Abstract
The primary factors leading to vision issues among the adult population are Diabetic retinopathy (DR) and age-related macular degeneration (AMD) including cataracts. Age-related macular degeneration (AMD) is responsible for nearly half of the cases of blindness in people older than 40 years. The prevalence of age-related macular degeneration (AMD) in India ranges from 1.2% to 4.7% among adults over 40 years of age, with a median estimation of 3% about 15.3 million Indians suffer from some form AMD in 2025. Globally the projected number of people with AMD is 225 million in 2025 and will rise to 288 million in 2040. There are two main types of AMD: dry AMD and wet AMD. Dry AMD is the more common form (80-85%), where the macula thins out with age. Wet AMD is about 15-20% and is a more serious form, characterized by the growth of abnormal blood vessels in the macula. In early AMD, vision changes like blurred vision, decreased contrast sensitivity, and impaired dark adaptation are mild or absent, whereas late AMD presents with distortion of images, central scotomas, and loss of central vision. AMD does not cause complete blindness, but it affects central vision, making it difficult to see faces, read, or perform close-up tasks. As AMD develops slowly, early vision loss is not noticed. Regular eye exams are the best way out, for individuals over 40, to monitor signs of AMD. Early detection of AMD is crucial for preventing further vision loss. The most important nonmodifiable risk factors are advancing age, blue iris, & genetic mutations, as genetics account for 71% of the risk of developing the disorder. Modifiable risk factors include smoking, hypertension, diabetes and diet. Treatment for dry AMD focuses on managing vision loss with low vision aids and lifestyle modifications. Treatment for wet AMD include injections of anti-VEGF drugs into the eye to reduce swelling and prevent bleeding, laser treatments, and advanced surgical options.
Materials & Methods: February 2025 was observed as AMD awareness month, as each year. This article is a dedication to AMD awareness month based on managing two cases with clinical manifestations and a recent small eye checkup camp which identified 20 AMD cases, in 95 elderly individuals, and supported by requisite literature search.
ularly in resource-limited settings. This approach could potentially improve patient outcomes by facilitating early investigations and referrals.
Keywords: Age-Related Macular Degeneration; Anti-Vascular Endothelial Growth Factor; Medications; Intravitreal Injections; Neovascular Age-Related Macular Degeneration; Wet AMD; Dry AMD
Abbreviations: AMD: Age-Related Macular Degeneration; Anti-VEGF: Anti-Vascular Endothelial Growth Factor; IVI: Intravitreal Injections; DAMD: Dry AMD; CNV: Choroidal Neovascularization; DR: Diabetic Retinopathy; MNV: Macular Neovascularization; AAO: American Academy of Ophthalmology; VEGF: Vascular Endothelial Growth Factor
Introduction
The primary factors leading to vision issues among the adult population are Diabetic (DR) retinopathy and age-related macular degeneration (AMD) including cataracts. Age-related macular degeneration (AMD) is responsible for nearly half of the cases of blindness in people older than 40 years. February each year is observed as AMD awareness month. Nearly 20 million Americans aged 40+ have been diagnosed with some form of macular degeneration & 1.49 million Americans are living with a late-stage vision-threatening form of it. By the age of 75, roughly 1 in 3 people living in the US will have some form of AMD, and 25% of them will have a vision-threatening, late-stage form of AMD [1]. According to data provided by 2 international bodies, cases of near vision loss have more than doubled in India to 137.6 million in 2020 as compared to 57.7 million in 1990 [2]. With an estimated midyear population of 1.46 billion, India has about 35% over the age 40 years from about 511 million. The prevalence of age-related macular degeneration (AMD) in India ranges from 1.2% to 4.7% among adults over 40 years of age. With a medianestimation of 3% about 15.3 million Indians suffer from some form AMD. By 2026, the number of people aged 60 and older is estimated to reach 180 million and with an AMD prevalence of 5% in this population we will have 9 million AMD cases in 2026. Epidemiological studies in adults (over 40 years) have shown prevalence of 2.7% - 4.3% among Indians [3]. Interestingly AMD does not cause complete blindness, it can affect central vision, making it difficult to see faces, read, or perform close-up tasks.
Intravitreal injection therapy with anti-vascular endothelial growth factor (VEGF) has progressed well in the care of the wet form of advanced AMD, or choroidal neovascularization (CNV), resulting from abnormal growth of blood vessels in the back of the eye and accounts for most cases of blindness from AMD. A study of IVI brolucizumab after it was launched in India in October 2020, demonstrated favorable visual and anatomic outcomes and safety profile for eyes with nAMD. The mean injection-free interval in eyes treated with PRN was 19 weeks. Our challenge is 80% of patients with AMD, who suffer from the dry form of the condition (DAMD), or geographical atrophy. DAMD is characterized by enlarging areas of photoreceptor & retinal pigment epithelium atrophy. Two recently approved drugs for dry AMD inhibit steps in the complement pathway & slower the growth of atrophic lesions but do not prevent loss of vision. Given the dearth of effective treatments once patients reach the late stage of the disease, advocacy for lifestyle changes early during the condition to preserve vision. This article is an outcome of managing two individual cases with clinical manifestations and a small eye checkup camp identifying 20 AMD cases, and requisite literature search.
Case Reports
Case 1:
• AMD in an elderly Male: A 65-year-old male patient came to an Ophthalmic OPD of a medical College in Gadag, Karnataka, India with complaints i) difficulty in recognizing faces, reading newspaper/book and straight lines appear distorted, ii) Diminished vision of B/L eyes iii) Photophobia iv) Difficulty in adapting to low light. Clinical Findings: All general examination findings were within normal ranges. Key diagnostic positive findings were
i. Cup-disc ratio 0.3:1, mild peripapillary atrophy on both sides,
ii. Macula Dull with drusen’s on both sides
iii. Both Fundus Reflex were absent. Diagnosis of AMD was made based on patients’ complaints i.e., Blurring of vision and distortion of central vision which was tested using Amsler’s grid & fundoscopy findings of B/L eyes showing dull macula & presence of drusen’s in the macula along with mild peripapillary atrophy. He was treated with IVI brolucizumab. Visual & anatomic outcomes were satisfactory, adverse reactions. The injection-free interval in eyes treated has been 20 weeks so far.
Case 2:
• AMD in an elderly Lady: A 79-year-old female presented with blurred vision in her left eye for the last 3 months. She gave a history of dry AMD in both eyes, hypertension for 25 years, heart disease, high cholesterol, and osteoporosis in the last 2 years. She was a survivor of lung and breast cancer, undergoing chemotherapy. A popular and dedicated eye hospital’s discharge summary read, Patient: A 79-year-old female with a history of dry AMD in both eyes. Complaint: Blurred vision in the left eye for 3 months. Ocular History: Prior history of dry AMD in both eyes, status post cataract surgery in both eyes.
• Diagnosis: She was put on the gold standard treatment of anti-VEGF therapy of Ranibizumab (Lucentis) via intravitreal injections. This drug effectively reduced abnormal blood vessel growth and fluid leakage in the retina, and stabilized vision, and was informed that there was no improvement possible
Case Report 3:
• AMD in an Apartment Complex in Bengaluru: A community-based screening of 95 subjects ≥60 years of age in an apartment complex in Bengaluru. It involved all subjects underwent a detailed history, physical examination, and a comprehensive ocular examination and 91 subjects with gradable images on 30° three-field retinal photographs were analyzed. AMD & DR were graded based on the International ARM Epidemiological Study Group classification & International Clinical Diabetic Retinopathy Disease Severity Scale, respectively. Of the 91 subjects, 65 had diabetes. Among the diabetics, 16 (25%) had Diabetic Retinopathy (DR), of which 3 had AMD. Of 26 with diabetes but no DR, 4 had AMD. The presence of DR was a protective factor for AMD in diabetics. After adjusting confounding factors, those with AMD 16 had diabetes, 12 had raised systolic blood pressure, 5 had higher BMI and 18 had higher serum triglycerides. Of the 20 cases 14 were in early stages of AMD and were advised to have a Lifestyle modification and better management of Diabetes, Hypertension and Dyslipidemia and reduction of weight. They were advised to consume fruits twice per day; and at least 200 g per vegetable per day. In addition, non-vegetarians were advised to consume fish at least twice per week and avoid more than 6 servings of red meat a week. A total of six cases were selected for Intravitreal injections (IVI) of vascular endothelial growth factor (anti VGEF) drugs. 2 cases each were given
i. brolucizumab, a newer drug
ii. Lucentis (Ranibizumab), considered a gold standard treatment and
iii. Avastin (Bevacizumab), a cost-effective option. The cases are being monitored.
Discussions
Age-related macular degeneration has become the leading cause of irreversible central vision loss in individuals older than 50 years in industrialized nations, with reported prevalence of 12.33% in Europe, 7.38% in Asia, and 7.50% in Africa. Age-related macular degeneration has been consistently found to be more prevalent among Whites than that in Blacks [1-3].
Types of AMD
There are two main types of AMD: dry AMD and wet AMD. Dry AMD is the more common form (80%), where the macula thins out with age. Wet AMD is about 20% and is a more serious form, characterized by the growth of abnormal blood vessels in the macula. Dry AMD (drusen fatty deposits within Bruch membrane, pigmentary changes, & RPE atrophy) accounts for 85%-90% of all cases. Although wet or nAMD is responsible for only 10%-15% of cases, it accounts for 90% of AMD-related blindness. As 42% of patients with nAMD in 1 eye develop neovascular membranes in the second eye within 5 years, such patients with blurred vision or distortion in the first eye should be referred promptly for periodical checkup.
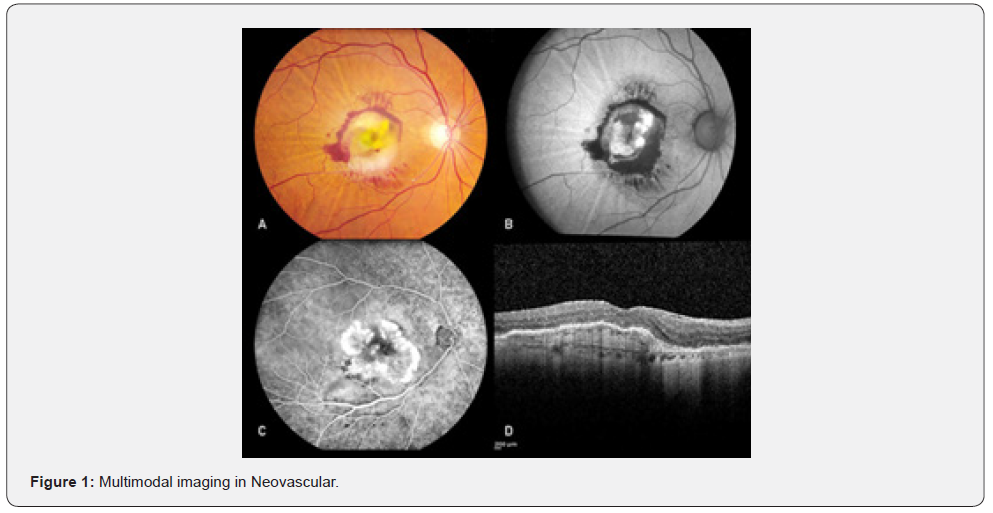
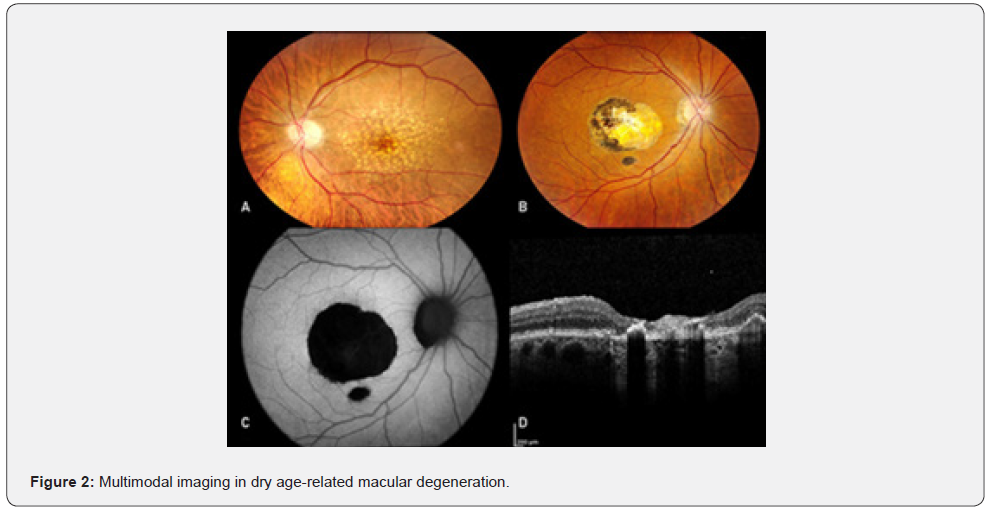
• Diagnosis: The gold standard for diagnosing AMD remains a thorough ophthalmologic examination with appropriate ancillary testing. Figures 1 and 2 show the multimodal imaging techniques used in evaluating patients with AMD. Individuals older than 55 years must undergo a dilated fundus examination to screen for macular degeneration. For patients at risk of developing advanced AMD (those with a previous diagnosis of early AMD, a strong family history, and smokers), regular monitoring of vision with an inexpensive, low-tech Amsler grid card is an easy & cost-effective way to identify progression; For patients with early & intermediate AMD, home monitoring devices can be used [1,3,4].
Pathophysiology
Age-related macular degeneration is a multifactorial disease, the etiology of which is not completely understood, but RPE dysfunction due to oxidative stress, lipid metabolism, inflammation, and complement activation is believed to play a crucial role. The elevated metabolic rate and high oxygen consumption of the macula puts this tissue in a state of chronic oxidative stress. The continuous uptake and degradation of shed photoreceptor outer segments by the adjacent, aging RPE cells cause lipofuscin to accumulate beneath the retina, which induces cell injury, dysregulation of RPE function, and abnormal extracellular matrix deposition into Bruch membrane. Together with oxidative stress, these changes trigger inflammation that damages the RPE and compromises the outer blood-retinal barrier. Progressive damage to Bruch membrane together with the upregulation of vascular endothelial growth factor (VEGF) due to hypoxia and inflammation induces the growth of new choroidal vessels into the sub-RPE or subretinal spaces. Excessive activation of complement, present in high concentration within drusen, contributes to disease progression. Oxidative stress amplifies this response by making the RPE more susceptible to complement-associated injury. Activation of the complement cascade together with oxidative stress increase VEGF secretion by up to 100-fold, thereby inducing abnormal new vessel formation of macular neovascularization (MNV) [1].
Genetic, environmental, and metabolic factors play complex roles in the development of AMD. The most important nonmodifiable risk factors are advanced age, blue iris, & genetic mutations, Modifiable risk factors include smoking, hypertension, diabetes and diet. Smokers have a 6 times higher risk of developing dry AMD than nonsmokers. Genome-wide association studies have identified risk variants in the ARMS2, HTRA1, and PLEKHA1 genes on chromosome 10,25 the CFH Y402 H26 gene on chromosome 1, and the TIMP3 gene [1]. Age is the biggest nonmodifiable risk factor for AMD, while genetics accounts for 71% of the risk of developing the disorder. Patients need to know that certain behaviors can increase or reduce their odds both of developing AMD and slowing its progression [2,3].
1. Smoking: Smoking has long been recognized as an important contributor to the risk for AMD, with a two- to three-fold risk for advanced AMD in current smokers compared with nonsmokers. But 20 years after quitting smoking, the risk returns to that of a nonsmoker.
2. Exercise: A 2017 meta-analysis of studies examining the relationship between exercise and AMD suggested that regular physical activity could reduce the development of late disease by 40%.
3. The Role of Nutrition: Nutrition is the second-best effort after cessation of smoking in preventing AMD. Lutein and zeaxanthin are very actively concentrated in the macula of the eye. We get them from our diet of green leafy vegetables, and orange and yellow fruits and vegetables. When the eye accumulates nutrient in the retina, it is important for the organs functioning. This theory has been buttressed by two randomized trials of vitamin supplementation. The Age-Related Eye Disease Study (AREDS1), from 1992-2001, demonstrated that patients with intermediate AMD treated with vitamins C, E, and beta-carotene, along with zinc, showed a 25% decrease in the risk of progressing to late AMD after 6 years of follow-up. The AREDS2 trial replaced the beta-carotene component with lutein and zeaxanthin to remove the risk for lung cancer while still protecting against progression from intermediate to advanced AMD, and the AREDS2 vitamins have become the standard of care for patients with intermediate forms of the disease.
Diet is a good preventive effort before AMD progresses to its intermediate stage:
“The Mediterranean diet, the anti-inflammatory diet pattern, or low glycemic diets are all strongly associated with reduced risk of disease. Research has found adherence to a Mediterranean diet can reduce the risk for progression from early to intermediate AMD by 21%, while also lowering the risk for the dry form of late AMD by nearly 30% [5]. The main protective drivers were consuming fish at least twice per week; fruits twice per day; and at least 200 g per day of vegetables. The consumption of six to sevenservings of red meat a week for women and nine or more servings a week for men was found to be harmful [5]. Dietary changes and supplements are complementary. Supplements are mostly helpful in decreasing the risk of developing wet AMD, whereas eating fish, fruits, and vegetables can prevent progression to advanced disease from geographical atrophy. For patients who have a family history of AMD, diet can largely overcome their genetic risk.
Screening Gaps
The American Academy of Ophthalmology (AAO) recommends a formal eye exam, which includes a dilated slit lamp exam, starting at age 40 years even in people without any loss of visual acuity. Because the risk for cataracts, glaucoma, and AMD rises with age, patients should visit an ophthalmologist or optometrist more frequently as they age (Table 1) [2].

Clinical Features and Staging
Age-related macular degeneration is usually classified into early and late stages by clinicians, whereas clinical trials frequently use the Age-Related Eye Diseases Study (AREDS) severity scale [1]. In early AMD, vision changes are absent or mild (blurred vision, decreased contrast sensitivity, and impaired dark adaptation), whereas late AMD presents with distortion of images (metamorphopsia), central scotomas, and loss of central vision.
Early AMD: Early AMD is often asymptomatic, but some individuals may notice mild central distortion and difficulty in reading in low light. Drusen, small yellowish deposits composed of lipids and proteins that are situated between the RPE and Bruch membrane, are the first visible signs and are the clinical hallmark of AMD. Both the size and number of drusen contribute to the risk of AMD progression. Drusen often progress over time, sometimes followed by more severe forms of AMD and loss of central vision. The AREDS found that specific combinations of vitamins slow progression of drusen to advanced AMD in 25% of patients.
Intermediate AMD: Intermediate AMD is defined as any medium-sized drusen or 1 large drusen and/or GA of the RPE not involving the center of macula that may cause mild metamorphopsia. The 5-year risk of progression from intermediate to advanced AMD is approximately 18% [1].
Advanced AMD:
Neovascular AMD: Neovascular AMD, the common form of advanced AMD, occurs when new choroidal or retinal blood vessels grow into the sub-RPE & subretinal spaces. The resultant fluid, hemorrhage, lipid exudates, or detachment of the RPE, if untreated, lead to irreversible, severe vision loss & fibrovascular scarring sometimes with outer retinal atrophy.
Geographic Atrophy: Geographic atrophy, the advanced form of dry AMD, is characterized by loss of RPE, photoreceptors, and choriocapillaris. Progression of atrophy often leads to progressive, permanent loss of central vision, although this loss occurs more slowly than that experienced by patients with nAMD. In fact, sudden loss of vision in a patient with GA should raise the suspicion of newly developed neovascularization and should prompt a referral.
Role of Primary Care Physicians: Primary care clinicians also can educate patients with a family history about the early warning signs of AMD, such as difficulty performing tasks under low light conditions, visual distortion, or symptoms of blurred vision or difficulty focusing, which are red flags indicating need for a referral to an eye specialist. “The low hanging fruit is healthy diet and active lifestyle, and those overlap with so many other benefits. Taking supplements and going for regular dilated slit lamp exams are mandatory for patients who have progressed to intermediate AMD. Regular Amsler grid testing is the most important for all who have intermediate AMD or more advanced AMD in one eye, as it can identify early changes in the good eye, to catch wet macular degeneration, as soon as possible because the treatment is very effective at halting progression. Patients undergoing should be reminded of the importance of adhering to a regular regimen. “Monthly treatments with anti-VEGF drugs does not cure, therefore it should not be disrupted as they can lose ground and can’t regain. Helping patients avoid late AM & the need for intravitreal injections should be the goal. If they have low levels of macular pigment related to poor diet or some type of malabsorption syndrome, putting them on supplements and looking forward to seeing them at follow-up is the right approach as a lot of their symptoms improve.
AMD burden and Situation in India: The prevalence of age-related macular degeneration (AMD) in India ranges from 1.2% to 4.7% among adults over 40 years of age. While the prevalence is lower in West India (1.4%) and highest in South India (3.1%). This makes AMD a significant cause of vision loss globally, including in India. While AMD does not typically cause complete blindness, it can affect central vision, making it difficult to see faces, read, or perform close-up tasks. The presence of diabetic retinopathy (DR) and higher serum HDL are protective factors whereas obesity and higher systolic blood pressure are risk factors for AMD in subjects with diabetes [1,4-7].
Prevalence and Risk Factors: AMD prevalence increases with age, with the highest prevalence observed above 80 years of age. Studies have found that urban areas and metropolitan regions have a higher prevalence of AMD, mainly attributable to diagnostic facilities. Diabetes, higher systolic blood pressure, and higher BMI are associated with AMD in South India [6-8]. In a retrospective study of the 608,171 patients over the age of 60 attended a tertiary care eye clinic, 1.68% of subjects had a diagnosis of AMD (N = 10,217) with 45%. of them were diagnosed to have dry AMD. Cataract surgery was associated with the higher risk of AMD (OR = 1.20). Cataract, glaucoma, and diabetic retinopathy were associated with lower risk of AMD. Surprisingly smoking was not associated with AMD in the Indian population. Cataract surgery was associated with higher prevalence of AMD [6].
The community-based prevalence of age-related macular degeneration (AMD) in India ranges from 1.4% to 3.1%. Studies indicate that AMD is more prevalent in older age groups, with a higher prevalence in rural areas compared to urban areas and in females compared to males. Age and socioeconomic status are significant factors influencing AMD prevalence. A community-based survey of 5495 subjects ≥ 60 years of age in south India, after all subjects underwent a detailed history, physical examination, and a comprehensive ocular examination 4791 subjects with gradable images on 30° three-field retinal photographs were analyzed. AMD & diabetic retinopathy were graded based on the International ARM Epidemiological Study Group classification & International Clinical Diabetic Retinopathy Disease Severity Scale, respectively. Of the 4791 subjects, 1256 had diabetes. Among the diabetics, 166 (13.2%) had Diabetic Retinopathy (DR), of which 9.6% had AMD. Of those with diabetes but no DR, 15.6% had AMD. The presence of DR (OR=0.57) was a protective factor for AMD in diabetes. When adjusted for potential confounding factors, those with AMD and diabetes were from urban areas (OR=1.65, P=0.018), had raised systolic blood pressure (OR=1.02, P=0.01), higher BMI (OR=1.06, P=0.005), and higher serum triglycerides (OR=1.00, P=0.011). A higher level of high-density lipoprotein (HDL- OR=0.98, P=0.038) was a protective factor for AMD in subjects with diabetes [7]. Another study by Central India Eye and Medical Study conducted in rural central India included 4,711 subjects (aged ,30 years).
Photographs of Fundus were available for 4,542 subjects. In subjects aged ,40, ,50, and ,60 years, prevalence of early AMD was 6.1 ± 0.4%, 8.2 ± 0.6% and 8.3 ± 0.8% respectively, Late AMD was 0.2 ± 0.8%, 0.2 ± 0.1%, and 0.6 ± 0.2% respectively at 95% confidence interval. The prevalence of early AMD increased from 1.3 ± 0.3% per subject in the 30-year-old to 40-year-old group, to 3.6 ± 0.5% in the 41-year-old to 50-year-old group, to 7.9 ± 0.9% in the 51-year-old to 60-year-old group, to 10.0 ± 1.1% in the 61-year-old to 70-year-old group, to 8.3 ± 0.2% in the 71-year-old to 80-year-old group, and to 8.0 ± 5.5% in the ,81-year-old group. Age-related macular degeneration was causative for visual impairment (best-corrected visual acuity in the better eye: <20/60 and ,20/400) in 3 of 342 subjects (0.9%) and for blindness (visual acuity <20/400) in 0 of 17 subjects [8].
Early Detection and Management: Early detection of AMD is crucial for managing the condition and preventing further vision loss. As AMD develops slowly, early vision loss is not noticed. Regular eye exams are the only way out, for individuals over 40, to monitor signs of AMD.
Treatment Options: Treatment for dry AMD focuses on managing vision loss with low vision aids and lifestyle modifications. Treatment for wet AMD may include injections into the eye to reduce swelling and prevent bleeding, laser treatments, and advanced surgical options. Pegcetacoplan, sold under the brand name Syfovre™, is a new treatment approved by the FDA, given as Intravitreal injection in the eye helps slow down the worsening of geographic atrophy. A retrospective multicentric, real-world study enrolled consecutive eyes with nAMD that were treated with IVI brolucizumab after it was launched in India in October 2020 [9]. Data collected for each eye included best-corrected visual acuity (BCVA), central subfield thickness (CSFT), subretinal fluid (SRF), and intraretinal fluid (IRF) status at 6-, 12-, and 24-months follow-up. In total, 331 eyes received a mean of 3.55 ± 1.83 injections. Most frequent treatment protocol was PRN (53%). BCVA data was available for 100%, 96%, and 74% eyes at 6-, 12-, and 24-month follow-up. BCVA and CSFT improved significantly (P < 0.001) at all follow-ups. Two hundred and seventy-six (83.38%) out of 331 eyes received more than one injection; out of these, 241 (87.3%) eyes that were treated by PRN protocol could achieve mean “maximum injection-free interval” of 19.43 ± 8.82 weeks. IOI and retinal vasculitis were reported in 2.11% (7/331) and 0.60% (2/331) eyes, respectively. None of the eyes with IOI or vasculitis lost any vision at the final follow-up.
Conclusion
Nearly 200 million people throughout the world have some form of AMD. Numbers are expected to increase over the next decades. The prevalence of AMD is increasing in sync with the aging population, and the projected number of people with AMD throughout the world is 225 million in 2025 and will rise to 288 million in 2040. India has about 15 million people with some form of AMD in 2025. AMD prevalence increases with age, with the highest prevalence observed above 80 years of age. Urban areas especially metropolitan regions have a higher prevalence of AMD, mainly attributable to diagnostic facilities, and Diabetes, Systolic Hypertension, higher BMI and dyslipidemia are associated with AMD in India. Treatment for dry AMD focuses on managing vision loss with low vision aids and lifestyle modifications. Treatment for wet AMD include injections of anti-VEGF drugs into the eye to reduce swelling and prevent bleeding, laser treatments, and advanced surgical options.
References
- Nithya Boopathiraj, Isabella V Wagner, Syril K Dorairaj, Darby D Miller, Michael W Stewart (2024) Recent Updates on the Diagnosis and Management of Age-Related Macular Degeneration. Mayo Clin Proc Innov Qual Outcomes 8(4): 364-374.
- 2025 AMD & Low Vision Awareness Month Resources.
- Age-related-macular-degeneration-and-diabetic-retinopathy, progression.
- Prevalence of macular degeneration at 4.7% in people above 40 years in India.
- Ann Thomas. Can Lifestyle Change Minimize the Risk for Blindness?
- Jacqueline Hamati, Sai Prashanthi, Raja Narayanan, Niroj Sahoo, Anthony Vipin Das, et al. (2023) Prevalence of age-related macular degeneration and associated factors in Indian cohort in a tertiary care setting, Indian Journal of Ophthalmology 71(10): 3361-3366.
- S Srinivasan, G Swaminathan, V Kulothungan, S Ganesan, T Sharma, et al. () Age-related macular degeneration in a South Indian population, with and without diabetes Eye (Lond) 31(8): 1176-1183.
- Vinay Nangia, Jost B Jonas, Maithili Kulkarni, Arshia Matin (2011) Prevalence of age-related macular degeneration in rural central India. Retina 31(6): 1179-1185.
- Deependra Vikram Singh, Aniruddha Agarwal, Anubhav Goyal, Daraius Shroff, Jatinder Singh et al. (2024) Initial experience with brolucizumab for neovascular age-related macular degeneration (nAMD) in India –Singh, Indian Journal of Ophthalmology 72(12): 1786-1794.






























