Abstract
Purpose: Cataract, a leading cause of blindness globally, increases with age and caused 6.67 million disability-adjusted life years (DALYs) in 2019. High body mass index (BMI) is a known risk factor for cataracts. This study assesses the global cataract burden attributable to high BMI using GBD data.
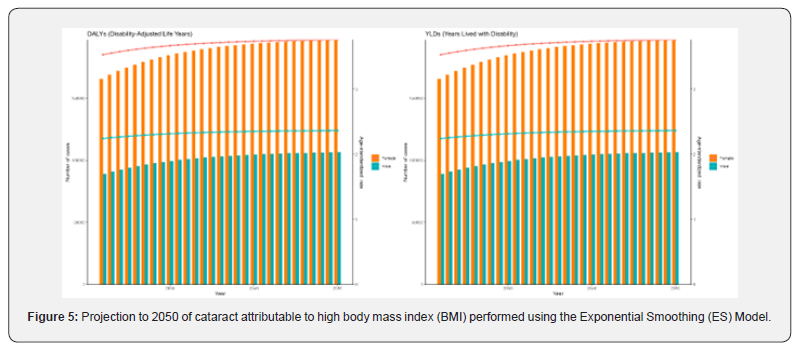
Methods: Data from the GBD 2021 was used, with statistical analysis involving age-standardized rates (ASR) to ensure comparability. The study tracked trends in DALYs and YLDs rates (ASDR and ASYR) from 1990 to 2021 using linear regression for annual percentage changes (EAPC). Projections for 2050 were made using ARIMA and Exponential Smoothing models.
Results: From 1990 to 2021, the global cataract burden attributable to high BMI steadily increased, with DALYs rising from 68,540 to 248,650. The ASDR increased from 1.84 to 2.91, reflecting a growing trend. Females had a higher ASDR than males, with both sexes showing steady rises. The burden peaked in the 95+ age group. Regionally, low-middle SDI regions had the highest ASDR, with the fastest growth occurring there. In 2021, Saudi Arabia, Oman, and Palestine had the top high ASDR. Both ARIMA and ES models predict a gradual increase in DALYs and ASDR of cataract attributable to high BMI.
Conclusions: The study highlights that elderly individual, females, regions with low and lower-middle SDI, and Asian countries like China face higher cataract burden attributable to high BMI.
Keywords: Cataract; Body Mass Index (BMI); Global Burden of Disease Study 2021 (GBD 2021); Disability-Adjusted Life Years (DALYs); Projections
Abbreviations: BMI: Body Mass Index; DALYs: Disability-Adjusted Life Years; GBD: Global Burden of Disease; YLDs: Years Lived with Disability; ASR: Age-Standardized Rate; ASDR: Age-Standardized DALYs Rate; ASYR: Age-Standardized YLDs Rate; EAPC: Estimated Annual Percentage Change; ARIMA: Autoregressive Integrated Moving Average; ES: Exponential Smoothing; SDI: Socio-Demographic Index; UI: Uncertainty Interval; YLLs: Years of Life Lost; HALE: Healthy Life Expectancy; IRB: Institutional Review Board; CI: Confidence Interval
Introduction
Globally, cataract is the leading cause of blindness [1], causing lens transparency loss, refraction changes, and increased light scattering, leading to vision impairment [2,3]. Its prevalence rises with age [4], reaching 92.6% in those ≥80 years [4]. In 2019, it caused 6,676,281 disability-adjusted life years (DALYs) globally [5]. Driven by population aging, its rise will escalate healthcare costs [6]. Currently, no authorized medications for cataracts exist [7], with phacoemulsification cataract surgery being the standard care [8,9]. Over 60% of the global population is overweight or obese [10-13], with obesity linked to cataracts [6]. A high body mass index (BMI, >25 kg/m² for those ≥20 years) [14] is a known risk factor for 13 cancers [13] and accounts for 9.69% of DALYs [15-17]. Multiple studies link cataract development to high BMI [18-21], but no prior studies have estimated its global disease burden. Our study aims to systematically assess the global disease burden of cataract attributable to high BMI, using data from the Global Burden of Disease (GBD) 2021 [22], the most comprehensive evaluation of risk factors, disability, and causes of death [23], to provide insights for future prevention measures and policies.
Methods
Data source
GBD 2021 is a comprehensive analysis of global health loss, calculating years lived with disability (YLDs), years of life lost (YLLs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases [22]. It also generates epidemiological estimates for 88 risk factors and their health outcomes [24]. For this study, we obtained DALYs and YLDs of cataract attributable to high BMI by sex, age, Socio-demographic Index (SDI) region, and country from the GBD 2021 database (available at https://vizhub.healthdata.org/gbd-results/).
Statistical analysis
In our study, age-standardized rates (ASRs) were calculated to ensure comparability between areas and across time. We used age-standardized DALYs rate (ASDR) and age-standardized YLDs rate (ASYR) to assess the burden trends of cataract attributable to high BMI from 1990 to 2021. To evaluate these trends, we calculated the estimated annual percentage change (EAPC). The formula for EAPC is as follows:
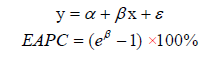
Where y is ln (ASR), x represented the calendar year and β denotes the slope determined from the linear regression of the natural logarithm of the ASR on the year [25]. Analyses were conducted using R version 4.1.0, with P < 0.05 considered statistically significant. Uncertainty intervals (UIs) for each statistic were created using the 2.5th and 97.5th percentiles of a 1000-draw distribution [26]. Projections to 2050 on the burden of cataract attributable to high BMI were performed using Autoregressive Integrated Moving Average (ARIMA) and Exponential Smoothing (ES) models. ARIMA captures patterns and seasonality in data, while ES focuses on current observations to project future trends [27].
Results
The global burden for cataract attributes to high BMI
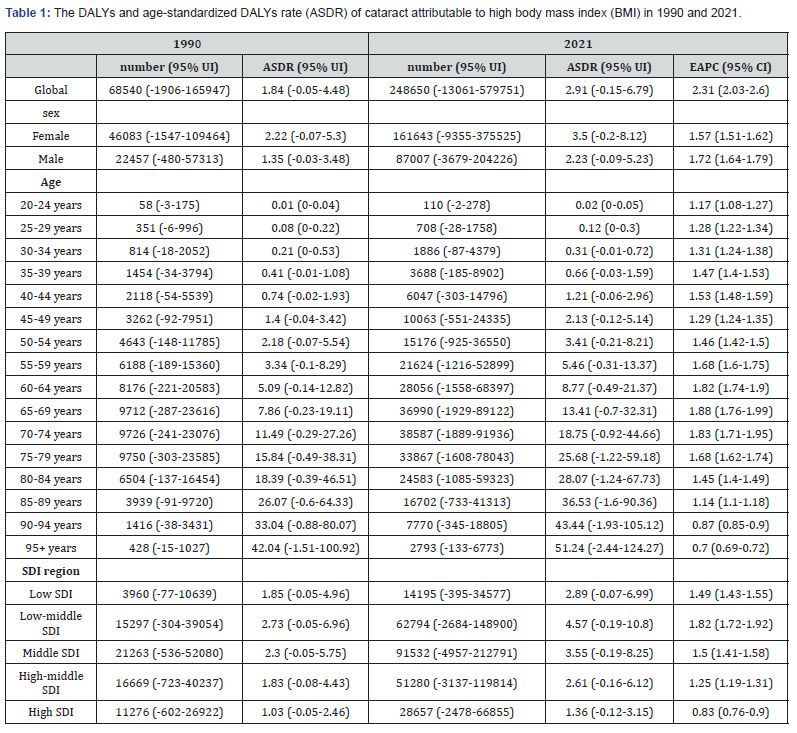
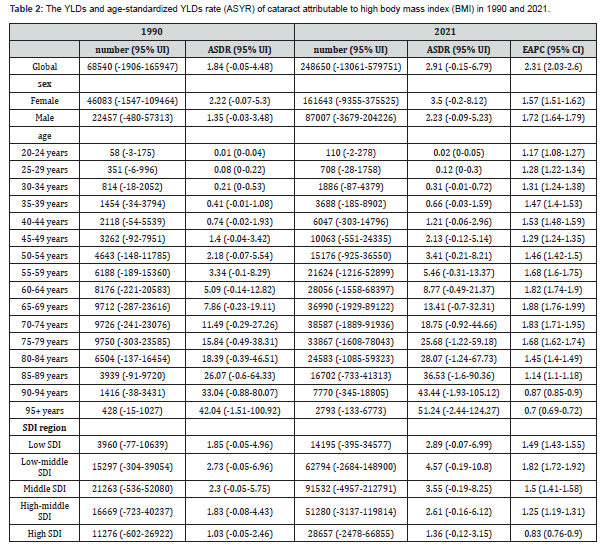
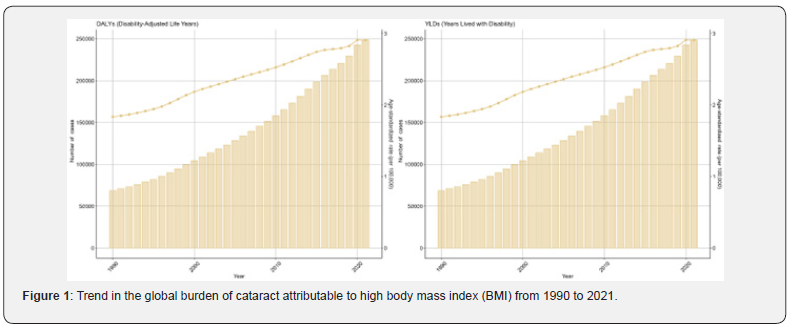
From 1990 to 2021, the DALYs of cataract attributable to high BMI increased steadily from 68540 (95% UI: -1906-165947) in 1990 to 248650 (95% UI: -13061-579751) in 2021 (Table 1 and Figure 1). The ASDR of cataract attributable to high BMI increased from 1.84 (95% UI: -0.05-4.48) in 1990 to 2.91 (95% UI: -0.15- 6.79) in 2021, with an EAPC of 2.31 (95% CI: 2.03-2.6). The pattern of ASYR is consistent with that of ASDR. The YLDs and ASYR of cataract attributable to high BMI was depicted in Table 2.
Sex-specific burden for cataract attributable to high BMI
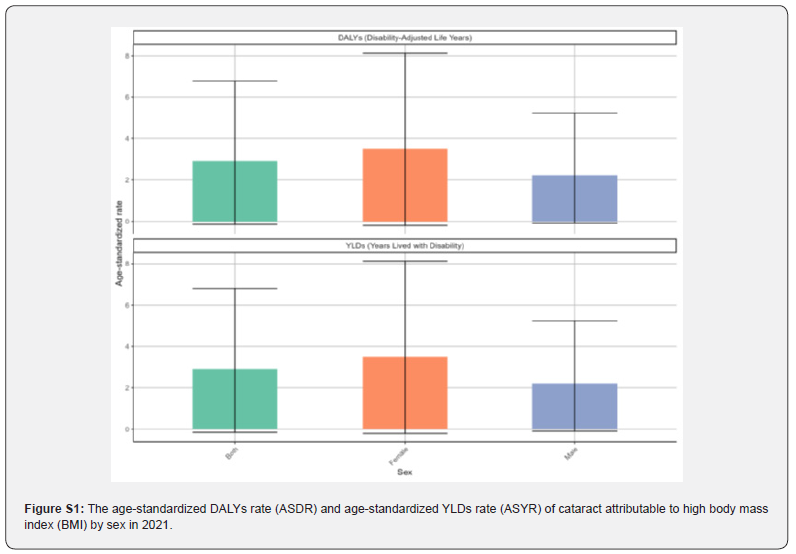
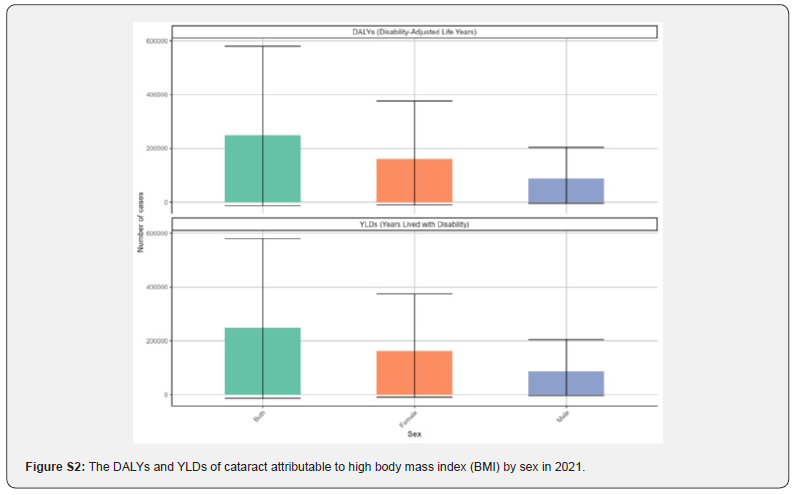
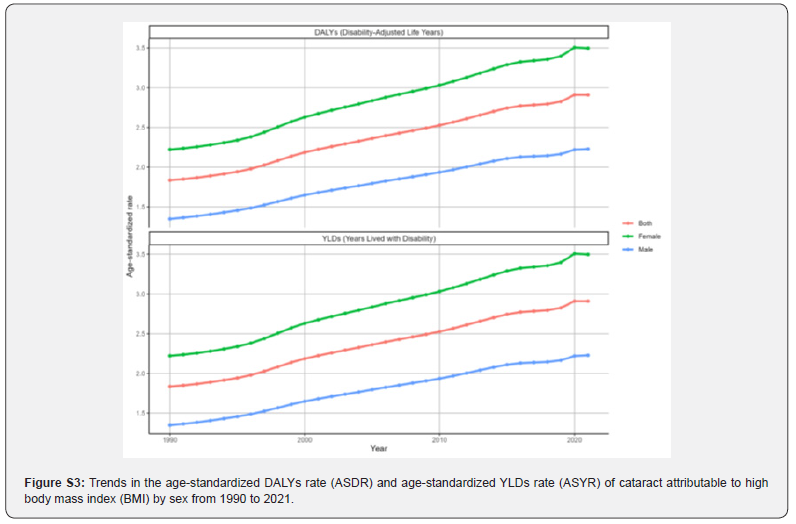
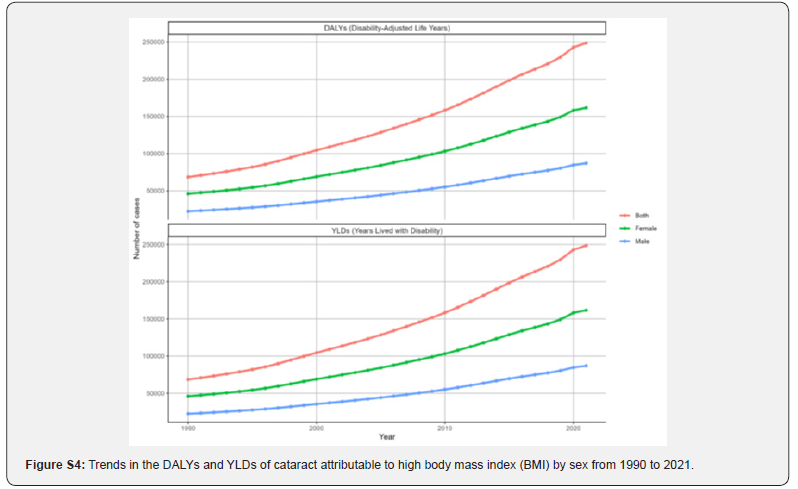
In 2021, females had a higher ASDR of cataract attributable to high BMI than males (Figure S1). The DALYs and YLDs by sex in 2021 are shown in Figure S2. From 1990 to 2021, females’ ASDR increased from 2.22 (-0.07-5.3) to 3.5 (-0.2-8.12), with an EAPC of 1.57 (1.51-1.62). Males’ ASDR also increased from 1.35 (-0.03-3.48) to 2.23 (-0.09-5.23), with an EAPC of 1.72 (1.64-1.79) (Figure S3). Trends in DALYs and YLDs by sex are depicted in Figure S4.
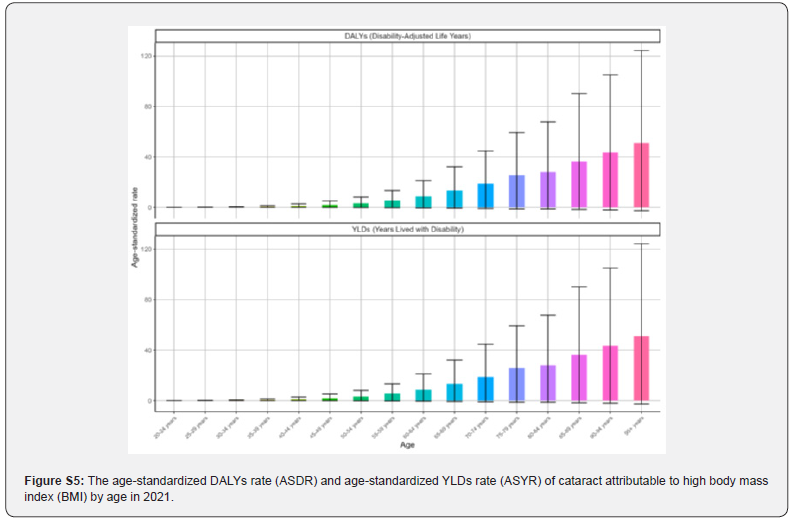
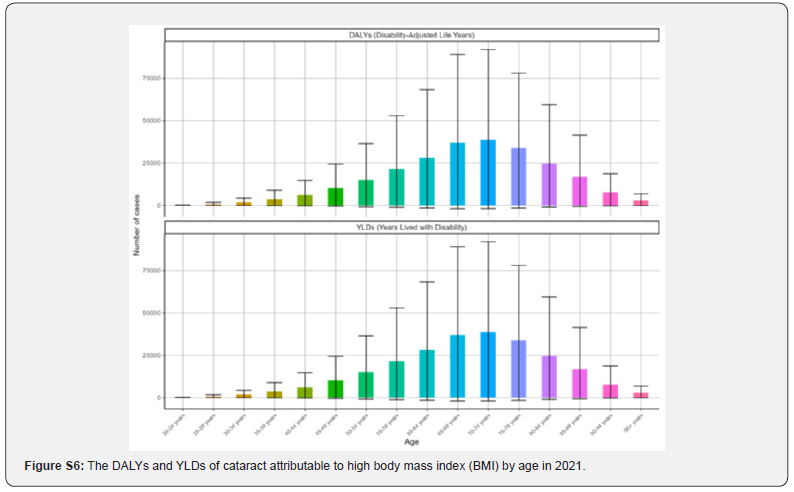
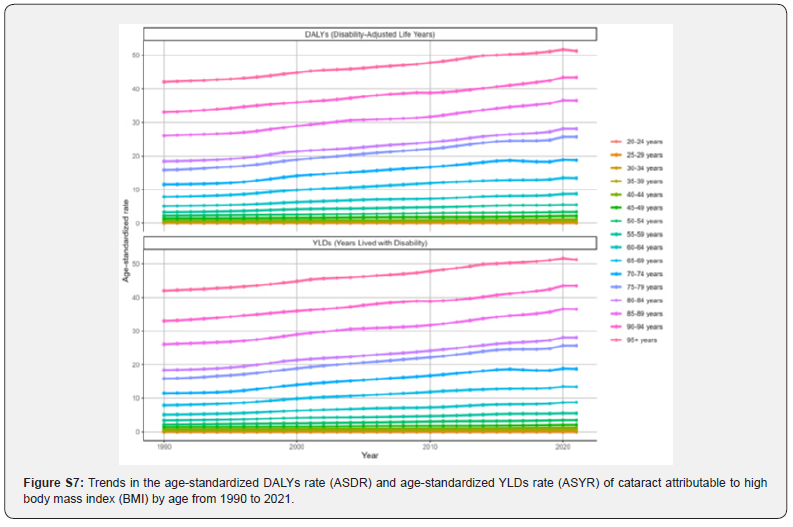
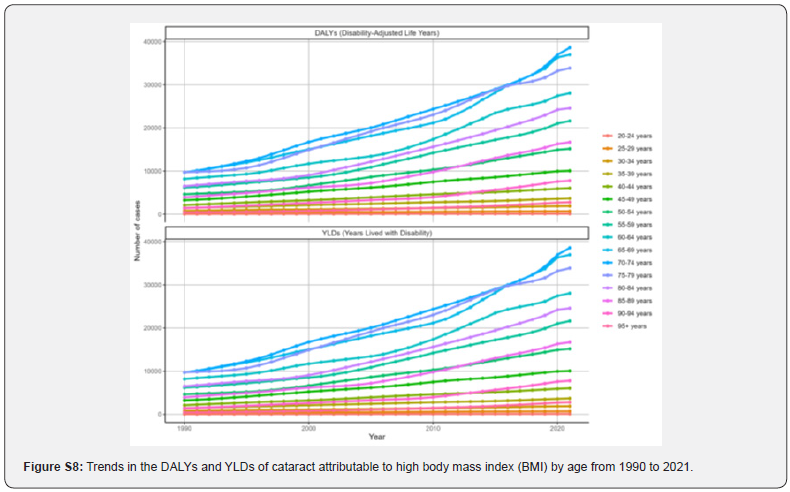
Age-specific burden for cataract attributable to high BMI
In 2021, the ASDR of cataract attributable to high BMI increased with age, peaking in the 95+ age group at 51.24 (-2.44- 124.27) (Figure S5). The DALYs and YLDs by age in 2021 are shown in Figure S6. From 1990 to 2021, ASDR increased steadily across all age groups. The largest growth occurred in the 65-69 age group, with an EAPC of 1.88 (1.76-1.99) (Figure S7). Trends in DALYs and YLDs by age are depicted in Figure S8.
Regional and national burden for cataract attributable to high BMI
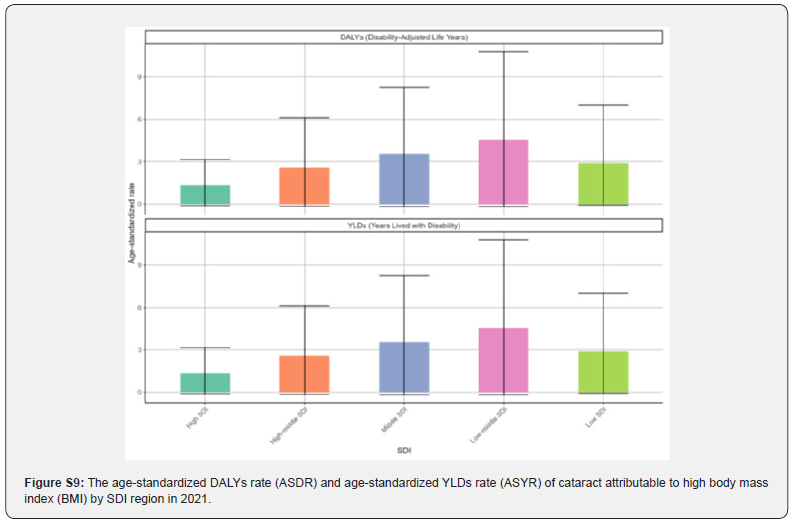
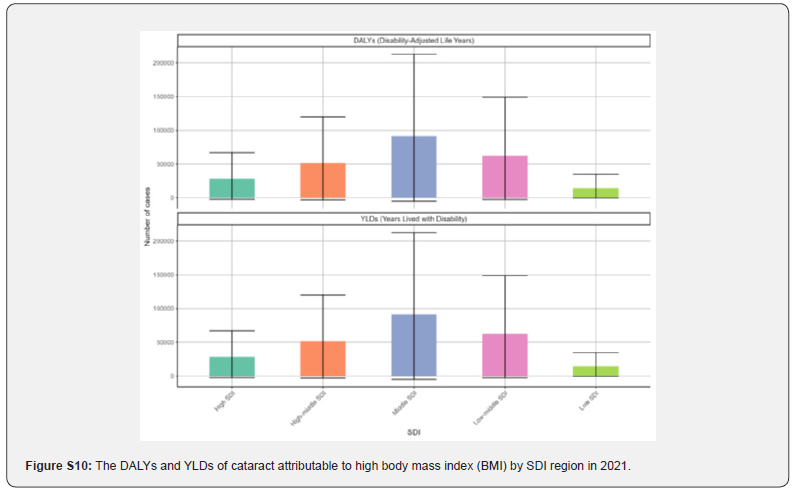
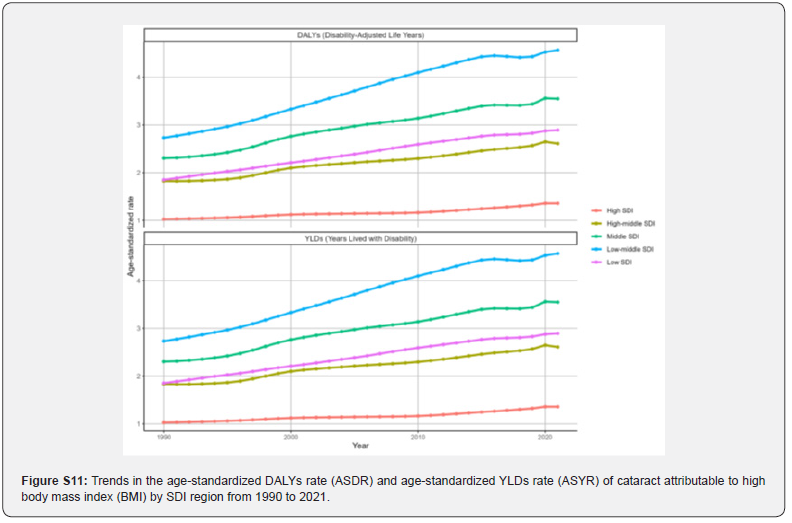
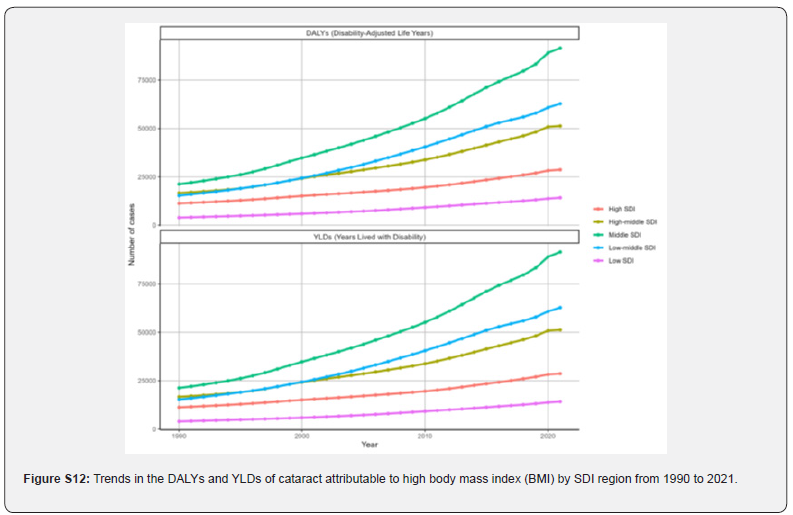
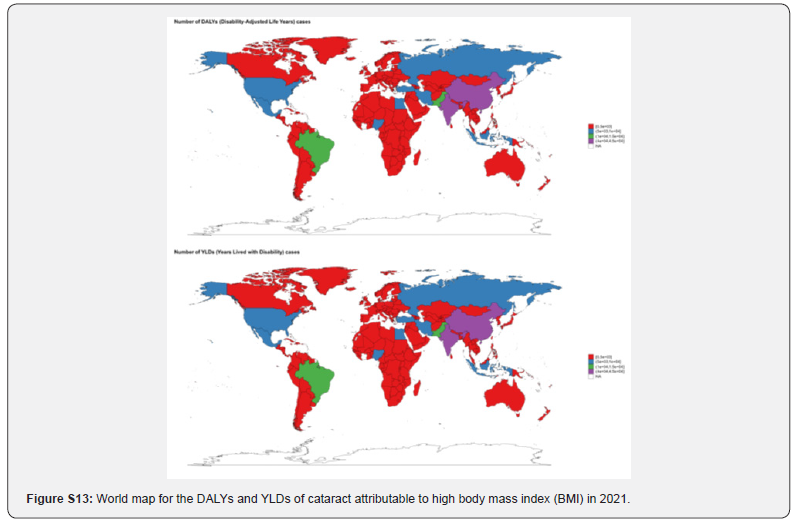
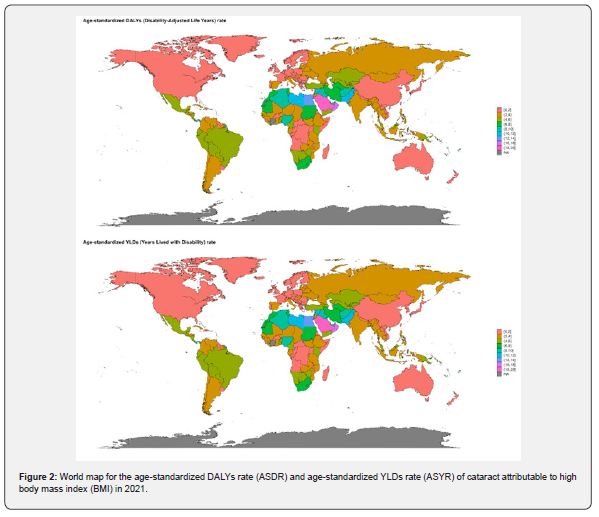
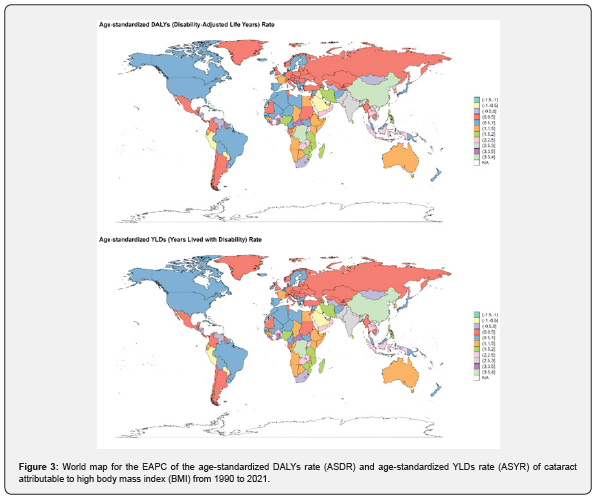
In 2021, the ASDR of cataract attributable to high BMI was highest in low-middle SDI regions (4.57, -0.19-10.8) compared to others (Figure S9). DALYs and YLDs by region are in Figure S10. From 1990 to 2021, low-middle SDI regions saw the fastest growth (EAPC 1.82, 1.72-1.92) (Figure S11). Trends in DALYs and YLDs by region are in Figure S12. In 2021, Saudi Arabia (19.38, -2.49-43.67), Oman (16.91, -1.96-38.54), and Palestine (12.7, -1.68-28.49) had the highest ASDR (Figure 2). DALYs and YLDs by country are in Figure S13. From 1990 to 2021, China (EAPC=4.94), Bangladesh (EAPC=4.91), and Taiwan (Province of China) (EAPC=4.33) saw the fastest increases (Figure 3).
Projections to 2050
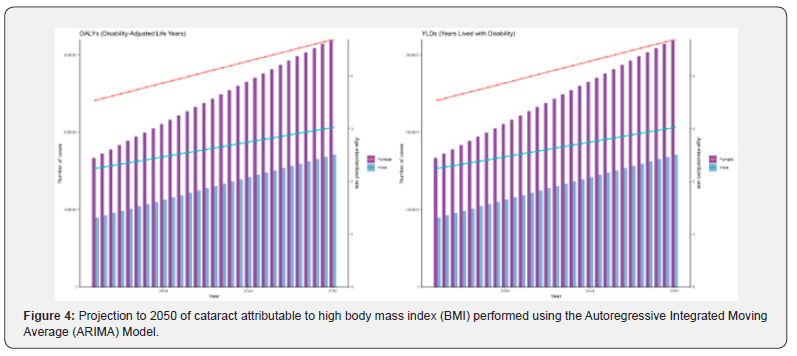
The ARIMA model predicts that from 2022 to 2050, DALYs and YLDs associated with cataract attributable to high BMI will consistently rise for both males and females, peaking in 2050 (Figure 4). The ASDR is also projected to linearly increase during this period. The ES model predicts a slightly different trend: from 2022 to 2050, the rate of increase in DALYs and YLDs due to cataract attributable to high BMI slows over time, with a similar trend observed for ASDR among both males and females (Figure 5).
Discussion
In our study, we performed a detailed stratified analysis of the current burden of cataract linked to high BMI, categorized by age, gender, region, and country. We also projected this burden through 2050. This research fills a gap in existing literature and provides updated evidence for future cataract prevention strategies and burden studies. From 1990 to 2021, DALYs and YLDs of cataract due to high BMI increased, as did the ASDR for high BMI-attributable cataracts, indicating a steady rise in the burden of high BMI-attributable cataract diseases over the past three decades, potentially becoming a significant public health issue. Several reasons underlie this: While overall ASDR for cataracts has declined [3], the ASDR for high BMI-attributable cataracts has risen, possibly due to the growing contribution of high BMI to total DALYs [14], despite global efforts to control cataracts [28]. Cataract development is often linked to aging [29,30], explaining the agerelated increase in ASDR for high BMI-attributable cataracts from 1990 to 2021, coinciding with global trends of population aging and increased life expectancy [28,31]. Our study found that from 1990 to 2021, females had a consistently higher ASDR for cataracts due to high BMI than males, indicating greater female susceptibility. This gender difference, also noted in other studies [5,32], may be due to estrogen decline post-menopause [33], longer female life expectancy [33,34], and gender inequalities in healthcare access [35,36]. Cataract surgery, the only treatment, effectively improves vision and is relatively safe [37]. However, the burden of high BMI-attributable cataracts is greater in low and low-middle SDI regions, possibly due to better surgery availability in higher SDI regions [38] and a weak correlation between ophthalmologist numbers and per capita GDP [39]. Additionally, higher cataract prevalence and earlier onset in Asian ethnicities [40] help explain the fastest increases in ASDR in Bangladesh and China from 1990 to 2021. Promoting cataract surgery awareness can benefit low-income and developing countries [41]. Both ARIMA and ES models predict a gradual increase in DALYs and ASDR for high BMI-attributable cataracts in the future, emphasizing the need for proactive prevention strategies. Early-stage interventions could be cost-effective and efficient. Our study has limitations. GBD 2021 estimates rely on modeling when data is inadequate [22], and data heterogeneity across countries due to healthcare system and data collection differences requires caution when extrapolating findings to specific regions. In conclusion, elderly individuals, females, low and lower-middle SDI regions, and Asian countries like China have a higher cataract burden due to high BMI. Addressing this burden requires considering the needs of these specific populations.
Acknowledgements
We would like to express our sincere gratitude to Wei Zhang from Tianjin eye hospital for their invaluable guidance, support, and encouragement throughout the course of this research. We are particularly thankful to Hui Song from Tianjin medical university eye hospital, who provided us with technical assistance. We would also like to acknowledge the financial support from Bengbu Science and Technology Innovation, Anhui Provincial Department of Education and Bengbu Medical University which made this work possible. Additionally, we extend our thanks to all participants and colleagues who contributed their time and effort to this study. Finally, we are deeply grateful to the editors and reviewers for their constructive comments and suggestions, which significantly improved the quality of this manuscript.
Author Contributions
Ling Yao, Meng Yue and Sijie Zhao contributed equally to the design of the study, data collection, analysis, and manuscript preparation. Yuxian Sun and Zhengyang Xu were responsible for statistical analysis and interpretation of the results. Ziqing Gao and Mingsen Li provided guidance on the methodology, interpreted the findings, and revised the manuscript critically for important intellectual content. All authors approved the final version of the manuscript and agreed to its submission for publication.
Funding Declaration
Supported by Bengbu Science and Technology Innovation Guidance Project (2024ZD0009); Key Projects of Anhui Provincial Department of Education (2023AH051963); Key Natural Science Project of Bengbu Medical College (2022byzd057); and Graduate Student’s Science and Technology Innovation Program of Bengbu Medical University (Byycx24093). The authors acknowledge the financial support provided by these institutions.
Ethics Declaration
Study using GBD 2021 data with no personal info collected. Transparent methodology, no IRB needed as no human experiments. Data used responsibly per guidelines. No conflicts of interest.
Human Ethics and Consent to Participate declarations
Human Ethics and Consent to Participate declarations: not applicable.
Data Availability Statement
The data is sourced from the publicly accessible GBD 2021 database and, following processing and analysis, adheres to transparency and reproducibility principles while complying with secondary use guidelines. It also adheres to ethical standards and sharing policies. The study promotes open science and public health collaboration. For more details, please refer to the corresponding authors.
Conflict of Interest
The authors have no conflicts of interest, as all potential areas of conflict were reviewed and deemed irrelevant. This declaration ensures transparency and credibility in the research process.
References
- Rupert R A Bourne, Gretchen A Stevens, Richard A White, Jennifer L Smith, Seth R Flaxman, et al. (2013) Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health 1(6): e339-349.
- Ruiss M, Findl O, Kronschläger M (2022) The human lens: An antioxidant-dependent tissue revealed by the role of caffeine. Ageing Res Rev 79: 101664.
- Rui Fang, Yang-Fan Yu, En-Jie Li, Ning-Xin Lv, Zhao-Chuan Liu, et al. (2022) Global, regional, national burden and gender disparity of cataract: findings from the global burden of disease study 2019. BMC Public Health 22(1): 2068.
- Liu YC, Wilkins M, Kim T, Malyugin B, Mehta JS (2017) Cataracts. Lancet 390(10094): 600-612.
- Jiang B, Wu T, Liu W, Liu G, Lu P (2023) Changing Trends in the Global Burden of Cataract Over the Past 30 Years: Retrospective Data Analysis of the Global Burden of Disease Study 2019. JMIR Public Health Surveill 9: e47349.
- Ang MJ, Afshari NA (2021) Cataract and systemic disease: A review. Clin Exp Ophthalmol 49(2): 118-127.
- Segewkal H Heruye, Leonce N Maffofou Nkenyi, Neetu U Singh, Dariush Yalzadeh, Kalu K Ngele, et al. (2020) Current Trends in the Pharmacotherapy of Cataracts. Pharmaceuticals (Basel) 13(1): 15.
- Cedric Schweitzer, Antoine Brezin, Beatrice Cochener, Dominique Monnet, Christine Germain, et al. (2020) Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): a multicentre participant-masked randomised superiority and cost-effectiveness trial. Lancet 395(10219): 212-224.
- Narayan A, Evans JR, O'Brart D, Bunce C, Gore DM, et al. (2023) Laser-assisted cataract surgery versus standard ultrasound phacoemulsification cataract surgery. Cochrane Database Syst Rev 6(6): Cd010735.
- NCD Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390(10113): 2627-2642.
- Safiri S, Carson-Chahhoud K, Noori M, et al. (2022) Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: results from the Global Burden of Disease Study 2019. Bmj 378: e069679.
- Guo X, Zhang Z, Yin X, QirongXu, Li F, Zhu F (2024) Global burden of ischemic stroke attributable to high body mass index in 204 countries and territories, 1990-2021. BMC Cardiovasc Disord 24(1): 584.
- Emmanouil Bouras, Dipender Gill, Verena Zuber, Neil Murphy, Niki Dimou, Krasimira Aleksandrova, et al. (2024) Identification of potential mediators of the relationship between body mass index and colorectal cancer: a Mendelian randomization analysis. Int J Epidemiol 53(3): dyae067.
- Zhou XD, Chen QF, Yang W, et al. (2024) Burden of disease attributable to high body mass index: an analysis of data from the Global Burden of Disease Study 2021. EClinicalMedicine 76: 102848.
- Jin X, Dong D, Xu Z, Sun M (2024) The global burden of colorectal cancer attributable to high body-mass index in 204 countries and territories: findings from 1990 to 2021 and predictions to 2035. Front Nutr 11: 1473851.
- Liu Y, Zhang C, Wang Q, et al. (2023) Temporal Trends in the Disease Burden of Colorectal Cancer with Its Risk Factors at the Global and National Level from 1990 to 2019, and Projections Until 2044. Clin Epidemiol 15: 55-71.
- Xing QQ, Li JM, Chen ZJ, Lin XY, You YY, et al. (2023) Global burden of common cancers attributable to metabolic risks from 1990 to 2019. Med 4(3): 168-181.e3.
- Alberti KG, Zimmet P, Shaw J (2005) The metabolic syndrome--a new worldwide definition. Lancet 366(9491): 1059-1062.
- Hiller R, Sperduto RD, Reed GF, D'Agostino RB, Wilson PW (2003) Serum lipids and age-related lens opacities: a longitudinal investigation: Framingham Studies. Ophthalmology 110(3): 578-583.
- Klein BE, Klein R, Lee KE (1997) cardiovascular disease, selected cardiovascular disease risk factors, and age-related cataracts: the Beaver Dam Eye Study. Am J Ophthalmol 123(3): 338-346.
- Kong X, Wang M, Jiang Y (2024) Global burden of atrial fibrillation attributable to high body mass index from 1990 to 2021: findings from the Global Burden of Disease Study 2021. BMC Cardiovasc Disord 24(1): 542.
- GBD 2021 Diseases and Injuries Collaborators (2024) Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440): 2133-2161.
- Global Nutrition Target Collaborators (2025) Global, regional, and national progress towards the 2030 global nutrition targets and forecasts to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 404(10471): 2543-2583.
- GBD 2021 Risk Factors Collaborators (2024) Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440): 2162-2203.
- Xie W, Li A, Zhang Y, Tan S, Luo J (2024) Global burden of stroke attributable to dietary risk factors in the GBD 2021 study. Front Nutr 11: 1494574.
- GBD 2021 Causes of Death Collaborators (2024) Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 403(10440): 2100-2132.
- Huang P, Zhang J (2025) Global leukemia burden and trends: a comprehensive analysis of temporal and spatial variations from 1990-2021 using GBD (Global Burden of Disease) data. BMC Public Health 25(1): 262.
- GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study (2021) Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 9(2): e144-e160.
- Klein BE, Klein R, Lee KE, Meuer SM (2003) Socioeconomic and lifestyle factors and the 10-year incidence of age-related cataracts. Am J Ophthalmol 136(3): 506-512.
- Klein R, Klein BE (2013) The prevalence of age-related eye diseases and visual impairment in aging: current estimates. Invest Ophthalmol Vis Sci 54(14): Orsf5-orsf13.
- Armstrong KL, Jovic M, Vo-Phuoc JL, Thorpe JG, Doolan BL (2012) The global cost of eliminating avoidable blindness. Indian J Ophthalmol 60(5): 475-480.
- Rui Fang, Pei-Lin Yue, Xue-Fei Ding, Ning-Xin Lv, Yu-Xuan Jia, et al. (2024) The burden of vision loss due to cataract in China: findings from the Global Burden of Disease Study 2019. Eye (Lond) 38(5): 885-892.
- Zetterberg M, Celojevic D (2015) Gender and cataract--the role of estrogen. Curr Eye Res 40(2): 176-190.
- Austad SN (2006) Why women live longer than men: sex differences in longevity. Gend Med 3(2):79-92.
- Courtright P, Lewallen S (2009) Why are we addressing gender issues in vision loss? Community Eye Health 22(70): 17-19.
- Misganaw Guadie Tiruneh, Eneyew Talie Fenta, Destaw Endeshaw, Habitu Birhan Eshetu, Ousman Adal, et al. (2024) Six in ten female youths in low-income East African countries had problems in accessing health care: a multilevel analysis of recent demographic and health surveys from 2016-2021. BMC Health Serv Res 24(1): 533.
- Yoo SH, Zein M (2021) Vision Restoration: Cataract Surgery and Surgical Correction of Myopia, Hyperopia, and Presbyopia. Med Clin North Am 105(3): 445-454.
- Wang W, Yan W, Müller A, He M (2017) A Global View on Output and Outcomes of Cataract Surgery With National Indices of Socioeconomic Development. Invest Ophthalmol Vis Sci 58(9): 3669-3676.
- Serge Resnikoff, Van Charles Lansingh, Lindsey Washburn, William Felch, Tina-Marie Gauthier, et al. (2020) Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update): will we meet the needs? Br J Ophthalmol 104(4): 588-592.
- Jacqueline Chua, Jia Yu Koh, Ava Grace Tan, Wanting Zhao, Ecosse Lamoureux, et al. (2015) Ancestry, Socioeconomic Status, and Age-Related Cataract in Asians: The Singapore Epidemiology of Eye Diseases Study. Ophthalmology122(11): 2169-2178.
- Lansingh VC, Carter MJ, Martens M (2007) Global cost-effectiveness of cataract surgery. Ophthalmology 114(9): 1670-1678.






























