Rotational Stability of Toric Intraocular Lenses
Debaruna Ghosh* and Narayan Bardoloi
West Bengal University of Health Sciences, 132, Goswami Para Road, Howrah, India
Submission: December 13, 2024; Published: January 09, 2025
*Corresponding author: Debaruna Ghosh, West Bengal University of Health Sciences, 132, Goswami Para Road, Howrah, India
How to cite this article: Debaruna G, Narayan B. Rotational Stability of Toric Intraocular Lenses. JOJ Ophthalmol. 2025; 12(1): 555826. DOI: 10.19080/JOJO.2025.12.555826
Abstract
Purpose: To study the short-term rotational stability of toric Intraocular lens. To assess the factors that affect rotational stability. To assess the residual astigmatism with toric IOL implantation.
Design: The prospective non-randomized interventional study.
Material and Methods:
Setting: A tertiary eye care hospital between the period of November 2018 to February 2020.
Population: 55 Patients were enrolled.
Intervention: Biometry was done using two instruments, the Oculyzer (ALCON) and IOL master 500 (ZEISS). All the patients underwent cataract surgery by the same surgeon assisted by the VERION digital overlay. Visual acuity and IOL rotation were assessed on post-operative days 1, 7 and 30 using the ImageJ software.
Outcome: Residual astigmatism was measured on postoperative days 7 and 30. Data was analysed using Statistical Package for Social Sciences (SPSS) Version 16.0 (IBM, Chicago).
Results: The patients recruited were aged 62.98 ± 9.15 yrs. 40 patients (72.72%) achieved uncorrected visual acuity better than 0.10. There was no significant correlation between white to white, axial length, anterior chamber depth and rotational stability (r=-0.002, p=0.98; r=0.02, p=0.45; r=0.020, p=0.88 respectively). The IOLs underwent a mean rotation of 0.39°±0.91° (00-2.550) in 30 days. The mean residual astigmatism on postoperative day 30 was 0.30±0.30D. There was a mean difference between 0.54D and 10.660 in the magnitude and axis of astigmatism measured by the two instruments. There was no statistically significant difference between K values measured by both instruments (z=-0.20326, p=0.84148).
Conclusion: Toric IOLs give good post-operative outcomes in terms of visual quality and rotational stability. The IOL Master and Oculyzer are similar but not interchangeable for biometry. In this study, axial length, anterior chamber depth and white to white did not show any association with IOL rotational stability.
Keywords: Astigmatism; Toric IOL; Rotational Stability
Abbreviations: OVD: Ophthalmic Viscosurgical Devices; IOLs: Intraocular Lenses; MICS: Minimal Incision Cataract Surgery
Aim of Study
· To study the short-term rotational stability of toric Intraocular lens.
· To assess the factors that affect rotational stability.
· To assess the residual astigmatism with toric IOL implantation.
Material and Methods
This institution based prospective non-randomized interventional longitudinal study was donein the OPD setting of a tertiary care hospital in India over 6 months. All cataract patients attending the OPD with a cylinder power in the range of -1D to -4.11D in the corneal plane were included. The exclusion criteria included patients with ocular problems such as previous intra ocular surgery, pseudoexfoliation syndrome, irregular astigmatism, retinal disease impacting the central visual acuity, glaucoma, fixating problems, zonular instability, previous or intra-operative posterior capsule rupture, ectopic pupil, refractive but not corneal astigmatism, extracapsular extraction or surgical techniques causing unpredictable surgically induced astigmatism, patients unavailable for subsequent follow up and patients who do not give written informed consent. 55 patients were enrolled with the above criteria.
Patients with cataract underwent comprehensive eye examination that included a detailed history taking, visual acuity with Snellen’s Chart, diffuse torch light examination, undilated refraction and slit lamp examination, Goldmann applanation tonometry and fundus examination. Cataract was graded as per LOCS II classification. All patients were taken for Ocular coherence tomography to look for the health of the retina. Patients requiring cataract surgery underwent routine blood tests. Fitness for surgery was taken.
Patients underwent optical biometry by the IOL Master wherein the keratometry, axial length, anterior chamber depth, pupil size, white to white distance and IOL power was calculated. Patients with corneal astigmatism were taken for the Scheimpflug tomography using the Pentacam. The IOL power was calculated using the Barrett online toric IOL formula. Preoperatively, slit lamp assisted marking technique was used.
Surgical Technique:
Each cataract surgery was performed by the same surgeon using the MICS (Minimal incision cataract surgery) technique with a CENTURION system (Alcon), VERION image guidance system, and LUMERA T microscope (ZEISS). After proper antiseptic dressing and draping, two 1mm paracentesis incisions were made, continuous curvilinear capsulorhexis done, the eyeball filled with ophthalmic viscosurgical devices (OVD), a 2.2mm triplanar temporal limbal incision was made. Hydrodissection was done, the nucleus was rotated. Phacoemulsification was done. The IOL used in every case is Acrysoftoric IOL by Alcon- SN6AT series. The surgical steps were aided by the VERION digital marking system. The IOL was initially kept 3-4 degrees short of the target axis. After OVD wash the IOL was correctly aligned with the irrigation probe. Intracameral moxifloxacin was administered. The wounds were hydrated.
Analysis:
The uncorrected/best corrected visual acuity was monitored on post operative days 1,7 and 30. The residual astigmatism was noted on day 30. For checking rotational stability of the IOL the eye was dilated with Tropicamide and phenylephrine and photographs taken keeping the head erect on post operative days 1,7 and 30. The degree of rotation of the intraocular lens was analyzed by the ImageJ software. Appropriate statistical methods were used for analysis.
Results
The mean age of the patients included in the study was 62.98±9.15 yrs. 65.5% of the patients were in the age group 50 - 69 years. The ratio of male to female (Male: Female) was 2.4:1.0. Out of 55 patients, 40 patients achieved UCVA 6/6p, 49 patients (89.09%) achieved UCVA equal to or better than 6/9 and 52 patients (94.54%) achieved UCVA equal to or better than 6/12 on post operative day 30. Two patients had UCVA of 6/15 while one patient achieved 6/18. However, with correction they were able to achieve 6/6. There was no significant correlation between each white to white, axial length and anterior chamber depth with rotational stability (r=-0.002, p=0.98; r=0.02, p=0.45; r=0.020, p=0.88 respectively). The mean rotation of the IOL at 30 days postoperative was 0.39°±0.91°. The mean residual astigmatism on postoperative day 30 was 0.30±0.30D.
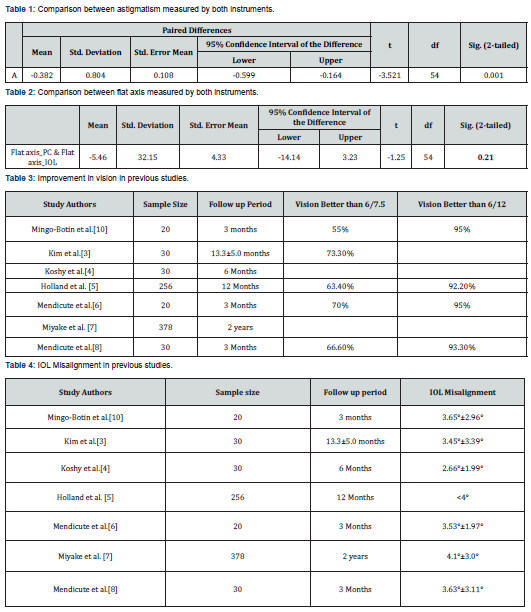
There was a mean difference of 0.54D and 10.660 in the magnitude and axis of astigmatism measured by the Oculyzer and IOL Master. Mean (SD) of flat axis using Oculyzer and IOL master are 90.69 (46.54) and 96.15 (44.91) respectively. IA statistically significant correlation was observed in terms of flat axis measurement with both instruments (r= 0. 75, p<0.001, Pearson correlation). There is a statistically significant increase in magnitude of astigmatism noted with IOL master compared to the pentacam. (p=0.001, paired t-test). There was no statistically significant difference between K values measured by both instruments (z=-0.20326, p=0.84148) (Table 1&2). The axial length showed no statistically significant correlation to the residual astigmatism (r=0.15, p= 0.27). The axial length and IOL rotation on post operative day 30 show statistically insignificant correlation (r=0.02, p=0.45). The mean residual astigmatism on postoperative day 30 was 0.30±0.30D.
Discussion
Shimizu et al. first introduced toric intraocular lenses (IOLs) in 1992 [1]. Thereafter, toric IOLs have become the treatment of choice for correcting significant corneal astigmatism in cases undergoing cataract surgery [2-8]. Accurate alignment of toric IOL is a must to achieve best outcome. The methods to place the preoperative reference and axis marks can be classified as manual methods, iris fingerprinting techniques, image‑guided systems and intraoperative aberrometry‑based methods [9]. The postoperative outcomes after implantation of toric IOL may be assessed in terms of visual acuity and precision and stability of IOL alignment. In this study, 40 patients (72.72%) acheived uncorrected visual acuity better than 6/6p. Good visual outcomes were obtained for all patients. Table 3 shows the proportion of improvement in visiual acuity in previous studies.
The design and material influence the stability of the IOL inside the capsular bag. Hydrophobic acrylic lenses are most stable [3-8,10]. This can be attributed to the development of strong adhesions between the IOL and lens capsules in the early postoperative period [9]. The axis of implanted toric IOL may be assessed using the slit‑lamp with a rotating slit. This requires proper dilatation to visualize the IOL graticules. The slit‑lamp measuring reticule has 10° steps which is limits the accuracy of this method. ImageJ computer software is a simple, fast and inexpensive method to measure the toric IOL axis using a camera‑enabled cellular phone and no additional equipment is required [11]. In this study, the IOLs underwent a mean rotation of 0.39°±0.91°(00-2.550) in 30 days. This study showed the Acrysoftoric IOL be considerably stable in terms of rotational stability. Table 4 shows rotation undergone in other related studies.
In this study it is observed that the amount of IOL rotation between postoperative days 1 and 7 was greater as compared to that between postoperative days 7 and 30. This agrees with the observation of Miyake T et al. that IOL rotation can occur within 1 h after surgery, though most rotations occur within the first 10 postoperative days [7]. In this study, there was no significant correlation between white to white axial length, anterior chamber depth and rotational stability(r=-0.002, p=0.98; r=0.02, p=0.45; r=0.020, p=0.88 respectively).This is in contrast to the study done by Shah GD et al. who concluded that early postoperative rotation is affected by a number of factors like large capsular bag size, high axial length, retained viscoelastics, and smaller haptics. Large bag size is itself correlated to increased axial length [12]. However, it agrees with the observations by Gao YF et al. and Klamann MK that the rotational stability of toric IOLs has no correlation with axial length or other biometric parameters [13,14-16].
The toric IOLs show lesser residual astigmatism when compared to nontoric IOLs with or without limbal relaxing incisions [5,6,8,9,17-19]. Residual astigmatism is caused by erroneous preoperative measurement, marking errors, ignoring posterior corneal astigmatism, ELP, and IOL rotation after surgery [9]. The mean residual astigmatism on postoperative day 30 was 0.30±0.30D. Related studies done previously show similar outcomes as shown in table 5. Previous studies have found 1.1% of cases implanted with AcrySoftoric IOL required repositioning [7]. Repositioning of the toric IOL is needed where the current axis differs from the target axis by more than 10°. Otherwise, no intervention is required post surgery [15]. Patients in this study, patients were satisfied with their visual outcomes.
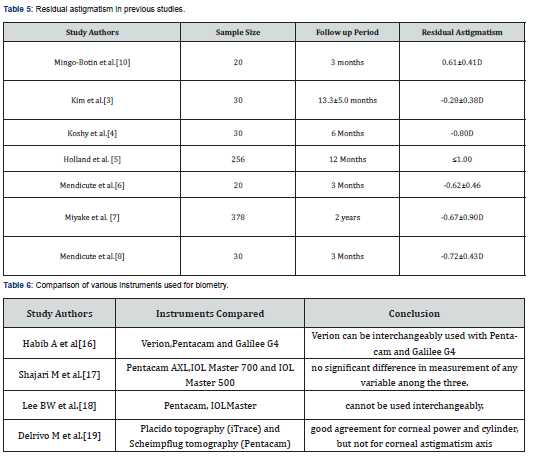
In this study, there was a mean difference of 0.54D and 10.660 in the magnitude and axis of astigmatism measured by the Oculyzer and IOL Master. A statistically significant strong positive correlation in terms of axes as well as the magnitude of astigmatism measurement with both the instruments. This study concludes that the two instruments cannot be used interchangeably. Table 6 shows related conclusions from studies done previously.
Limitations of the study
· Positioning the patient on post operative days required a great deal of cooperation for perfect alignment with the line of the slit lamp rendering the process cumbersome.
· In this study, sample size was limited, and follow-up period was short. There is a need to study with larger sample size and extended follow-ups.
Conclusion
Toric IOLs provides a high degree of spectacle independence and minimal to negligible residual astigmatism. IOL rotation is thought to be affected by factors such as large capsular bag size and high axial length. However, this study shows biometric parameters like anterior chamber depth, axial length, white to white are unlikely to affect short term rotational stability of IOLs. Early postoperative rotation (within 7 days) is more likely than late rotation.
References
- Shimizu K, Misawa A, Suzuki Y (1994) Toric intraocular lenses: Correcting astigmatism while controlling axis shift. J Cataract Refract Surg 20(5): 523‑526.
- Thomas BC, Khoramnia R, Auffarth GU, Holzer MP (2018) Clinical outcomes after implantation of a toric intraocular lens with a transitional conic toric surface. Br J Ophthalmol 102(3): 313-316.
- Kim MH, Chung TY, Chung ES (2010) Long‑term efficacy and rotational stability of Acry Softoric intraocular lens implantation in cataract surgery. Korean J Ophthalmol 24(4): 207‑212.
- Koshy JJ, Nishi Y, Hirnschall N, Crnej A, Gangwani V, et al. (2010) Rotational stability of a single‑piece toric acrylic intraocular lens. J Cataract Refract Surg 36(10): 1665‑1670.
- Holland E, Lane S, Horn JD, Ernest P, Arleo R, et al. (2010) The Acry Softoric intraocular lens in subjects with cataracts and corneal astigmatism: A randomized, subject‑masked, parallel‑group, 1‑year study. Ophthalmology 117(11): 2104‑2111.
- Mendicute J, Irigoyen C, Ruiz M, Illarramendi I, Ferrer‑Blasco T, et al. (2009) Toric intraocular lens versus opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg 35(3): 451‑458.
- Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, et al. (2014) Long‑term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg 40(10): 1654‑1660.
- Mendicute J, Irigoyen C, Aramberri J, Ondarra A, Montés‑Micó R (2008) Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg 34(4): 601‑607.
- Kaur M, Shaikh F, Falera R, Titiyal JS (2017) Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol 65(12): 1301-1313.
- Mingo‑Botín D, Muñoz‑Negrete FJ, Won Kim HR, Morcillo‑Laiz R, Rebolleda G, et al. (2010) Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg 36(10): 1700‑1708.
- Teichman JC, Baig K, Ahmed II (2014) Simple technique to measure toric intraocular lens alignment and stability using a smartphone. J Cataract Refract Surg 40(12): 1949‑1952.
- Shah GD, Praveen MR, Vasavada AR, Vasavada VA, Rampal G, et al. (2012) Rotational stability of a toric intraocular lens: Influence of axial length and alignment in the capsular bag. J Cataract Refract Surg 38(1): 54‑59.
- Gao YF, Sun T, Luo JH, Y Y Liu, B K Ma, et al. (20) The rotational stability of toric intraocular lensesandinfluencing factors in cataract patients with different axial length. Zhonghua Yan KeZaZhi 56(1):41-46.
- Klamann MK, Von Sonnleithner C, Gonnermann J, Maier AK, Torun N, et al. (2013) Influence of biometric parameters on rotational stability of toric IOLs. Eur J Ophthalmol 23(6): 836-840.
- Felipe A, Artigas JM, Díez‑Ajenjo A, García‑Domene C, Alcocer P (2011) Residual astigmatism produced by toric intraocular lens rotation. J Cataract Refract Surg 37(10): 1895‑1901.
- Habib A, Khan MS, Ishaq M, Yaqub MA (2018) Agreement between Keratometric readings by VERION image guided System, Galilei G4 and Pentacam. Pak J Med Sci 34(3): 740-743.
- Shajari M, Cremonese C, Petermann K, Singh P, Müller M, et al. (2017) Comparison of axial length, corneal curvature, and anterior chamber depth measurements of 2 recently introduced devices to a known biometer. Am J Ophthalmol 178: 58‑64.
- Lee BW, Galor A, Feuer WJ, Pouyeh B, Pelletier JS, et al. (2013) Agreement between Pentacam and IOL master in patients undergoing toric IOL implantation. J Refract Surg 29(2): 114‑120.
- Delrivo M, Ruiseñor Vázquez PR, Galletti JD, Garibotto M, Fuentes Bonthoux F, et al. (2014) Agreement between placido topography and scheimpflug tomography for corneal astigmatism assessment. J Refract Surg 30(1): 49‑53.






























