department of Orthopaedics and Traumatology, Istanbul University, Turkey
Submission: January 29, 2018; Published: February 09, 2018
*Corresponding author: Yildiz Analay Akbaba, Istanbul University, Faculty of Health Sciences, Division of Physiotherapy and Rehabilitation, Demirkapi cad, Karabal sk, Bakirkoy, Istanbul, Turkey, 34147, Tel: 0090 212 4141528- 40169; Fax: 0090 212 4141515; Email: yildizanalay@yahoo.com; yildizanalay@istanbul.edu.tr
How to cite this article: Yyldyz Analay Akbaba, Ata Can, Fahri Erdogan. Functional Results of Total Hip Arthroplasty for Ankylosed Hip. JOJ Orthoped Ortho Surg. 2018; 1(3): 555564. DOI: 10.19080/JOJOOS.2018.01.555564
Abstract
Objective: To evaluate the long term results of THA in patients with surgically hip ankylosed and define a postoperative rehabilitation program for this patients.
Materials & Methods: Seven patients’ 8 hips in whom ankylosed hips were converted to total hip arthroplasty between October 2011 and November 2015. All patients had surgery ankylosis. All patients received the same rehabilitation program after total hip arthroplasty. The patients evaluated before surgery and after 1 year surgery for lomber and kontralateral hip pain, hip joint range of motion, funtional status and satisfaction from treatment.
Result: In our study the etiology of the ankylosis was tuberculous septic arthritis in 2 (25%] and developmental hip dysplasia in 6 (75%] hips. The mean duration of the surgical ankylosis before conversion surgery was 29±13.6 years. The mean age of the patients was 41.5±14.5 years (mean ± SD] met all of the inclusion criteria. All patients had osseous ankylosis and the indications for arthroplasty were intractable low back pain in 6 patients (85.7%], hip pain in 4 patients (57.1%]. Complications occurred in two patients.
The mean follow-up period was 13±2.7 months. There was statistically significant improvement in lomber and contra lateral hip pain, hip joint range of motion, functional status and satisfaction from treatment after treatment (P=0.00]. One-hundred percent of patients were stated that they were much better than before treatment.
Conclusion: Function, range of motion of hip, lumbar and contralateral hip pain on the same side showed a marked improvement after conversion of hip ankylosis to total hip arthroplasty.
Keywords: Hip Ankylosis, Arthroplasty, Function, Pain, Arthrodese, Rehabilitation
Abbreviations: DDH: Developmental Dysplasia of the Hip; THA: Total Hip Arthroplasty; VAS: Visual Analogue Scale; HHS: Harris Hip Score
Introduction
Ankylosis of the hip can occur spontaneously or it can be performed surgically (arthrodesis]. Surgical ankylosis of the hip was initially indicated for the management of conditions such as sepsis, developmental dysplasia of the hip (DDH], significant deformity of the femur or acetabulum that is not suitable for total hip arthroplasty (THA], neurological disorders that cause a high risk of dislocation and it remains a viable option in young patients who are not ideal candidates for other treatment options [1,2]. Including the lumbosacral spine and ipsilateral knee, hip ankylosis alters the biomechanics of the adjacent joints, as well as the contralateral hip and knee. In addition, there is increased motion of the lumbar spine, increased lordosis with pelvic tilt. This often results in increased pain and decreased functional capacity several decades after the ankylosis [2-4]. These symptoms may be reduced with conversion THA of the ankylosed hip. Conversion THA was known to effectively relieve or eliminate these symptoms, not only improving overall patient function and satisfaction, but also returning to daily activities [5,6].
THA in the ankylosed hip is a technically difficult procedure. Bone deformation, atrophy and contracture of surrounding soft tissues, effects of the previous operation, and alterations of normal anatomy all increase the difficulty of this procedure. The overall clinical outcome is generally less satisfactory than routine THA performed for osteoarthritis and other etiologies. There are case reports in this matter, but the number of clinical trials with large number of cases is insufficient. The postoperative rehabilitation program should be well designed because of the difficulty of the surgery procedure and the limitation of range of motion and excessive loss of muscle strength. But no specific rehabilitation program has been reported until now for these patients. The aim of this study was to evaluate the long term results of THA in patients with surgically hip ankylosed and define a postoperative rehabilitation program for patients with THA.
Materials and Methods
Trial Design The clinical study was designed as a prospective study. This study was performed at the Istanbul University The research protocol was confirmed by the Research Ethics Committee of the Human Research Ethics Committee of Bakirkoy Sadi Konuk Training and Research Hospital (IRB: 2012/271). (Institutional review board approval no....). The present study was conducted in accordance with the Declaration of Helsinki. Informed consent was provided to all patients prior to their enrolment in the study.
Participants
The participants were recruited from Istanbul University, Department of Orthopaedics and Traumatology and treated at the Istanbul University, Faculty of Health Sciences, Division of Physiotherapy and Rehabilitation from October 2012 to November 2016. Seven patients' 8 hips in which ankylosed hips were converted to THR were diagnosed and operated by an orthopedic surgeon. Preoperative and postoperative clinical assessments and rehabilitation program were performed by the same physiotherapist at a university research clinic. Patients with spontaneous hip ankylosis were excluded from the study. Only patients who were previously surgically ankylosed were included in the study. The demographic and clinical features of all patients were recorded. Intraoperative or postoperative complications were recorded.
Surgical Technique
First-generation cephalosporin was administered 30 minutes before the operation. Under epidural anesthesia, patient positioned in the lateral decubitus position and the affected hip was prepared. An incision approximately 10 cm in length was made as used in anterolateral approach. Gluteus medius muscle partially detached from the trochanter major. Next, the joint capsule was resected and femoral neck, the site of the fusion between the ileum and the femoral head were clearly visualized. Then a subcapital osteotomy has done. Femur was positioned and visualized properly for a more precise femoral neck osteotomy located approximately 1 cm proximal to the trochanter minor.
The bone between these cuts was removed and true acetabulum was exposed with the removal of soft tissues. Next, the diameter of the reamer was successively increased until subchondral bone was observed. After trials, the hemispheric cementless acetabular cup was installed at a proper anteversion and abduction angle. Two to three screws were used for acetabular fixation. Matched polyethylene or ceramic linings were placed inside the component. When confirmed stable, the resected femur exposed. After preparation of the femoral canal with appropriate anteversion, the femoral component and femoral head trials were installed. The hip joint was then restored, and joint stability, range of motion and limb length was evaluated. The cementless femoral component and appropriate femoral head were implanted, and the incision was washed with saline. After the placement of drainage tube, all layers of the incision were sutured. For the bilaterally operated patient contralateral hip was operated using the same technique. Drains were removed 24 h after the operation.
Outcome Measures
Pain intensity was assessed using the Visual Analogue Scale (VAS) (0 -10) for lumbar and kontralateral hip region [7]. Active hip flexion, abduction, extension and external-internal rotation ROM were assessed using a standard goniometer. Abductor muscle strength was assessed with the manual muscle test. Function was assessed by Harris Hip Score (HHS). HHS was developed for the assessment of the results of hip surgery [8]. The domains covered are pain, function, absence of deformity, and range of motion. The score has a maximum of 100 points. A Harris score of 90-100 was considered excellent, 80-89 was considered good, 70-79 was considered fine and <70 was considered poor. For objective satisfaction assessment, patients were asked whether they would undergo the operation again or not. The prosthesis position and surrounding bone changes were observed with X-rays of the hips at the final follow-up and compared with the previous X-rays.
Follow-up
All outcome measures were performed twice (before surgery and in the first year of surgery). Consultation of patients was performed in the first, third and twelfth month after operation.
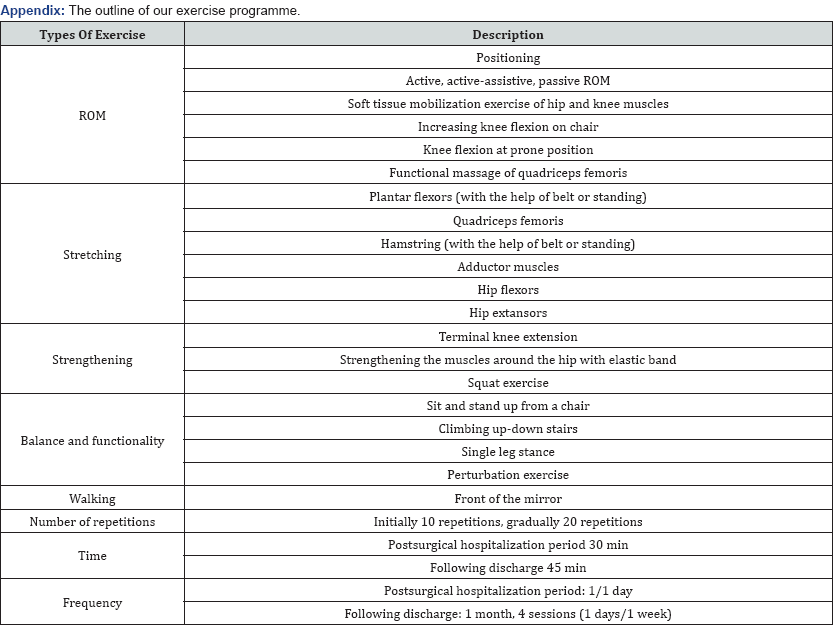
Interventions: All patients were taken on postoperative first day education and rehabilitation program in order to avoid complications and to gain early mobilization, range of motion and function. Exercise programs were implemented everyday supervised by a physiotherapist during their hospitalization period. Patients may need to use a can or walker to reduce limp for an extended period postoperatively, depending on the functional capacity of quadriceps muscle and hip abductors. Patients were allowed immediate full weight bearing. Only one patient had intra-operative fracture of the greater trochanter that was allowed full weight bearing at the second month. Hip flexor and abductor stretching exercises should be instituted on immediate term. Patient education program including positioning and transfer activities from bed to chair, from chair to bed. Exercises were commenced with a repeat of 10 times, and number of repeats increased if needed. Following discharge from hospital, patients were invited to hospital once in a week for 1 month to update the exercise program and instructions and to improve the patient compliance. Exercise programs were revised for all patients and new exercises were added. The outline of rehabilitation programs for patients in “Appendix”.A long period of rehabilitation is typically required to achieve maximal functional capacity. For this reason, we recommended a home-based exercise program for all patients.
Data Analysis: Sample-size calculation was based on the clinically important improvement of 10 mm points on a 0-to-100 HHS for function, Data analyses were performed using the SPSS Version 20.0 statistical software package (SPSS Inc., Chicago, IL]. The "Paired-Samples T Test" was used to comparison the normality of the data between preoperative and postoperative clinical outcome of the cases. Statistical significance was set for all testing at P< 0.05. Data are expressed as the mean±standard deviation.
Results
Seven patients (mean ± SD age, 41.5±14.5 years (range 15 - 69], 6 female] met all of the inclusion criteria. One patient had bilateral hip fusion and underwent bilateral synchronous THA, thus 8 hips were evaluated at the final follow-up and included in this study. The etiology of the ankylosis was tuberculous septic arthritis in 2 (25%] and developmental hip dysplasia in 6 (75%] hips. The mean duration of the surgical arthrodesis before conversion surgery was 29±13.6 (range 9-49] years. The mean follow-up period was 13±2.7 months. All patients had osseous ankylosis and the indications for arthroplasty were intractable low back pain in 6 patients (85.7%], contralateral hip pain in 4 patients (57.1%]. All but two patients had perceptible contraction of the abductor muscles on palpation preoperatively. Previously operated limb was shorter than the contralateral (not affected] limb. The mean limb-length discrepancy was 3.2 cm (range 0-6 cm] preoperatively. Complications occurred in two patients. One patient had intra-operative fracture of the greater trochanter that was treated with the help of trochanteric grip and cables. The other patient experienced arterial damage that required an external iliac-femoral artery anastomosis at postoperative fifteenth day.
The patients with arterial damage had an acute increase in thigh pain and increased circumference along with the firmness after discharge from the hospital at postoperative day 15. Although the patient did not manifest any neurovascular problem in the immediate postoperative period; at the time of presentation, her distal pulses were absent. Vascular surgery consultation was undertaken and emergency arteriography revealed a left femoral artery tear of 4 cm, causing total obstruction. Exploration allowed us to locate the intimal tear and this was treated surgically with a bypass between external iliac and femoral arteries using a patch. Perioperatively, contact of acetabular cup or screws with the problematic segment could not be revealed and the vessel wall was intact. After vascular surgery, the distal peripheral pulses were symmetrical and the patient recovered but at the final follow-up she had severe limitations in her hip movements thus still satisfied with the surgical outcome. Both patients recovered uneventfully. No patients had heterotrophic ossification, sciatic nerve palsy or dislocation during the study period. No patients had sings of loosening around acetabular and femoral components and required a revision surgery because of this. Clinical outcomes of the patients were presented. There was statistically significant improvement in lumbar and contralateral hip pain, funtional status, hip joint range of motion and abductor muscles strength after treatment (P=0.00)( Table 1). Three of seven patients in our study still need to use crutches especially for long distances. All patients had limping because of abductor weakness. One- hundred percent of patients were stated that they were much better than before treatment.

Paired-Samples T Test, n.s.: p > 0.05.
SD: Standard Deviation; HHS: Harris Hip Score; VAS: Visual Analogue Scale; IR: Internal Rotation, ER: External Rotation
Discussion
This study shows that conversion total hip arthroplasty (THA) of the ankylosed hip effective a method on pain, ROM, function and patient satisfaction. Nowadays, hip arthrodesis is used less commonly in orthopaedic practice because of the higher patient expectations and improved results of total joint replacement. But, there are a group of patients with their hips got arthrodesed due to several reasons like DDH, septic arthritis or ankylosing spondylitis. If bony union is achieved, the overall results of arthrodesis are generally good [3]. Altered biomechanics secondary to hip ankylosis often result in degeneration and pain of the lumbar spine, ipsilateral knee, contralateral hip and knee. Nearly 10% of patients start to experience adjacent joint pain by two years and this involvement increases with time [9].
Kirkos et al. [10] reported that in patients with hip ankylosis; 75% had lomber pain, 66% had knee pain and 33% had contralateral hip pain after a mean follow-up of 37 years. Similarly, after a mean of 29 years with ankylosis; 6/7 (85.7%) of our patients had back pain and 4/7 (57.1%) of our patients had contralateral hip pain before surgery. Although our patients can not reflect the whole population of arthrodesed patients; they show us that patients suffering from pain seek for a solution. All patients with lomber and contralateral hip pain reported relief following THA. This improvement is similar with the previous studies results [11-13]. Pain may be contributed to previous degeneration of adjacent joints but improved alignment is enough for patient satisfaction even the existing degeneration does not resolve.
Reported complication rates in the literature vary widely from 11% to 54% [14-17]. Mechanical failure, infection, nerve palsy, heterotophic ossification, fractures related with greater trochanter or femoral shaft, incomplete removal of bone block, dislocation, malalignment and arterial damage can be listed as reported complications [3,18]. Shoenfeld, et al. [19] studied 68 vascular complications associated with THA and reported that incorporation of iliac vessels in cement, misplaced Hohmann retractor, excessive traction on the vessels and intrapelvic migration of an acetabular component are most common causes of vascular injuries but there are still 16% of cases remain unexplained. We experienced one minor (intraoperative fracture of greater trochanter) and one major (arterial damage) complication. We accounted the fracture of the trochanter to lower bone quality and difficulty in reduction of the hip because of the tightness of abductor muscles.
Thus, this risk must be kept in mind and forceful manipulation should be avoided. Additionally, we think that muscle wasting, scar alteration and position of the hip in an arthrodesed situation for a long period (in our case 33.5 years] could lead to anatomical changes and this may explain torsion related arterial damage without an obvious insult to the vessel. Kim et al. [20] reported in their study that HHS increased from 55.4 to 82.3 points in average 11 years. Our data confirm that HHSs after surgery compared with before surgery showed considerable progress, so that mean HHS of 56.13±20.48 was improved to 90.63±6.56 at the final follow-up. The change in HHS after THR was greater in our series than in other studies [11,21-23]. This difference may be related with limited number of patients in the study group. An optimal hip position of 20° to 30° flexion, 20° of abduction, 5° to 10° of external rotation is required to achieve a successful outcome from arthrodesis [24,25].
Bhatti et al. [26] reported in their case report that patient had 20° fixed flexion, 10° internal rotation and 10° adduction deformities. Howard et al had reported patients with surgical arthrodesis 45°-60° hip flexion angle [27]. Our patients also had similar range of motion before conversion surgery. Hip abductor muscle strength continued to improve for ≥2 years following conversion THA [28]. Limping is a common finding after conversion to THR. Limping is related with weakness of abductor muscles but it may not affect patient satisfaction negatively [18]. This is also valid for our patient population. Three of seven patients in our study still need to use crutches especially for long distances. Functional integrity of the hip abductor muscles is the most important predictor of walking ability following conversion THA. But, limitation of active use after a hip arthrodesis is associated with atrophy, fibrosis and fatty degeneration within the abductor muscles along with the scarring and devascularization from previous operations and if the duration of the arthrodesis is long than you can expect to see degenerative process more diffusely [29,30]. Our two patients with shortest time to conversion (6 years and 9 years, respectively] had nearly normal postoperative abductor muscle strength. But we need to expand our study population to validate this finding.
All of patients are satisfied with their surgical outcome and stated that they will have the surgery again under the same circumstances. This study had several strengths. First, it was a prospective clinical trial. Second, all hips included in our cases were hips with surgical arthrodesis. The other ankylosed hips were excluded Third, this is the first study to report the relationship between rehabilitation and the effectiveness of kinesiotaping. In their study, many researchers establish THA for ankylosed hip, but none of the researchers have been reported a specific rehabilitation program until now. However, the study also has some limitations. The major limitation of our study is inclusion of small number of patients with short follow- up time. However, hip conversion arthroplasty is not a routinely performed procedure, thus 8 hips, all with surgical arthrodesis can be considered enough. Another limitation is lack of a control group and retrospective nature of our study.
Conclusion
Conversion of a previously arthrodesed hip to total joint arthroplasty is an effective method that provides patient satisfaction and improves function, range of motion, pain and symptoms of adjacent joints.
Conflict of Interest
The authors declare that there is no financial interest or any conflict of interest.
Appendix: The outline of our exercise programme.
References
- Whitehouse M, C Duncan (2013) Conversion of hip fusion to total hip replacement. Bone Joint J 95(11 Supple A): 114-119.
- Swanson MA, MH Huo (2011) Total hip arthroplasty in the ankylosed hip. Journal of the American Academy of Orthopaedic Surgeons 19(12): 737-745.
- Jain S, Giannoudis PV (2013) Arthrodesis of the Hip and Conversion to Total Hip Arthroplasty: A Systematic Review. J Arthroplasty 28(9): 1596-1602.
- Aderinto J, Lulu OB, Backstein DJ, Safir O, Gross AE (2012) Functional results and complications following conversion of hip fusion to total hip replacement. J Bone Joint Surg Br 94(11 Suppl A): 36-41.
- Stover MD, Beaule P, Matta JM, Mast JW (2004) Hip arthrodesis: a procedure for the new millenium? Clin Orthop Relat Res 418: 126-133.
- Park KS, Taek-Rim Yoon, Lee TM, Ahn YS (2015) Ceramic on ceramic hip arthroplasty in fused hips. Indian J Orthop 49(3): 336-341.
- Carlsson AM (1983) Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 16(1): 87-101.
- Nilsdotter A, A Bremander (2011) Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res 63 Suppl 11: S200-S207.
- Matta JM, Siebenrock KA, Gautier E, Mehne D, Ganz R (1997) Hip fusion through an anterior approach with the use of a ventral plate. Clin Orthop Relat Res (337): 129-139.
- Kirkos JM, Papavasiliou KA, Kyrkos MJ, Sayegh FE, Kapetanos GA (2008) The long-term effects of hip fusion on the adjacent joints. Acta Orthop Belg 74(6): 779-787.
- Fernandez-Fairen M, Murcia-Mazon A, Torres A, Querales V, Murcia A (2011) Is total hip arthroplasty after hip arthrodesis as good as primary arthroplasty? Clin Orthop Relat Res 469(7): 1971-1983.
- Rutz E, Schäfer D, Valderrabano V (2009) Total hip arthroplasty after hip joint ankylosis. J Orthop Sci 14(6): 727-731.
- Schäfer D, Dick W, Morscher E (2000) Total hip arthroplasty after arthrodesis of the hip joint. Arch Orthop Trauma Surg 120(3-4): 176178.
- Hamadouche M, Kerboull L, Meunier A, Courpied JP, Kerboull M (2001) Total hip arthroplasty for the treatment of ankylosed hips : a five to twenty-one-year follow-up study. J Bone Joint Surg Am 83-A(7): 992998.
- Joshi AB, Markovic L, Hardinge K, Murphy JC (2002) Conversion of a fused hip to total hip arthroplasty. J Bone Joint Surg Am 84-A(8): 13351341.
- Richards CJ, CP Duncan (2011) Conversion of hip arthrodesis to total hip arthroplasty: survivorship and clinical outcome. J Arthroplasty 26(3): 409-413.
- Peterson ED, Joseph P Nemanich, Aaron Altenburg, Miguel Cabanela E (2009) Hip throplasty after previous arthrodesis. Clin Orthop Relat Res 467(11): 2880-2885.
- Villanueva M, Sobron FB, Parra J, Rojo JM, Chana F, et al. (2013) HSS J 9(2): 138-144.
- Schoenfeld NA, Stuchin SA, Pearl R, Haveson S (1990) The management of vascular injuries associated with total hip arthroplasty. J Vasc Surg 11(4): 549-555.
- Kim YL, Shin SI, Nam KW, Yoo JJ, Kim YM, et al. (2007) Total hip arthroplasty for bilaterally ankylosed hips. The Journal of arthroplasty 22(7): 1037-1041.
- Morsi E (2007) Total hip arthroplasty for fused hips: planning and techniques. J Arthroplasty 22(6): 871-875.
- Rittmeister M, SM, Zichner L (2000) Hip and knee replacement after longstanding hip arthrodesis. Clin Orthop Relat Res 371: 136-145.
- Kim YL, Shin SI, Nam KW, Yoo JJ, Kim YM, et al. (2007) Total hip arthroplasty for bilaterally ankylosed hips. J Arthroplasty 22(7): 10371041.
- Beaulé PE, Matta JM, Mast JW (2002) Mast, Hip arthrodesis: current indications and techniques. J Am Acad Orthop Surg 10(4): 249-258.
- Bonin SJ, Eltoukhy MA, Hodge WA, Asfour SS (2012) Conversion of fused hip to total hip arthroplasty with presurgical and postsurgical gait studies. J Arthroplasty 27(3): 493. e9-493. e12.
- Bhatti A, Khan KM, Rasheed K, Minhas MS (2012) Total Hip Arthroplasty for Childhood Fused Hip. J Coll Physicians Surg Pak 22(9): 598-600.
- Howard M, Bruce WJ, Walsh W, Goldberg JA (2002) Total hip arthroplasty for arthrodesed hips. J Arthroplasty 10(1): 29-33.
- Swanson MA, MH Huo (2011) Total hip arthroplasty in the ankylosed hip. J Am Acad Orthop Surg 19(12): 737-745.
- Reikeras O, Bjerkreim I, Gundersson R (1995) Total hip arthroplasty for arthrodesed hips: 5 - 13 year results. J Arthroplasty 10(4): 529-532.
- Kilgus DJ, Amstutz HC, Wolgin MA, Dorey FJ (1990) Joint replacement for ankylosed hips. J Bone Joint Surg Am 72(1): 45-54.






