Abstract
Introduction: A pre-anesthetic assessment is usually required during cataract surgery, the leading cause of curable blindness. To this end, we wanted to know the contribution of this assessment to patients undergoing cataract surgery at the Yaoundé Gynaeco-Obstetric and Paediatric Hospital (HGOPY).
Methodology: Descriptive, retrospective, and cross sectional study, carried out from January 15 to April 30, 2022, at HGOPY. All patients who underwent cataract surgery at HGOPY between 2016 and 2020 were included in our study. The variables of interest were age, sex, medical and surgical history, clinical characteristics of the cataract, paraclinical examinations and results, ASA classification and type of anesthesia recommended. The data was analyzed by IBM-SPSS software version 25.0.
Results: We recruited 250 surgical patient files. The sex ratio was 0.78 for 56% women. The average age was 58±21 years; 66.34% of patients had a chronic pathology including diabetes (41%) and high blood pressure (39.5%). The proportion of abnormal investigation results was 10% for blood laboratory tests (blood count, prothrombin time, urea/creatinine, fasting blood sugar), 6% for electrocardiogram and 4% for chest X-ray. One hundred and thirty patients (63%) were classified ASA2 followed by 71 (35%) ASA1 patients. Loco-regional anesthesia was the most used type and the cost of a complete pre-anesthetic assessment was estimated at 37,650 CFA francs (58 euros), approximately a quarter of the overall cost.
Conclusion: Our work confirms that pre-anesthetic assessment is useful for screening for unrecognized comorbidities or unstable clinical conditions; however, it can be minimized depending on the clinical status in adult patients.
Keywords: Cataract surgery; Preanesthetic assessments; Comorbidities; Yaoundé; Cameroon
Abbreviations: OAD: Oral Antidiabetics; VKA: Vitamin K Antagonists; BP: Blood Pressure; BMI: Body Mass Index; FBS: Fasting Blood Sugar; LVF: Left Vetricular Failure; WHO: World Health Organization
Introduction
Cataract is defined by the World Health Organization (WHO) as a partial or total opacification of the lens. This pathology is considered to be one of the main causes of visual impairment and blindness in the world after refractive errors according to WHO [1]. Cataract remains a pathology essentially linked to aging and therefore inevitable. A few studies have been conducted on the prevalence of cataract in the world. In Asia, Chatterjee et al found a prevalence of 1% in people between 30-49 years old, 67% for those over 70 years old [2]. In the United States, Congdon et al found a prevalence of 17.2% in Americans aged over 40 years old with a sex ratio of 1.37 in favor of women [3]. In Central Africa, more precisely in Cameroon, in a study carried out in the Central region, Afetane et al in 2018 found a prevalence of 5.14% in a population with an average age of 70 years and 54.80% of eyes were affected by blindness [4]. The diagnosis of this condition is mainly clinical. The symptoms can vary depending on the level of damage to the lens, however the reduction in distance visual acuity remains the main symptom; photophobia with the presence of colored halos around lights can also suggest a cataract [5]. The only treatment to date remains surgery by ablation or excision of the lens (the most widely used method) followed by appropriate optical correction [6].
Although most cataract surgeries are performed on an outpatient basis, a pre-anesthetic assessment remains required, recommended and prescribed by surgeons. Cayzac et al found that performing phacoemulsification procedures under topical or sub- Tenon anesthesia without prior pre-anesthetic consultation showed anesthetic and surgical complication rates comparable to those reported in the literature [7]. In Cameroon, Nomo et al found among the community-related barriers to surgery the poor results of old surgical practices probably due to comorbidities not detected at the time of consultation [8]. In our context, preanesthetic assessments are not systematically carried out in all our hospitals. The aim of this study was to determine the contribution of the pre-anesthetic assessment in cataract surgery at the Yaoundé Gynaeco-Obstetric and Paediatric Hospital (HGOPY).

Materials and Methods
We conducted a descriptive, retrospective and cross-sectional study in the anesthesia and intensive care and Ophthalmology units of the Yaoundé Gynaeco-Obstetric and Paediatric Hospital over a five-year period from January 2016 to January 2020 for four months from January 2022 to April 2022. We studied the records of all patients operated on for cataracts at the Yaoundé Gynaeco- Obstetric and Paediatric Hospital who had a pre-anesthetic consultation. We included in our study all the records of patients followed in the Ophthalmology unit for an operable cataract whose surgery was scheduled and the pre-anesthetic assessment carried out in the Anesthesia and intensive care unit of the Yaoundé Gyneco-Obstetrics and Pediatric Hospital. The minimum sample size was estimated at 83 patients according to the Cochrane method. Data were collected in both units using a previously designed data sheet. We obtained ethical clearance for this study from the Institutional Research Ethics Committees of the Gyneco Obstetric and Pediatric Hospital of Yaoundé and the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé I. Data confidentiality was respected. The variables of interest were sociodemographic data, personal history, clinical characteristics of operable cataract, results of preoperative assessments (biological, radiological and specialized consultation), the ASA (American Society of Anesthesiologists) classification of the anesthetic risk of patients, the type of anesthesia used (general, sub- Tenon, laterobulbar, topical) and the surgical technique performed. The distribution of normal values of the different variables is shown in Table 1. The data was analyzed using IBM-SPSS version 25.0 software.
Results
Epidemiological Profile Socio-Demographic Characteristics
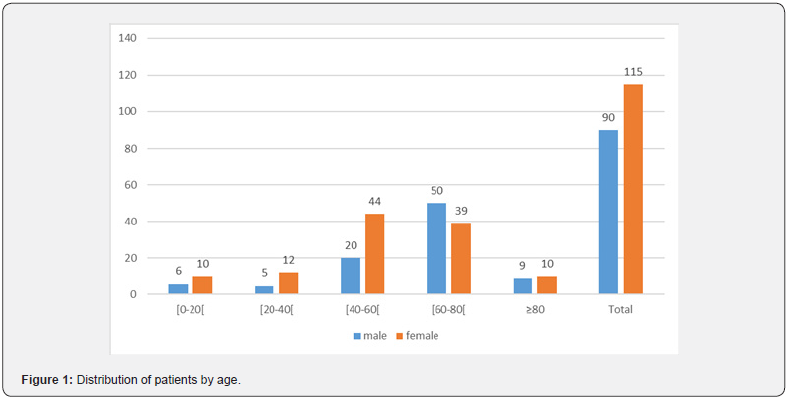
We selected 205 patient files, including 115 women (56%) and 90 men (44%), giving a sex ratio of 0.78. The average age was 58 ± 21 years, with extremes ranging from 1 to 91 years. The most represented age group was [60-80] years (Figure 1).
Background
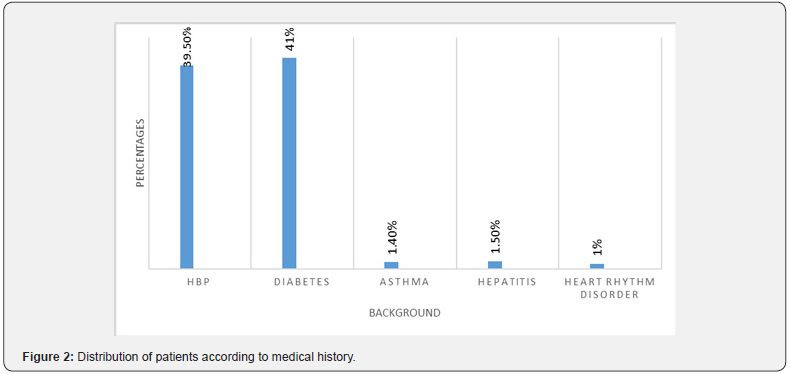
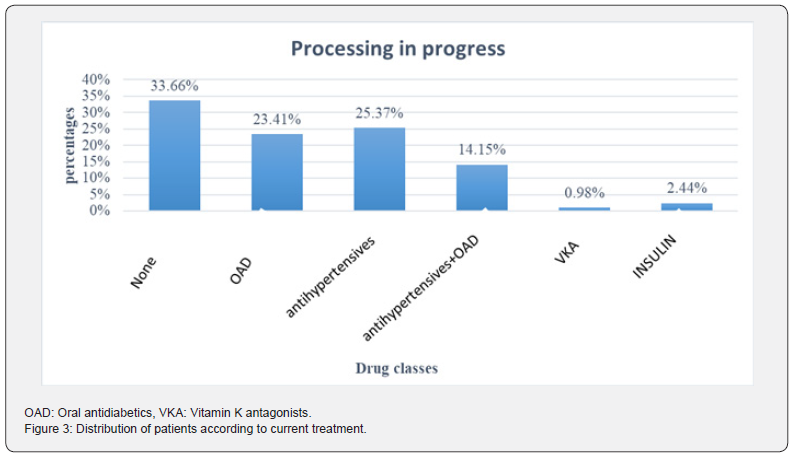
High blood pressure accounted for 39.5% (81 patients) and diabetes 41% (85 patients). We noted seven cases of type 1 diabetes and 78 cases of type 2 diabetes ( figure 2). One hundred and thirty-six patients (64.34%) were undergoing prior treatment. The most recurrent drug classes were antihypertensives 39.52% (81 cases) followed by oral antidiabetics 37.56% (78 cases) (Figure 3). Unilateral cataract was the majority in 98% of cases, i.e., 201 patients and 4 cases (2%) of bilateral cataract.
Clinical Data Vital/Anthropometric Parameters • Blood Pressure (BP)
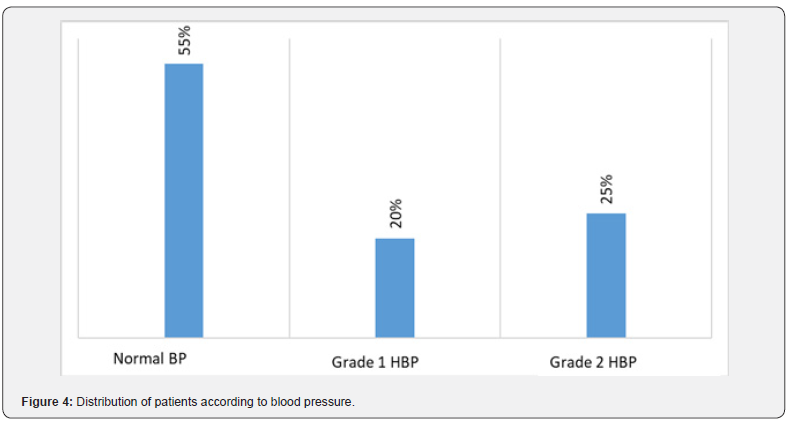
Elevated blood pressure was found in 45% of patients (n=90). The grades of hypertension are shown in Figure 4. It was noted that of the 81 patients with known hypertension, 19 (33%) had elevated blood pressure on clinical examination compared to 62 who had controlled BP.
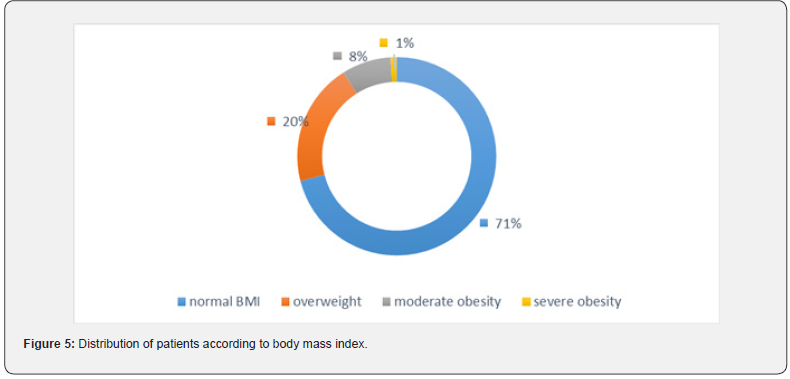
• Body Mass Index (BMI)
The majority of patients 71% (n=145) had a normal BMI. Sixty patients (29%) had a BMI greater than 24, and there were no cases of underweight (Figure 5).
• Clinical Signs
No visible clinical signs were found in the 205 patients.
Results of Additional Examinations Biological
Abnormal fasting blood glucose levels were found in 30% (n=63) of patients. The results obtained are presented in Table 2.
Morphological Assessments
Of the 172 ECGs requested, 10 (6%) returned with abnormalities, all of which were left ventricular hypertrophy. All the results of the various morphological and physiological assessments are described in Table 3.


v
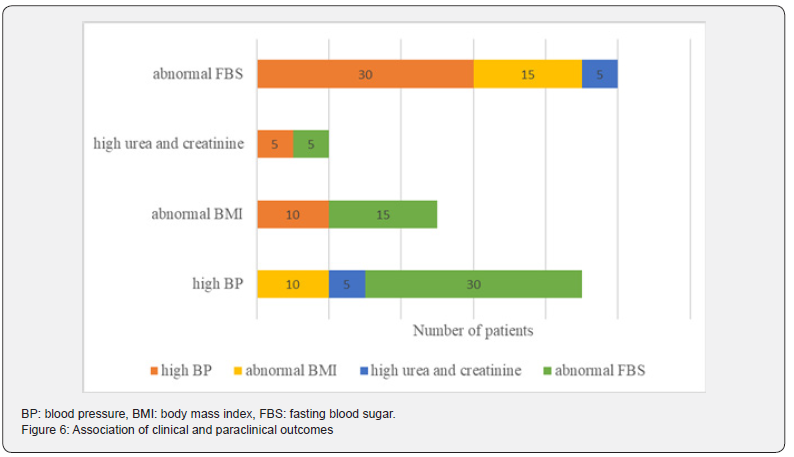
In our series, among the patients with elevated BP, 30 had abnormal GAJ, 10 had abnormal BMI, and five had elevated blood urea-creatinine. The different associations of clinical and paraclinical outcomes presented by the patients are described in Figure 6.
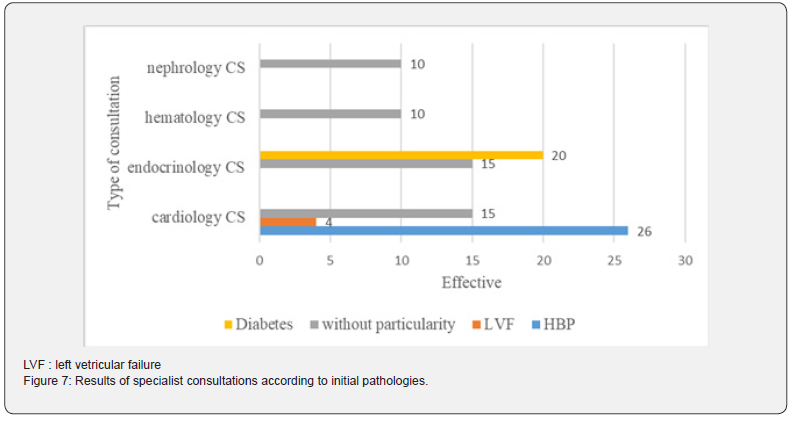
Specialized Consultations
Of the 205 patients in our series, 100 (49%) had an abnormality in at least one of the assessments requiring specialist consultations from other specialties. The results are contained in Figure 7. Among the 100 patients, 50 (24.39% of our series) were diagnosed with an inaugural pathology. The average age of the 100 patients who benefited from consultation with another specialist was 69 ± 9 years with the class [60-80] which represented 80% of these patients. The different indications for these patients are presented in Table 4.

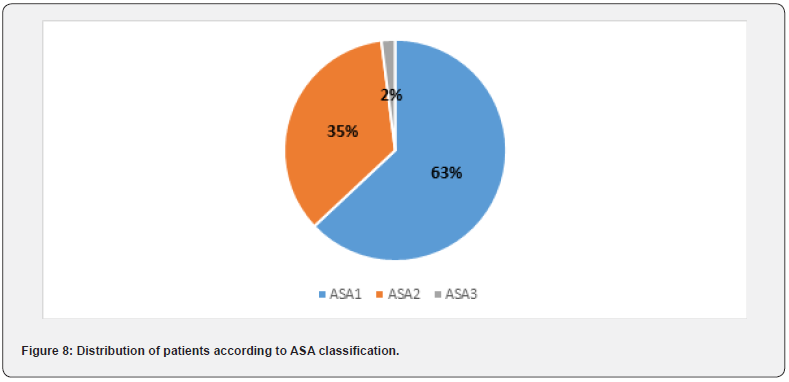
ASA Classification of Patients
ASA2 and ASA1 classes were in the majority with respectively 130 (63%) and 71 (35%) patients and finally 4 patients (2%) classified ASA3 (Figure 8).
Type of Anesthesia Used
Locoregional or laterobulbar anesthesia was the majority in 92% of cases (189 cases) followed by general anesthesia in 8% (16 pediatric cases). No cases of topical anesthesia were found (Table 5).

Cost of the Assessments Carried Out
The total cost of a complete pre-anesthetic assessment by HGOPY was 37,650 CFA francs (or 57.5 Euros) distributed as described in Table 6.

Discussion
Epidemiological characteristics
Women were predominantly represented with a sex ratio of 0.78. This result corroborates that of Afetane et al in Cameroon who found a sex ratio of 0.8 [4]. The average age was 58 years. This figure is lower than that of Afetane et al and Rabii Kouta et al who reported 70 years and 67 years respectively [4] [9]. This difference could be explained by the inclusion in our series of patients of all ages unlike these authors who did not include in their studies patients aged less than 60 years. In Congo, Otiobonda et al reported in their series the presence of HBP as the only antecedent in 13.3% of patients [10]; Rabii Kouta et al found 49% of patients to be diabetic and 48% to have hypertension [9]. Our results were similar to those of Rabii Kouta, in our series we found 41% of diabetic patients and 39.5% with hypertension (figure 2). Cataract is a pathology of the elderly subject who is himself at risk of cardiovascular pathologies.
Clinical features Vital/anthropometric parameters
In our series, 90 patients (45%) had elevated BP when the parameters were taken. Nineteen hypertensive patients still had elevated BP on physical examination, i.e., 9% of cases. In France, Bouvet et al in a study found that 4% of patients operated on for cataracts had an intraoperative hypertensive peak requiring the intervention of the anesthesiologist-resuscitator [11]. Hypertension can be aggravated in the perioperative period by the omission and/or accidental discontinuation of antihypertensive drugs, anxiety, administration of phenylephrine eye drops, hypothermia and pain during the procedure. Anesthesiologists and ophthalmologists are concerned that perioperative hypertension increases the risk of adverse events (cardiovascular and neurological, for example) and the surgical risk of sightthreatening hemorrhage before, during or after cataract surgery. Intra- or periocular bleeding can lead to blindness, especially in cases of large-incision cataract surgery [12]. A Brazilian study found that (22%) of cataract surgeries were postponed due to uncontrolled hypertension [13].
Additional Examinations Biological Assessments • Coagulation Disorders
Four patients (2%) in our series had a coagulation disorder. Although that according to the literature, the risk of hemorrhage would be linked to the insertion of a needle into the orbit, Otionbonda et al reported that the main per-operative complication in their series of cataract surgery was hemorrhagic chemosis, hence the importance of having a normal hemostasis assessment [10]. A French study conducted by Boureau et al on-cataract surgery under anticoagulant or antiplatelet agent: topical and sub -Tenon’s anesthesia showed no intraocular hemorrhagic complications. Some subconjunctival hemorrhages without consequences were noted, more frequent with sub- Tenon’s anesthesia but comparable in the group with or without anticoagulant or antiplatelet agent [14].
• Urea/creatinine
Regarding renal assessment, 5% of patients had elevated serum creatinine. In the United States, Son Huynh et al found a significant incidence between renal failure and cataract surgery for patients aged over 60 years, although according to the literature, this would not be a problem for cataract surgery in the case of local or locoregional anesthesia [15].
• Fasting blood sugar
Of the 205 cases in the series, 63 had hyperglycemia. Postoperative complications of cataract surgery are increased in these patients. Postoperative cystoid macular edema is more frequent and more prolonged in diabetics. In addition, it has been clearly demonstrated that cataract surgery promotes the progression of diabetic retinopathy. For all these reasons, when indicating cataract surgery in diabetics, it is essential to make a very precise assessment of diabetic retinopathy which will determine the postoperative functional visual prognosis [16]. Postoperatively, clinicians should address pseudophakic cystoid macular edema, diabetic macular edema, diabetic retinopathy, and posterior capsular opacification [17]. Ahmed Gazza et al had conducted a comparative study in Morocco showing that corneal edema occurred in 6.3% of non-diabetic patients and in 16.1% of diabetic patients [18]. According to the study of Gondhale et al, diabetics had 1.634 times more risk of postoperative endophthalmitis (P = 0.048), and those with diabetes and hypertension had 3.961 times more risk of having postoperative endophthalmitis (P < 0.001) after adjustment for age, alcoholism, smoking, socioeconomic strata and the presence of a posterior capsule rupture [19].
• Morphological and physiological assessments
Electrocardiological abnormalities. People who suffer from senile cataracts are patients at risk of cardiovascular pathologies that would require assistance from the resuscitation unit perioperatively to avoid cardiac rhythm disorders linked to stress that could hinder surgery and worse lead to cardiac arrest.
• Other specialties
In our series we had identified 26 cases of inaugural hypertension, four patients had seen diagnosed with left ventricular failure and 20 new cases of diabetes, all of type 2. These results can be explained by the absence of regular routine consultations in our context after 40 years which results in late diagnosis of pathologies that can lead to poor results from cataract surgery. Multidisciplinary management is therefore required to balance these parameters.
• ASA Classification
Many authors reported in their series a predominance of ASA classes 1 and 2. Rabii Kouta et al found 40% ASA 1 and 54% ASA 2 [9] and Otiobonda et al in Congo 86.7% ASA 1 and 10.5% ASA 2 [10]. These results are in agreement with ours, i.e., 63 % ASA 1 and 35% for the ASA 2 class. The American Society of Anesthesiologists (ASA) classifies the physical state of patients into six grades, of which ASA 1 represents a normal patient and ASA 2 represents a patient with moderate systemic abnormality [20]. Cataract surgery is a surgery that is generally performe on an outpatient basis and therefore requires that the patient with a chronic pathology or a disturbance of a major function be controlled and stable for better progress of the surgery as well as better postoperative follow-up.
• Type of Anesthesia
The vast majority of patients in our series (92%) had received locoregional anesthesia and the remainder had received general anesthesia. None of the patients in the series required surgeons to convert from locoregional to general anesthesia. These figures are different from those of Otiobonda et al [ 10] in Congo, Rabii Koutta et al [9] in Morocco and Bisinotto et al [21] in Brazil who all had 100% of surgeries performed under loco-regional anesthesia. This difference could be explained by the inclusion in our study of very young patients who could only be operated on under general anesthesia. Furthermore, Quentin Duroi et al [22] in a study compared the benefits and disadvantages of local anesthesia versus loco-regional anesthesia, they found that local anesthesia reduced all the risks associated with inserting a needle into the orbit but provided less good operating conditions than well-conducted loco-regional anesthesia.
• Cost of Assessments
The cost of a complete pre-anesthetic assessment at HGOPY that we found was 37,650 CFA francs or 58 euros. Combined with the already high cost of surgery, the financial means necessary for surgery on a single eye do not seem within everyone’s reach. Nomo et al [8] in a study conducted in Cameroon found an overall rate of cataract surgery of 26.8%. The high cost of surgery was the main reason for refusal of surgery, 59.6 % of patients in their series lived below the minimum wage (36,270 CFA francs or 56 euros) and that for 96.4% of patients, care was paid for either by relatives or by themselves [8]. Generally, patients with operable senile cataracts are retired and are not insured. The limitation of this study is that of retrospective studies which poses problems of missing data and archiving.
Conclusion
At the end of our study, it appears that nearly half of our study population had either diabetes or hypertension. ASA classifications 1 and 2 were the majority with a cumulative 98%. The comorbidities found associated with the total cost of a preanesthetic assessment could constitute a factor of poor prognosis for cataract surgery or even non-surgery. The measurement of fasting blood sugar, blood pressure and prothrombin time were useful and their non-measurement could have an impact on the course of cataract surgery and follow-up.
References
- (2023) Organisation Mondiale de la Santé. Cécité et déficience visuelle.
- Chatterjee A, Milton RC, Thyle S (1982) Prevalence and aetiology of cataract in Punjab. Br J Ophthalmol 66(1): 35-42.
- Congdon N, Vingerling JR, Klein BE, West S, Friedman DS, et al. (2004) Eye Diseases Prevalence Research Group. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol 122(4): 487-494.
- Afetane Evina TG, Noutouom J, Nkumbe H, Tchouyo M, et al. (2018) Épidémiologie de la Cataracte en Stratégies Avancé Health Sci-Dis 19(4 S 1): 17-19.
- Schweitzer Cedric (2018) La cataracte, une pathologie courante. Actualités Pharmaceutiques 57(576): 25-27.
- Crispim J, Chamon W (2017) Lens: Management of Cataract Surgery, Cataract Prevention, and Floppy Iris Syndrome. Handb Exp Pharmacol 242: 163-178.
- Cayzac V, Bordes J, Valero B, Voisin H, Sagnard M, et al. (2005) Cataract surgery without preanesthetic consultation: A 2-year retrospective study. J Fr Ophtalmol 48(3): 104428.
- Nomo AF, Efouba YJ, Epee E, Nanfack NC, Akono ME et al (2020) Les barrières à la chirurgie de la cataracte à l'HGOPY; Revue SOAO 15e congrès SAFO pp: 25-32.
- Rabii Kouta, Moutaouakil A, Filali K (2018) Apport d'une procédure de consultation d'anesthésie simplifiée dans la chirurgie de cataracte. Thèse Faculté de Médecine et de Pharmacie de Marrakech.
- Otiobanda GF , Nganga Gabou F , Ngabou G , Atipo-Tsiba WP, Mokoko B (2013) L’anesthésie pour chirurgie de la cataracte. Revue africaine d’anesthésiologie et de médecine d’urgence 2013. Tome 18 (2).
- Bouvet L, Calderon AL, Augris-Mathieu C, Diot-Junique N, Benoit MP, Boselli E, et al (2015) Évaluation du recours à l’anesthésiste-réanimateur lors de la chirurgie de la cataracte réalisée sous anesthésie topique; J Fr d'Ophtalmol. 2015;38(4): 316‑3
- Kumar CM, Seet E, Eke T, Joshi GP (2017) Hypertension and cataract surgery under loco-regional anaesthesia: not to be ignored? Br J Anaesth 119(5): 855-859.
- Magri MP, Espíndola RF, Santhiago MR, Mercadante EF, Kara Júnior N (2012) Cancelamento de cirurgias de catarata em um hospital público de referência [Cancellation of cataract surgery in a public hospital]. Arq Bras Oftalmol 75(5): 333-336.
- C Boureau, Y Ounnoughene, M Coudray, C Mesner (2002) Chirurgie de la cataracte sous anticoagulant ou antiagrégant: anesthésie topique et sous té, J Fr d’Ophtalmol 25(5): 130.
- Huynh SC, Kifley A, Strippoli GFM, Mitchell P (2005) Is renal impairment a predictor of the incidence of cataract or cataract surgery?. Ophthalmology 112(2): 293‑
- Malecaze F (2003) La chirurgie de la cataracte chez le diabé J Fr d’Ophtalmol 26(5): 525-527.
- Go JA, Mamalis CA, Khandelwal SS (2021) Cataract Surgery Considerations for Diabetic Patients. Curr Diab Rep 21(12) :67.
- Ahmed Ghazza, Aimrane A, Oukassou R, Lahoucine A, Redouane M, et al. (2021) Œdème de cornée après chirurgie de cataracte: étude comparative entre patients diabétiques et non diabé PAMJ Clinical Medicine 5(48).
- Gondhale H, Jaichandran VV, Jambulingam M, Anand AR, Srinivasan S, et al. (2021) Distribution and risk factors of postoperative endophthalmitis in people with diabetes. Indian J Ophthalmol 69(11): 3329-3334.
- ASA Physical Status Classification System.
- Bisinotto Flora, Mesquita Gustavo, Miziara Adriana, Martins Laura (2016) The preanesthetic evaluation for ophthalmic surgery in the elderly is really necessary? The reality of a public hospital. Revista Brasiliera d’Oftalmologia 75: 279-285.
- Duroi Q, Baudet JM, Bigoteau M, Slim M, Pichard T, et al. (2021) Ambulatory cataract surgery centre without perioperative anaesthesia care: a prospective cohort study. Sci Rep 11(1): 8311.






























