Abstract
Background: Prematurity is associated with a higher prevalence of visual and neurocognitive impairments not only during the neonatal period but also throughout childhood and adolescence.
Objective: To design a comprehensive health care model for pediatric patients screened under the National Program for the Care of Retinopathy of Prematurity.
Methodological Design: A multicenter, multistage, mixed-methods study was conducted. In the first stage, the clinical and epidemiological characteristics of children screened between 2002 and 2018 were described. In the second stage, a longitudinal study was carried out involving 60 premature children aged 7 to 18 years-30 diagnosed with retinopathy of prematurity and 30 without the condition. Ophthalmological and neurocognitive sequelae were evaluated and treated. In the third stage, a comprehensive health care model was designed for pediatric patients screened in the program.
Results: A high percentage of patients presented with ophthalmological, neurocognitive, and general disorders. The proposed model takes a holistic and multidisciplinary approach and includes four interrelated components focused on the child/adolescent and their family. Each component generates specific interventions and tools for clinical follow-up, aimed at improving the quality of care.
Conclusions: The health care model was considered highly appropriate by the experts consulted.
Keywords: Prematurity; Retinopathy of Prematurity; Sequelae; Model of Care
Abbreviations: ROP: Retinopathy of Prematurity; NICUs: Neonatal Intensive Care Units; LBW: Low Birth Weight; MGI: Medicina General Integral; PHC: Primary Health Care; MINED: Ministry of Education; TEA: Trastorno Del Espectro Autista
Introduction
Premature birth rates are increasing worldwide due to adolescent pregnancies, pregnancies at extreme maternal ages, and risk factors such as hypertension, gestational diabetes, and multiple pregnancies resulting from assisted reproductive treatments [1,2]. Retinopathy of prematurity (ROP) is a vitreoretinal, Vaso proliferative, and multifactorial disease characterized by an interruption of normal vasculogenic, leading to neovascularization and retinal detachment [3-7]. The main risk factor is vascular imma turity, typically in infants with a birth weight of less than 1500 grams or a gestational age under 30 weeks, or both [3-9].
The prevalence of childhood blindness varies according to each country’s socioeconomic development and infant mortality rate [4-8]. Latin America accounts for two-thirds (24%) of childhood blindness cases due to ROP [5-7]. In Cuba, a country with first-world healthcare services and established neonatal intensive care units (NICUs), survival is possible for infants weighing less than 1250 grams, with low infant mortality rates of under 7.9 deaths per 1,000 live births [4,8,9]. The “Prevention of Blindness from ROP” project began in Cuba in 2000 [8]. The national rate of ROP was 5.1% in 2010 and increased to 8.6% in 2021 [4,7-9].
In Villa Clara, a NICU reports survival rates above 70% for newborns weighing under 1500 grams. Partial statistical reports by Fariñas Falcón et al [9]. have shown a low incidence of ROP. In 2021, the low birth weight (LBW) index was 7.1%, the survival rate for premature infants was 58.3%, and infant mortality was 7.3%. These outcomes reflect the implementation of national research protocols and technological advances in NICU care. National and international literature reviews show little information on the sequelae during preschool, primary education, and adolescence.
There is a lack of published articles proposing comprehensive health care models to follow up on pediatric patients with these characteristics-developmental stages where the acquisition of skills and knowledge can significantly impact academic performance. Therefore, care for this population must continue beyond the age of six. The health care model emerges from various knowledge streams applicable to the sector to structure regulations and institutional frameworks, supporting the development of a socially responsive health system and reducing uncertainty. It links individual and collective choices and should ensure quality of life for the population [10].
This study integrates medical-social knowledge using clinical, epistemological, holistic, and multidisciplinary criteria essential for delivering care, implementing actions, and developing skills that explain how to carry out this transformation during the school years and adolescence. The economic impact of visual disability is significant, hindering cognitive, academic, and social development in children and adolescents, affecting self-esteem, and limiting access to certain professions.
Therefore, we Pose the Following Scientific Question:
How can comprehensive health care be achieved for pediatric
patients screened in the Retinopathy of Prematurity Program?
General Objective:
To design a comprehensive care model for pediatric patients screened in the Retinopathy of Prematurity (ROP) program.
Methodological Design of the Study
This is a multicenter, multi-stage study that follows a qualitative- quantitative or mixed methodological approach. It was conducted between 2002 and 2019 by a multidisciplinary team comprising specialists from the “Arnaldo Milián Castro” University Clinical-Surgical Hospital, the “Mariana Grajales” University Gyneco- Obstetric Hospital, the “José Luis Miranda” University Pediatric Hospital, and the Mental Health Center of the “Chiqui Gómez-Lubián” University Polyclinic in Santa Clara, Villa Clara.
First Stage
A retrospective descriptive study was carried out on patients included in the “Blindness Prevention Program for Retinopathy of Prematurity,” who were treated in the neonatal care service of the “Mariana Grajales” University Gyneco-Obstetric Hospital from 2002 to 2018. The study population consisted of 1,020 newborns who met the inclusion criteria, and the sample included 58 neonates who were diagnosed with some degree of the disease.
Second Stage
This phase covered the period from 2017 to 2019. A longitudinal mixed-methods study was conducted on pediatric patients aged between 7 and 18 years, who received a health intervention involving Ophthalmology, Psychology, and integrated care. The study population included 495 premature neonates born at the “Mariana Grajales” University Gyneco-Obstetric Hospital in Santa Clara, of whom 45 developed ROP. The non-probabilistic sample, based on specific criteria, consisted of 60 children, 30 who had ROP and 30 who did not-as well as 60 parents or guardians. Socio- demographic and clinical variables were assessed, including ophthalmologic, psychological, and parental satisfaction measures. Pilot surveys were also conducted with general medicine specialists (MGI) and primary health care (PHC) ophthalmologists.
Third Stage - Model Design Phase
1. Preparation Phase: Various aspects and pieces of evidence
were considered:
• The clinical and research experience of the lead doctor
in the “National Project for the Prevention of Blindness from ROP”
• The results from the previous stages
2. Document Analysis: National Program and International
Classification of ROP, ROP National Program
• ROP protocols proposed by the “Ramón Pando Ferrer”
ICO in 2008 and 2018
• The professional development plan of the University of
Medical Sciences of Villa Clara from 2017 to 2021
• The latest five editions of national health statistical yearbooks
in Cuba
• Consultation records for the targeted age group
• A systematic review of health care models
• Group techniques such as nominal and focus groups
• Ethical considerations were also addressed
Fase del diseño del modelo y Valoración por experto (Figure 1).
Discussion of the Results
The most frequent diseases were: chronic lung disease (41.7%), followed by epilepsy (23.3%), musculoskeletal abnormalities and congenital heart disease (11.7%). Speech disorder affected 21.7% of cases, hearing loss 11.7%, psychological disorders were found in five children (8.3%), and autism in two (3.3%). Children with ROP were more affected in percentage terms in most of the recorded diseases (Table 1). This aligns with findings from studies by Rodríguez, Manzitti J, and Ruiz Orosco [4,5,7,11,12]. Mild myopic astigmatism was the most common refractive error, seen in 21 children (35.0%) among those with ROP. High compound myopic astigmatism followed, present in 14 patients (23.3%).
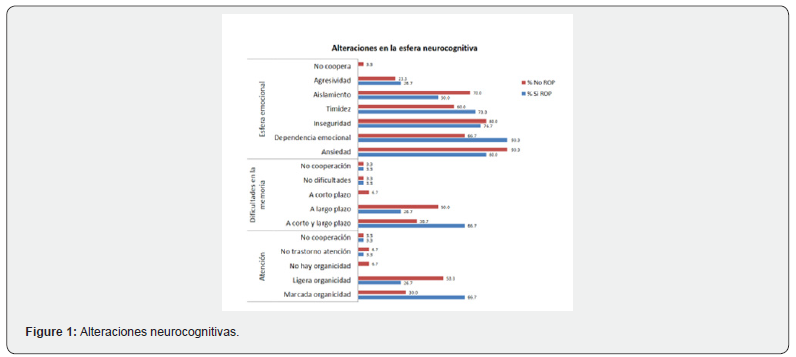

No refractive error was found in 11 children (18.3%) (Table 2), consistent with the findings of Ruiz Orosco H [7,11,12]. Difficulties were confirmed in memory, attention, affective domain, and language. Similar results were reported in articles by Manzitti J [5], Ruiz Orosco H [7], and others who addressed this topic [13- 18]. 80.0% of the children required ophthalmological treatment, 90.0% required support for neurocognitive and psychological issues, and 18.6% were seen by other medical specialties. Follow- up care showed stability and improvement in their sequelae.
Phase III Comprehensive Health Care Model for Pediatric Patients Screened in the Retinopathy of Prematurity Program
The care model is conceptually based on health systems that follow the Primary Health Care (PHC) strategy and the Chronic Disease Care Model for children and adolescents [10,18,19]. It places PHC as the integrating framework in public health policy delivery and gives it a central role in intersectoral collaboration. In Cuba, there is a comprehensive strategy for the management of patients with non-communicable chronic diseases that includes both promotion and prevention [20-23].

Source: Ophthalmologic examination.
The consolidation of experiences from clinical ophthalmology services, awareness of the current national health situation, the country’s social, political, and economic reality, and the structural and functional characteristics of Cuba’s health system, together with legal, bioethical, political, and strategic health guidelines, form the foundation for shaping an integrated ophthalmological health care model for children screened in the ROP program. This contributes to appropriate social integration and improved quality of life for these pediatric patients in Villa Clara province.
Model Characteristics
• Functional: Simple, practical, and human-centered. It
incorporates and enhances existing programs.
• Multidisciplinary and Intersectoral Approach: Based
on coordinated action among health and education professionals.
• Care Flowchart: Includes a clear structure of roles, steps
in the care process, patient journey, and integration between PHC
and hospital services.
General Objective
• To establish guidelines to reorganize health services and improve the quality of comprehensive care for premature children in the ROP program.
Specific Objectives
• Ensure that the basic care needs of premature pediatric
patients in the ROP program are met, promoting satisfaction and
quality of life.
• Empower patients with knowledge about their condition,
personal health goals, and self-care practices.
• Promote foundational training and research on the care
of premature pediatric patients in the ROP program to improve
services for patients and their families.
• Systematically evaluate the development and quality of
the model’s implementation.
Model Principles
• Fundamental rights of the child
• Child-centered care
• Comprehensiveness of care
• Continuity of care
Model Components
• Clinical-functional care process
• Professional development / research and publication
• Information system
• Monitoring and evaluation
Stages of the Model
• Stage I: Care for children aged 0 to 6 years
• Stage II: Care for children aged 6 to 12 years
• Stage III: Care for adolescents aged 13 to 18 years
Each participant in the system has a specific role at every stage, including PHC physicians (MGI), ophthalmologists, psychologists, other specialists, parents, children, adolescents, the Ministry of Education (MINED), and social workers. Comprehensive Health Care Model for Pediatric Patients Screened in the Retinopathy of Prematurity Program (Figure 2).
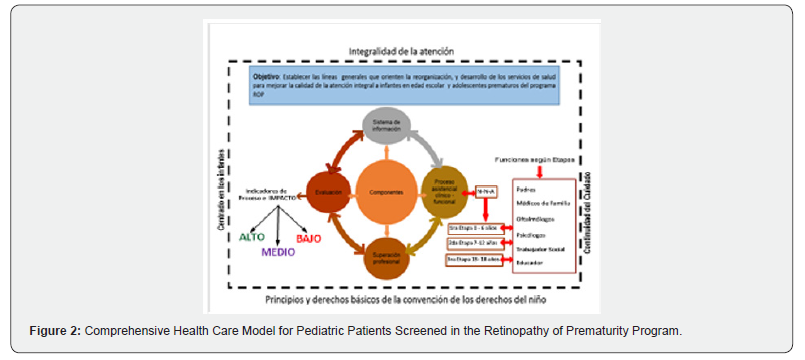
Conclusions
The comprehensive health care model for pediatric patients screened in the Retinopathy of Prematurity program positions Primary Health Care (PHC) as an integrative framework in the delivery of public health policies and in the care model for chronic diseases in children and adolescents. It adopts a multidisciplinary and intersectoral approach that encompasses both health promotion and disease prevention. The model proposal was evaluated by expert consensus and was considered highly appropriate.
References
- Milián Espinosa I, Cairo Gonzáles V, Silverio Negrín M, Benavides Casals ME, Pentón Cortes R, et al. (2023) Epidemiology of Spontaneous Preterm Birth. Acta Méd Centro 13(1).
- Valdés Armenteros R, Ruiz Tellechea Y, Morilla Guzmán A, et al. (2016) High-Risk Newborn. In: Neonatology. Diagnosis and Treatment. 2nd Havana: Editorial Ciencias Médicas p: 35-71.
- Martínez-Lemus O, Pérez-González J, Toledo-González Y (2022) Factors Associated with Retinopathy of Prematurity in Very Low Birth Weight Neonates (2016-2020). Rev cubana Med Int Emerg
- Rodríguez M, Esther Caridad Díaz Guzmán, Matilde Landín Sorí, Mayra Mier de Armas (2017) Retinopathy of Prematurity in Sancti Spíritus: Epidemiology and Clinical Characteristics. Rev cubana Oftalmol.
- Parag K Shah, Vishma Prabhu, Smita S Karandikar, Ratnesh Ranjan, Venkatapathy Narendran, et al. (2015) Retinopathy of Prematurity: Past, Present, and Future. World J Clin Pediatr 5(1): 35-46.
- National Library of Medicine (2022) Retinopathy of Prematurity. MedlinePlus.
- Ruiz Orozco H, et al. (2013) Retinopathy of Prematurity. México: Grupo ROP.
- Mier Armas M, et al. (2023) Preliminary Report on the Cuban Program to Prevent Childhood Blindness from ROP. Visión Panamericana.
- Fariñas Falcón Z, et al. (2014) Results of the ROP Program in Villa Clara Province. Acta Méd Centro.
- Minué S, Fernández C (2018) Critical Perspective and Argumentation on Chronic Care Programs in Primary and Community Care. Aten Primaria 50(2): 114-129.
- Fustamante-Sánchez V, et al. (2017) ROP and Its Evolution in Low-Birth-Weight Neonates Discharged from NICU. Rev Cuerpo Mé
- Carrer de Cirilo A (2015) Premature Children Have More Visual Defects.
- Magán Maganto MC (2021) Neuropsychological Characteristics and Neurodevelopmental Disorders in Premature Children [thesis]. Spain: University of Salamanca.
- Dýrleif Pétursdóttir, Gerd Holmström, Eva Larsson, Birgitta Böhm (2021) Visual-Motor Functions are Affected in Young Adults Born Premature. Acta Paediatr 110(1): 127-133.
- Pérez-Jara C, Ruíz Y (2022) Neuropsychological Evaluation in Children with Neurodevelopmental Disorders. Rev Méd Clínica Las Condes 33(5): 502-511.
- Hernández Monroy R (2020) Bayley III Neurodevelopment Assessment and Risk Factors in a Premature Cohort [thesis]. Mexico: Universidad Autónoma de Nuevo Leó
- Leticia Alcántara-Canabal, Cristina Fernández-Baizán, Gonzalo Solís-Sánchez, Jorge L Arias, Marta Méndez (2020) Behavioral and Emotional Issues in Premature Children in Primary Care. Aten Primaria 52(2): 104-111.
- Pereira-Cerro AV, et al. (2020) Psychomotor Development in Preschoolers with Prematurity History. Anales de Pediatrí
- Helbert Orlando Arévalo Roa, Natalia Guarín Téllez (2022) The model of care as the cornerstone of the health outcomes of chronic patients. Rev Colombiana de Reumatología 29(3): 155-156.
- Giraldo ADJF (2020) Configurations and Health Models Based on Primary Care in 21st-Century Latin America: A Narrative Review. Gerencia y Políticas de Salud 19.
- Figueras-Roca M, et al. (2020) Integration of Primary Ophthalmology into Hospital Settings: Comparative Analysis. Atención Primaria.
- Del Campo RR, Iturbe AG (2022) Reflections on 21st Century Primary Care. Atención Primaria Prá
- Pernía A, et al. (2022) Tensions in Health Care Models for Patients with Risk Factors for Chronic Diseases. Glob Health Promot.






























