Abstract
The purpose of this article is to describe and analyze two different ocular manifestations of acute unilateral HSV infection in a 13-year-old and a 16-year-old male patient that were referred in the emergency ophthalmologic department of Pediatric General Hospital of Pentelis during February 2025 and March 2025. This report reveals the rapid clinical aggravation of the disease that requires immediate intervention with the appropriate pharmaceutical agents and formulation of a strict monitoring protocol in order to prevent visual deterioration and emergence of sight threatening complications in this vulnerable population group. During February 2025 a 13-year-old male patient was referred to the clinic due to acute onset of pain and redness in the left eye (LE), accompanied by severe eyelid inflammation, foreign body sensation, itching, light sensitivity and blurred vision. Slit lamp examination revealed the presence of dendritic ulcer after fluorescence staining with a slight increase in intraocular pressure. No cells or reaction were noted in the A/C, therefore anti-herpetic medication was registered to the patient with Virgan gel, tb Valtrex, Idroflog collyrium and artificial tears (Thealoz duo collyrium) for symptom relief in order to exclude the diagnosis of HSV ocular infection. During March 2025, a young 16-year-old male patient was referred to the emergency department of Ophthalmology in the General Pediatric Hospital of Pentelis in Athens. A brief history intake revealed that the case’s primary symptom was a slight discomfort and blurred vision in the right eye (OD) without any other concomitant ocular manifestations. On the day of the referral, hyperemia of the same eye was reported as well as systemic symptoms of dizziness, gait instability and vomiting. The patients’ visual acuity measurement was recorded to be 10/10 in both eyes, with normal pupillary reflexes bilaterally and absence of retinal pathology in fundoscopic examination (normal posterior pole in the right and left eye). The patient reported absence of comorbidities and free ophthalmic and hereditary medical history.
Keywords: HSV keratitis; Dendritic Corneal Ulcer; Slit-Lamp Examination; Intraocular Pressure; Visual Acuity
Abbreviations:LE: left Eye; HSV: Herpes Simplex Virus; VZV: Varicella-Zoster Virus; CMV: Cytomegalovirus; VEGF: Vascular Endothelial Growth Factors; POAG: Primary Open Angle Glaucoma; PACG: Primary Angle Closure Glaucoma; KPs: Keratic Precipitates; PAS: Peripheral Anterior Synechiae
Introduction
The Herpes simplex virus (HSV-1) constitutes the most usual infectious cause of corneal ulcer development and keratitis in developed countries. The most prominent symptoms are mild to moderate discomfort, redness, photophobia, watering and blurred vision. Topical steroid therapy should be avoided in these cases as it can promote gradual enlargement of the corneal ulcer and evolution to a geographical or “amoeboid” configuration. A mild residual subepithelial haze is typical and can be present for weeks after the epithelium heals. Reduced corneal sensation, mild anterior chamber inflammation, follicular conjunctivitis and elevated IOP are not uncommon. Differential diagnosis of dendritic ulceration includes herpes zoster keratitis, acanthamoeba keratitis, epithelial rejection in a corneal graft, tyrosinaemia type 2, the epithelial effects of soft contact lenses and toxic keratopathy secondary to topical medication. Treatment of HSV disease is predominantly with nucleoside analogues that disrupt viral DNA. The majority of dendritic ulcers will eventually heal spontaneously without treatment, though scarring and vascularization may still remain. The most frequently used topical drugs are acyclovir 3% ointment or ganciclovir 0.15% gel, each administered five times daily. It has been proven that 99% of ulcers heal within 2 weeks after administration of these agents. Debridement where the corneal epithelium surface is removed 2 mm beyond the edge of the ulcer is an effective solution in resistant cases. Oral antiviral therapy (e.g., acyclovir 200-400 mg five times a day for 5-10 days, famciclovir or valaciclovir) is indicated in immunodeficient patients, in children and cases with marked ocular surface disease. Oral agents constitute an alternative regimen to topical treatment when the latter is poorly tolerated or in case of resistance development. Cycloplegia once or twice daily can be administered to contribute in the reduction of ocular discomfort. Prostaglandin derivatives should not be used for IOP control, since these drops can promote herpes virus activity. Application of topical steroids should be avoided in epithelial herpes keratitis (unless significant disciform keratitis is present), because they can aggravate ulceration and lead to corneal perforation. In especially refractory cases, a combination of two topical agents with oral valaciclovir or famciclovir may be effective. A non-negligeable minority of resistant cases are due to varicella-zoster virus (VZV) infection [1].
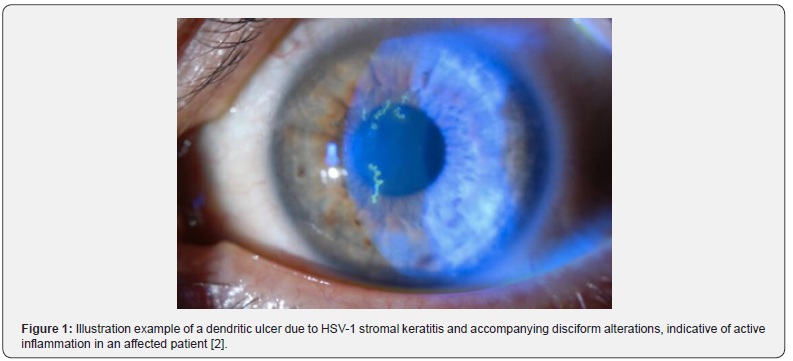
HSV-1 infection can manifest as dendritic, stromal or disciform keratitis. The risk of recurrence increases by factors such as prior herpes simplex virus keratitis, stress and sunlight exposure. Severe complications include corneal scarring, glaucoma, cataract, vision detriment and blindness in the final stage of the disease [2].
The second case constitutes a rare manifestation that resembles Posner- Schlossman syndrome and is characterized by rapid increase of intraocular pressure-IOP (glaucomatocyclitic crisis) in one eye that is accompanied by significant inflammation of the anterior chamber. Progression of the disease, misdiagnosis and delayed management can lead to non-reversible complications in the posterior pole such as glaucomatous optic nerve atrophy. It usually involves recurrent episodes of acute non granulomatous anterior uveitis with an increase of IOP unilaterally. These episodes can lead to secondary chronic glaucoma. The clinical course of the disease tends to exhibit a variable pattern; however, the condition usually follows a selflimiting course, and a spontaneous resolution of the disease is noted within days or weeks. Nevertheless, prompt management of the condition is imperative to avoid vision loss and minimize the risk of complications. The most likely infectious agents involved in the etiology of PSS are cytomegalovirus (CMV), varicella-zoster virus (VZV) and herpes simplex virus (HSV). Males are more likely to be affected, with a noticed prevalence of the disease during the age-group 20-50 years. Conditions that should be included in the differential diagnosis are acute and chronic ACG (acute close angle glaucoma), ocular hypertension, POAG (primary open angle glaucoma), Uveitic glaucoma, Iridocyclitis with trabeculitis, neovascular glaucoma, steroid induced glaucoma and other viral uveitis [3].
The treatment of this entity is directed towards controlling intraocular pressure and reducing inflammation. First line treatment includes administration of topical beta-blockers such as timolol, alpha agonists such as brimonidine and carbonic anhydrase inhibitors such as dorzolamide. Apraclonidine has also been advocated as a first line agent. Patients should be frequently monitored (daily measurements of IOP) and then on a weekly basis during tapering of antiglaucoma drops and topical steroids [3]. PSS is considered a benign disease (good long-term prognosis) as most patients are treated for attacks and recover without any residual sequelae [3].
A possible pathophysiological mechanism responsible for the acute episodes of increased IOP is the impairment of aqueous outflow from inflammation in the anterior segment, particularly of the trabecular meshwork. Studies have reported higher levels of prostaglandin E in the aqueous humor of these patients during acute phases of IOP elevation. It has been reported in several studies an overall altered cytokine profile in PSS, with increased levels of interleukin 6 (IL-6), IL-8, MCP-1, TNF, and vascular endothelial growth factors (VEGF). A natural subsequent of elevated IOP in these eyes is reduced blood flow to the optic nerve and retina that resolves spontaneously without leaving permanent damage in most cases [4].
Case Reports
To begin with the first HSV infection case, the patient was systemically followed up (visits every 10 days in the clinic) to check treatment response. The primary treatment administered on the case’s first presentation was the following: syrup Zovirax 20 mg/kg four times daily for 1 week, eye ointment Virgan gel four times daily until next re-examination, cyclogyl collyrium twice daily and thealoz duo collyrium (5 ml), four times daily. Significant amelioration was observed within 10 days after the initiation of medication. After the seventh day only subepithelial opacities were noted in the cornea of the left eye with significant retirement of the dendritic ulcer that was observed on the first visit (Figure 1). The cornea acquired full clarity after day 20, with only minor remaining limbitis in the left eye (noted epithelial defects near the limbus). During the follow up period, on the examination that took place on 18.03.2025, slit lamp examination revealed subepithelial corneal opacities in the left eye, absence of inflammatory cells in the anterior chamber and complete resolution of the dendritic ulcer. Therefore, the treatment administration was remodeled as follows: collyrium FML two drops twice daily, gel Virgan one drop three times daily, collyrium Thealoz duo (artificial tear) four times daily and collyrium Idroflog three times daily. The visits were programmed with intervals of seven days from one another (periodic monitoring once a week) to check for response to treatment. The next one took place on 24.03.2025 and revealed negative fluorescein staining (absence of corneal epithelium erosions or ulcers), however some subepithelial opacities remained. The doctor in charge decided to stop the administration of virgan gel due to the amelioration of the clinical picture and continue with a regimen of collyrium FML twice daily, collyrium idroflog four times daily and artificial tears five times daily. The next examination was scheduled to take place in seven days. The initial eye discomfort and concomitant ocular symptoms had clearly subsided thanks to the eradication of the causative factor (successful targeted treatment) and the relieving effect of the artificial tears’ application in the affected eye. This is a typical case of HSV-1 ocular infection in a pediatric patient that exhibited satisfactory response to treatment.

Regarding the second case, the sixteen-year-old patient was
referred to the ophthalmologic emergency department on the 5th
of March 2025 and was immediately imported for hospitalization
after a quick first evaluation. The patient mentioned sudden
onset of pain in the RE, headache and nausea. An initial slit lamp
examination revealed edema and opacification of the cornea of the
right eye with the development of bullous keratopathy. Corneal
percipitates were also noted as well as a pathological pupil reflex,
(non-reactive, in a mydriasis state) in the RE. Extensive conjunctival
injection was also present in the same eye accompanied by
herpetic disciform keratitis temporal to the limbus, visualized as a
focal opacification in the corneal region. In the anterior chamber
(A/C), a significant reaction due to the presence of several cells
(+++) was noted. The measured intraocular pressure of the right
eye with the use of tonometry was recorded to be 45 mmHg. The
swelling of the cornea with the accompanying glaucomatocyclitic
crisis of the right eye led to the diagnosis of HSV- induced Uveitic
Glaucoma (Figure 2). Immediate hospitalization of the patient
took place for pharmaceutical treatment and monitoring of
the disease. The preliminary emergency management of the
condition included administration of Lumigan eye drops, tablets
of acetazolamide, Sopa K, mannitol, collyrium cosopt, collyrium
tobradex, tb Valtrex 500 mg, gel Virgan and Cyclogyl. The next
day (6th of March), slit lamp examination revealed the presence
of disciform keratopathy (OD) due to HSV infection, whereas the
anterior chamber inflammation remained (but milder than the
previous day). The intraocular pressure was measured to be 11
in the right eye and 13 in the left eye. Fundoscopy of the posterior
pole in both eyes did not reveal any alteration. Nevertheless, a
notable overall improvement of the right eye’s ocular symptoms
was recorded that was accompanied by an amelioration of the
patient’s systemic condition (Figure 3). Therefore, a unanimous
decision was made by the doctors of the clinic for the patient to be
discharged after adapting his medical treatment as follows:
1. Tb Valtrex 1000 mg (twice daily)
2. Eye ointment Virgan- ganciclovir (four times daily)
3. Use of cycloplegic collyrium twice daily.
f2
However, after more thorough consideration the final
pharmaceutical Rp received by the patient was:
1. Tobradex collyrium six times daily
2. Lumigan collyrium once daily
3. Cosopt collyrium twice daily
4. Eye ointment Virgan six times daily
5. Tb Valtrex twice daily, whereas acetazolamide was
stopped. The measured IOP after the treatment intake was 12
mmHg for the right eye and 13 mmHg for the left eye with a
significant decrease of ocular symptoms and corneal alterations.
The patient was periodically monitored during the next month (every seven days), with a noticeable improvement in his clinical profile in each re-examination and as a result only minor modifications of his medication guidelines were decided by the director of the clinic and his colleagues.
The examination that took place on the 7th of March, decided in the remodeling of the regimen as follows: collyrium Tobradex six times daily for four days and then tapering to dexafree and tapering to one drop every one week, collyrium cyclogyl once daily for four days, collyrium cosopt once daily for four days and continuing of tb Valtrex 1gr twice daily for four days and oint virgan five times daily for four days. The patient’s visual acuity measurement was 10/10 in both eyes, with only minor inflammation in the A/C (+) and conjunctival injection in the 7th to 9th hour. His IOP measurement was 12 mmHg in the RE and 15 mmHg in the LE. The next visit was rescheduled on the 11th of March, where an amelioration of his clinical profile was recorded with FLARE (++) and Tyndall (+) in the A/C, reduced IOP (13 mmHg in both eyes) and as a result his medical treatment was decided as follows: collyrium Dexafree four times daily, collyrium cosopt twice daily, ointment Virgan five times daily and stopping of collyrium cuclogyl.
The next re-examination took place on the 20th of March (after nine days) where a subepithelial caterpillar hair induced lesion was observed near the previous area of damage. The patient demonstrated satisfactory compliance with the regimen indicated by the medical team, however the following modifications were pointed out: discontinuing of tb Valtrex after the completion of 14 days administration, continuing of Dexafree four times daily, collyrium cosopt twice daily and oint Virgan five times daily. The next examination was scheduled in two weeks for monitoring of responsiveness to treatment.
Disciform keratitis has an unclear etiology. The most preliminary signs are a central zone of stromal oedema, often with overlying epithelial oedema. Large granulomatous keratic precipitates underlying the oedema are noted as well as Descemet membrane folds in severe cases. The IOP is usually elevated. Regimens should be individually adapted to each patient’s needs, since a broad approach to management is available. Careful monitoring and adequate treatment are imperative to minimize progression of inflammation and scaring. Initial treatment is with topical steroids (prednisolone 1% or dexamethasone 0.1%) with antiviral cover, four times daily. Cycloplegia can be used to improve discomfort if needed. Subsequently, regimen dosage can be tapered to 0.5% prednisolone once daily. Topical ciclosporin 0.05% may be useful, particularly in the presence of epithelial ulceration and to facilitate tapering of topical steroids such as in steroid- related IOP elevation [1].
Discussion
These cases represent two different manifestations of HSV-1 infection. The first case (13-year-old male patient) exhibited mainly corneal alterations (dendritic ulcer) with no significant increase of intraocular pressure and absence of severe inflammation (cells) in the A/C which guided the administration of anti-herpetic treatment alone and rendered the long-term use of cyclogyl collyrium and anti-glaucoma drops unnecessary. On the other hand, the presence of severe inflammation (increased number of cells) in the A/C and the high intraocular pressure measurement in the RE of the second case (16-year-old male patient) guided the systematic use of cyclogyl collyrium and antiglaucoma treatment as useful. These cases constitute vivid examples of daily clinical practice emergencies that require adjustment to different medication guidelines according to each individual’s needs based on his clinical profile and ocular manifestations. The recording of these cases aspires to raise awareness in ophthalmologists worldwide in managing successfully similar emergencies by following the right protocol and carrying out a thorough evaluation (slit lamp examination, fluoresceine staining, IOP measurement and fundoscopy) before initiating treatment. A brief differential diagnosis of HSV- Induced Uveitis Glaucoma is listed in Table 1.

Conclusions
The occurrence of HSV-1 ocular infection is not rare amongst pediatric patients and all physicians should be properly informed of the broad spectrum of its appearance (as presented in the previous cases) in order to achieve preliminary recognition of the disease and effective control and interception of the possible sightthreatening complications. The development of a standardized management and monitoring protocol could be useful or even imperative in these cases.
References
- Salmon JF (2024) Kanski’s Clinical Ophthalmology, A Systematic Approach, Tenth Edition, Elsevier. Chapter 7, Cornea, p. 220-223.
- Will’s Eye Hospital, Herpes Simplex Keratitis | Wills Eye Hospital
- Hung Crystal, JoAnn A Giaconi (2023) Glaucomatocyclitis Crisis (Posner- Sclossman Syndrome), American Academy of Ophthalmology. Glaucomatocyclitic Crisis (Posner-Schlossman Syndrome) - EyeWiki
- Okonkow ON, Zeppieri M, Tripathy K (2024) Posner -Schlossman Syndrome. In StatPearls [Internet]. Treasure Island (FL).






























