Complementary Treatments to Blepharoplasty
Guillermo Rodríguez Iranzo* and Raúl Martínez Belda
Hospital Clínico Universitario, Blasco Ibáñez 17, 46010 Valencia, Spain
Submission:September 13, 2024;Published:September 25, 2024
*Corresponding author:Guillermo Rodríguez Iranzo, Hospital Clínico Universitario, Blasco Ibáñez 17, 46010 Valencia, Spain
How to cite this article: Guillermo Rodríguez I, Raúl Martínez B. Complementary Treatments to Blepharoplasty. JOJ Ophthalmol. 2024; 11(4):555818. DOI: 10.19080/JOJO.2024.11.555818
Abstract
Introduction: Aging clinical signs typically begin in the periocular region. Blepharoplasty plays a crucial role in the treatment of dermatochalasis with an aesthetic and functional aim.
Objectives: To carry out a study of all those medical and surgical procedures that can be used in combination with blepharoplasty for the rejuvenation of the periocular area.
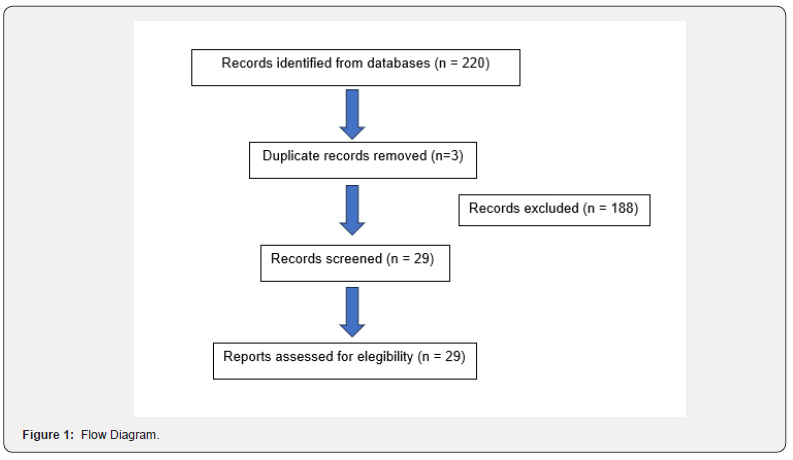
Methods: This is a bibliographic review of the literature, whose databases were Pubmed, ScienceDirect and Cochrane library. After establishing the keywords and applying the methodological criteria, a total of 29 articles were chosen to be included in the final sample of the review.
Results: Lasers and peels can improve skin elasticity in a conservative way associated with surgery. Fillers with hyaluronic acid or autologous fat are useful for restoring volume loss. The use of botulinum toxin in cases of frontalis muscle hyperactivity optimizes the surgical plan. At an intraoperative level, eyebrow elevation and ptosis surgery improve the results of upper blepharoplasty. If there is lateral canthal tendon hypermobility, its reattachment is usually combined with lower eyelid surgery.
Conclusions: Different medical and/or surgical procedures can be used in combination with blepharoplasty to optimize its results.
Keywords:Blepharoplasty; Dermatochalasis; Hyaluronic Acid; Botulinum Toxin; Surgery
Introduction
The periocular region stands out for being the facial area where the aging clinical signs first appear [1]. This is why both the demand for aesthetic treatments in this area and the range of techniques to address them have expanded significantly in the last decade. Blepharoplasty, performed for the treatment of dermatochalasis, is one of the most frequently performed surgical procedures [2], the third for cosmetic reasons after liposuction and breast augmentation surgery. Although it presents good results, it is an invasive procedure, it tends not to be definitive, it can produce visible scars and require touch-ups or complementary treatments in the future [3,4]. Nowadays, there has been an increase in demand for innovative aesthetic procedures that, when used in isolation, are less invasive, providing good results with fewer adverse effects compared to surgery. If used in combination with blepharoplasty, they may be aimed at improving its results [2].
History of Aesthetic Treatments in the Periocular Area
The beginnings of blepharoplasty date back to more than two thousand years ago, when Susruta described eyelid surgery in the Susruta-Tantra. As early as the 10th century, Arab surgeons cauterized excess skin to produce a more youthful appearance [5]. Ambrose Pare described functional upper blepharoplasty in the 16th century to correct visual field loss. In the 19th century, several authors performed skin resection of the upper eyelid [6]. However, it was Von Graefe in 1818 who coined the term blepharoplasty to describe that eyelid surgery [7]. The introduction of lasers for skin vaporization, specifically using CO2, began in 1987 as a treatment modality to eliminate localized skin tumors. The incidental discovery of its cosmetic benefit led to an initial study of facial aesthetic resurfacing in 1989 [8]. In 1994, Weinstein was the first to describe the use of this laser for the treatment of periocular wrinkles [9]. Regarding the erbium: YAG laser, Hibst and Kaufman initially worked with it and recommended it for cosmetic resurfacing [10].
Purified botulinum toxin type A, as the main neuromodulator, was initially developed as an alternative to the surgical treatment of strabismus. In the early 1970s, the effectiveness of botulinum toxin type A in the treatment of benign essential blepharospasm and hemifacial spasm was described. Given the beneficial effect on periocular and glabellar wrinkles reported by Carruthers and Carruthers [11], doctors began to use it for aesthetic purposes in the early 1990s. In 1994, Keen and Blitzer carried out a double-blind study confirming the effectiveness of the toxin in the treatment of hyperkinetic facial lines [12]. Currently it is the most frequently performed aesthetic procedure.
The first steps regarding the use of dermal fillers were described in 1990, when Charles Kelman reported some incidents with the use of bovine collagen (mainly related to severe allergic reactions), as well as the benefits of volume restoration for the treatment of facial wrinkles. Together with the biochemist Dale P. de Vore, he promoted a safe, injectable autologous collagen, which later evolved into current products [13,14]. Hyaluronic acid, as a routine component of intraocular surgery, has demonstrated its effectiveness, safety and biocompatibility. Modifications of its initial molecule, with cross-linking, have helped to maintain its persistence and effect over the time. After many intraocular implants, lenses with polymethylmethacrylate and polypropylene haptics have shown not to generate an inflammatory reaction and have laid the foundations for the use of this material as an injectable dermal filler [15].
Palpebral Anatomy
The eyelids consist of an anterior and a posterior lamella, the orbital septum marking the division of these two structures at the level of the upper eyelid. The anterior lamella is made up of skin and orbicularis muscle, while the tarsus and conjunctiva form the posterior lamella. The tarsal plates are responsible for providing structural integrity to the eyelid margin, constituting a fibrous skeleton. The upper tarsal plate measures 10 mm and corresponds to the height of the eyelid crease, while the lower one measures 4-6 mm.
The medial and lateral canthal tendons anchor the tarsal plates to the orbit. The pretarsal and preseptal portions of the orbicularis muscle of each eyelid taper to form the superior and inferior branches of the lateral canthal tendon. Posteriorly, the lateral canthal tendon inserts on the inner surface of the orbital rim, on Whitnall’s tubercle. The rhytids that originate in the lateral canthus, popularly known as “crow’s feet”, are due to the contraction of the orbicularis muscle. The upper eyelid contains only 2 fatty compartments, the preaponeurotic and the nasal, separated by a septum. However, the lower one consists of three fatty compartments: nasal, central and lateral, with the nasal and central compartments separated by Lockwood’s ligament. The levator apparatus superioris consists of the levator palpebrae superioris muscle and the Müllerian muscle, which originates from the anterior. The latter is innervated by the sympathetic nervous system while the levator muscle receives fibers from the superior division of the oculomotor nerve. The confluence of both muscles forms the levator aponeurosis, which inserts into the upper tarsal plate. Fibers from the levator palpebrae superioris muscle insert into the skin 8 to 10 mm above the tarsus [16-20].
Blepharoplasty Indications
Dermatochalasis is excess skin on the eyelids, while steatoblepharon refers to fatty protrusion on the eyelids. Both alterations, present significantly, are an indication for blepharoplasty of both the upper and lower eyelids. Many patients present concomitant eyelid ptosis that will require surgery to advance the aponeurosis of the levator muscle. The most reliable way to detect it is by measuring the distance between the light reflection in the center of the pupil in the primary position and the edge of the upper eyelid, with 4 mm being normal. It is also important to assess the existence of loss of elasticity and increased laxity of the lower eyelid, which may indicate the presence of ectropion. This pathology can be evaluated using the snap-back test, through which the lower eyelid is moved away from the sclera and released suddenly. The eyelid may return to its previous position slowly or even not move, indicating that additional surgical treatment such as canthopexy or lateral canthoplasty may be necessary [21-24].
Blepharoplasty Surgical Technique
Upper eyelid blepharoplasty consists of a wedge-shaped skin resection. The lower limit of the skin incision approaches the point of the supratarsal crease, extending 4 to 5 mm above the medial and lateral canthus with its highest point in the center of the line, lying 10 mm above the eyelid margin. The upper limit of the skin incision is marked as a gentle curve that follows the natural upward inclination of the eyelid and orbit. It is determined intraoperatively by pinching the skin of the upper eyelid and should leave 10 to 15 mm of skin between the eyebrow hairs and the skin wrinkle, as this will prevent lagophthalmos due to excess skin resection. The blepharoplasty marks can be extended approximately 1 cm lateral to the lateral canthus to remove the skin remnant. As variants of the technique, partial resection of the orbicularis muscle can be additionally performed as well as the elimination of the fatty compartment, mainly medial in the case of upper eyelid blepharoplasty [25,26]. Lower eyelid blepharoplasty consists of the dissection of a skin and muscle flap, with removal of preaponeurotic fat and the optional performance of a canthoplasty to horizontally tighten the eyelid. In young patients without excess skin or muscle, the fat can be removed through a transconjunctival incision, with no scars on the skin. In these patients, lateral canthoplasty is normally not necessary as there is no eyelid laxity [27,28].
Materials and Methods
This is a bibliographic review, where the articles were searched in three databases for health sciences: Pubmed, ScienceDirect and Cochrane Library. The following search equations were used after defining the study keywords: lasers AND blepharoplasty, non-surgical blepharoplasty, blepharoplasty NOT surgery, laser AND blepharoplasty, peels AND blepharoplasty, fillers AND blepharoplasty, platelet-rich plasma AND blepharoplasty, ptosis AND blepharoplasty.
Inclusion Criteria
i. Articles from Pubmed, ScienceDirect and Cochrane Library databases.
ii. Articles in English or Spanish.
iii. Full text articles.
iv. Articles that talk about the treatment of the periocular skin region, in direct association or not with blepharoplasty.
v. Articles with publication years from 2000 onwards.
Flow Diagram
Materials and Methods
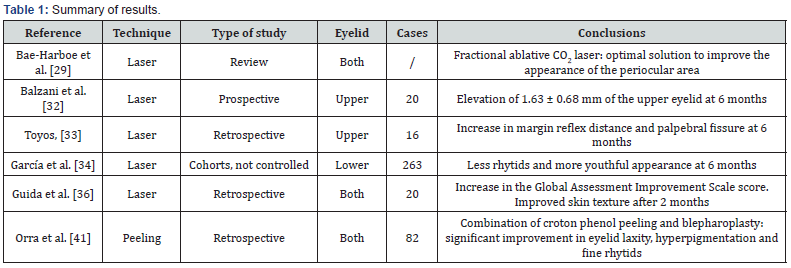
Laser
Laser treatments have proved to be useful in the management of periocular cutaneous morphological and functional changes. Its objective is to generate tissue contraction that produces a smoother and more toned appearance to the skin, being able to optimize the surgical results of a conventional blepharoplasty [29].
There are different laser technologies that can be used in the eyelid region, which include: ablative CO2 laser, erbium-doped yttrium-aluminum-garnet (Erb: YAG) laser (in fractional and continuous modalities) and non-ablative fractional laser [29,30]. The main difference between ablative and non-ablative lasers is the depth of penetration, dose and effectiveness, which tends to be greater in ablative lasers. However, these present greater risks and involve a longer recovery time. Fractional lasers are associated with a lower risk of abnormal scarring, dyschromia and infections, as well as a shorter healing time for the treated skin.
The ablative CO2 laser has historically been considered the gold standard for skin resurfacing. The study carried out by Bae- Harboe et al [29] provides an exhaustive analysis of advantages, disadvantages and potential adverse effects of the different modalities of laser therapies and positions the ablative CO2 laser as an effective treatment to improve the aesthetic appearance of the periocular area. This constitutes an effective way to treat eyelid dermatochalasis and generates greater tissue contraction and improvement of the rhytids compared to ablation produced by the Erb: YAG [30] laser. Fitzpatrick et al [31] demonstrated that both lasers (CO2 and Erb:YAG) produced similar degrees of skin tightening. However, the Erb:YAG laser produced scars in 33% of patients and a lower coagulation capacity compared to the CO2 laser.
Several studies talk about the positive effect of laser to treat eyelid skin excess in cases of mild or moderate dermatochalasis. Balzani et al [32] provided satisfactory results with the CO2 laser in a study in which 20 patients were treated in the upper eyelid and eyebrow region with the fractionated ultrapulsed CO2 laser. The mean elevation of the eyelid crease and eyebrow after treatment was 1.63 ± 0.68 mm and 2.30 ± 0.67 at 6 months, respectively. Furthermore, this fractional laser modality showed a reduction in collateral thermal damage thanks to the selective vaporization of the skin, generating a correct contraction of collagen fibers, mild adverse effects and fairly fast recovery times. The edema after the procedure resolved in 1-2 days on average, while the erythema remained until the fourth day. Toyos [33] published a study based on 16 patients with mild dermatochalasis treated with continuous wavelength fractionated CO2 laser. An average increase in the margin-reflex distance of the upper eyelid of 1.5 mm and the palpebral fissure of 1.8 mm was observed 6 months after treatment, with few side effects, these being minor. Garcia and Badin [34] retrospectively analyzed 263 patients with mild inferior dermatochalasis treated exclusively with fractional ablative CO2 laser. They demonstrated an improvement in rhytids and a more youthful appearance of the periocular skin 6 months after treatment, making the laser a good alternative to transcutaneous lower eyelid blepharoplasty.
In 2022, Filippi Sartori et al [35] published an article in which they reported the histological changes that occur in the skin after fractionated CO2 laser treatment, noticing an increase in the concentrations of type I and III collagen one month after skin rejuvenation, with an evident improvement in periorbital rhytids. The treatment of lower eyelid dermatochalasis has also been analyzed by Guida et al [36] in a retrospective study carried out in 20 patients treated with CO2 resurfacing in the periocular area. They demonstrated an increase in the Global Assessment Improvement Scale score and a reduction in skin surface irregularity with improvement in texture at 2 months, validated by 3D image reconstructions.
Periorbital hyperpigmentation is another common reason for consultation by many patients, which is also not the main objective of blepharoplasty surgery. Various treatments can be carried out for its management, including laser. Its etiology can be vascular, pigmentary, structural and/or mixed [37]. Samaan and Cartee [38] and Vrcek et al [39] have carried out an analysis of its possible treatment. First, they propose the Q-switched laser, ideal for the treatment of hyperpigmentation by targeting melanosomes selectively. Second, pulsed light lasers, useful in patients with pigmented lesions of vascular etiology. As the last option and considered the most effective in most cases, resurfacing with ablative or fractional laser. When comparing Erb:YAG to CO2, the former tends to offer more accuracy with less depth of penetration and minimal thermal damage.
The incidence of complications after laser treatment is usually low. Furthermore, if any adverse effect occurs, it is usually minor. It is important to warn patients of the possible appearance of hypo or hyperpigmentation, edema, as well as the risk of infection and abnormal scarring that may cause ectropion. Kim et al [40] analyzed the complications after performing fractional ablative resurfacing with CO2 laser. The results showed a risk of infection of less than 1%, with a higher prevalence due to viral etiology. The most common complication was post-inflammatory hyperpigmentation (10%), resolved in most cases with topical treatment. Visible scars remained in 0.9% of cases. The degree of maximum satisfaction with the treatment was reached in 97% of the patients.
Chemical Peels
Peelings consist of the application of a chemical substance to the skin with the aim of producing desquamation of the stratum corneum, epidermal normalization and general skin remodeling. It can be obtained a significant improvement in the skin quality after a slight recovery period following the procedure. Peels are classified as superficial, medium or deep according to their level of action, while their mechanism will depend on the active ingredient present in it. In a retrospective study carried out by Orra et al [41], the effects of croton phenol peel were studied. It was applied alone or associated with blepharoplasty, either during or after surgery. The results showed that when both techniques were combined there was a significant improvement in upper and lower eyelid laxity, hyperpigmentation and a reduction in fine wrinkles, proving cost-effective with long-lasting results and minimal adverse effects.
Fillers
Fillers are widely used in facial rejuvenation. Recently, they have become an alternative or complement to surgery not only for blepharoplasty, but also for lagophthalmos, volume loss and eyelid retraction or malposition. The injection of different products at the intradermal level constitutes a minimally invasive, titratable, repeatable and, in some cases, reversible procedure. Depending on the source of origin, they are classified as: biological fillers (collagen and hyaluronic acid), synthetic (polylactic acid, calcium hydroxyapatite and polymethylmethacrylate) and autologous (fat). Depending on the duration of effect, they are divided into: short (bovine collagen, < 3 months), medium (hyaluronic acid, 3-12 months), long (calcium hydroxyapatite and polylactic acid, 12-24 months) and very long duration (polymethylmethacrylate and grease). Hyaluronic acid and bovine collagen are considered reversible substances, while polymethylmethacrylate, calcium hydroxyapatite, polylactic acid and fat are not [42].
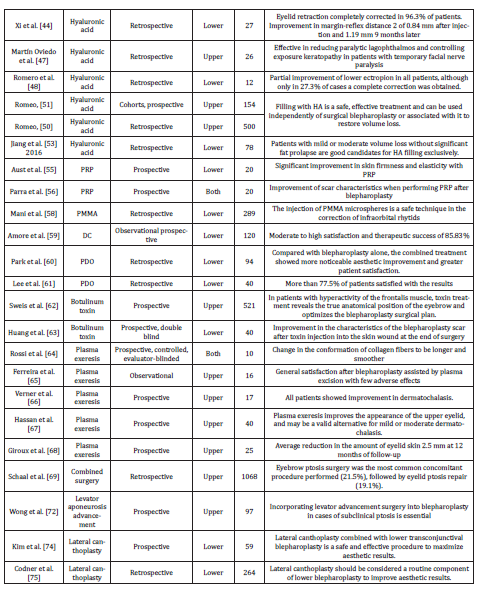
Hyaluronic Acid (HA)
HA derivatives are the most used dermal fillers, since they do not require an allergy test prior to use as they originate from a molecule ubiquitous in the human body. The cross-linking of HA with other chemical substances prevents its enzymatic degradation and gives it a medium-long duration of effect (6-12 months). A wide variety of HA derivatives has been produced over the years, adapting their use to different surgical fields of action, such as eyelid and periorbital pathology. HA injections are an effective treatment to treat upper eyelid retraction adjuvant to blepharoplasty surgery. Leyngold et al [43] showed good clinical results in patients with deep superior palpebral sulcus syndrome. After the injection of Juvéderm® Ultra XC (HA 24 mg/0.8 ml + lidocaine hydrochloride 3 mg/0.8 ml) behind the orbital septum at the level of the superior sulcus in 5 patients, a 70% (2 mm) reduction in lagophthalmos was observed after a mean follow-up of 9.5 months. Lower eyelid retraction secondary to different etiologies can also be treated with HA injections. Xi et al [44] performed an analysis of the physical impact of HA injection below the orbicularis muscle in 27 patients with lower eyelid retraction (14 of them after blepharoplasty surgery). This alteration was completely corrected in 96.3% of the cases, without recurrence in any of them 9 months after treatment, with an improvement in the immediate margin-reflex distance 2 of 0.84 mm on average and 1.19 mm 9 months later.
Lagophthalmos or inability to complete eyelid occlusion can be caused by eyelid retraction (restrictive), paralysis of the orbicularis muscle (paralytic) or proptosis. After blepharoplasty surgery, it is frequently found in the immediate or early postoperative period and usually improves as the edema decreases and eyelid dynamics recover. In patients with septal retractions or excess skin removal, lagophthalmos can become permanent [45]. In severe cases, it may be necessary to reconstruct the anterior lamella with a full-thickness skin graft, but in milder cases, HA fillers may be helpful. Two retrospective studies carried out by Mancini et al [46] and Martín-Oviedo et al [47] in cases of paralytic lagophthalmos talk about the use of Restylane® (HA 20 mg/ml + lidocaine hydrochloride 3 mg/ml) or Juvéderm® Ultra injected into the region of the prelevator and/or pretarsal aponeurosis along the upper eyelid, with good results. It constitutes a useful alternative in patients who are not candidates for surgery and as a temporary measure in those with lagophthalmos in whom functional recovery of the facial nerve is expected, given the reversible nature and slow absorption of HA.
On the other hand, Romero et al [48] analyzed the effects of HA injection in the primary management of cicatricial ectropion, defined as the eversion of the eyelid due to shortening of the anterior lamella because of previous surgeries or trauma, among other causes. The study was based on the injection of 1 mL of Restylane in each eyelid at the infraorbital level in the preseptal area and in the infraciliary region. The results showed a partial improvement in eyelid position in all patients, although only in 27.3% of cases a complete correction was obtained. Due to the unsatisfactory final aesthetic result of several patients, the authors suggested the use of this treatment in patients who are not candidates for surgery.
As we have previously commented, HA injections in the eyelid and upper orbital region can improve the aesthetic appearance of a patient with deep superior sulcus, secondary to periocular aging itself or excess fat removal during surgical blepharoplasty [49]. HA injection in the upper eyelid was compared with surgical blepharoplasty in terms of periocular rejuvenation in two studies carried out by Romeo [50,51] in two cohorts of 154 and 500 patients, respectively. Both studies showed high patient satisfaction and lasting results at a 12-month follow-up, concluding that HA filling is a safe, effective treatment and can be used independently of surgical blepharoplasty or associated with it to restore volume loss [51].
Dark circles are another target of HA treatment to improve the loss of volume in the lower eyelid. In young patients, the pronounced lacrimal groove that produces the dark circle is located in the middle third of the orbital ring, while in older people it extends towards the lateral canthus. To correct this aesthetic alteration, this product is introduced in the preperiosteal plane below the orbicularis muscle [52]. Jiang et al [53] compared the use of HA with autologous fat injections and fat transposition surgery for the treatment of dark circles in 78 patients. Patients with mild or moderate volume loss without significant fat prolapse were good candidates for HA filling alone. However, patients with significant fat prolapses and excess skin showed better results with transposition surgery or autologous fat injections. Diaspro et al [54] also analyzed the treatment of dark circles with HA. They carried out an observational study with 600 patients in which they demonstrated that a single injection of this product could be effective for the treatment of dark circles in patients between 30 and 40 years old, based on a statistical study with inverse correlation between age and aesthetic improvement.
Platelet-rich plasma (PRP)
Aust et al [55] evaluated the use of PRP to treat actinic elastosis and rejuvenate the skin of the periocular area. The study included 20 patients who received 3 injections of 2 mL of PRP in each lower eyelid at monthly intervals. The results showed a significant improvement in skin firmness and elasticity due to increased collagen and elastin production, respectively. In addition, a progressive aesthetic improvement was observed with a high level of patient satisfaction. The side effects of the treatment were minimal, highlighting the mild edema produced after the injection. Parra et al [56] studied the effect of autologous PRP after blepharoplasty surgery through its intradermal application 24 hours, one month and two months after surgery. An improvement in scar characteristics was observed compared to the control group in terms of thickness and flexibility, suggesting the potential therapeutic value of PRP after eyelid surgery. The effect of PRP combined with surgery for the treatment of mild or moderate blepharoptosis has also been investigated in a retrospective study carried out by Shenzhen et al [57] with 36 patients. The results were excellent, remarking its possible use as an adjuvant treatment to surgery.
Polymethylmethacrylate (PMMA)
PMMA is a synthetic, potentially irreversible and long-lasting filler substance. Mani et al [58] analyzed the use of PMMA microspheres in the infraorbital region for the treatment of rhytids in a retrospective case series of 289 patients. The technique proved safe, with natural and predictable results. Only 4 patients developed small granulomas as a minor complication, which resolved after intralesional triamcinolone injection and were correlated with previous blepharoplasty surgery.
Sodium deoxycholate (DC)
DC is an injectable filler substance that has been widely used for the treatment of localized adiposity. Addressing lower eyelid fat pads with monthly injections of 1.25% DC has been studied by Amore et al [59]. After carrying out a multicenter observational study with 120 patients, they showed moderate to high satisfaction and therapeutic success in 85.83% of patients treated with DC at the level of the lower eyelid, with a high degree of effectiveness and few adverse effects. In total, 306 injections were carried out with DC with an average of 2.55 per patient, with a higher success rate observed in patients under 40 years old, which is why they recommended using it preferably in this age group.
Polydioxanone (PDO) Threads
PDO threads are resorbable sutures that stimulate collagen formation and tissue contraction. Its synergistic effect with lower eyelid blepharoplasty has been analyzed in a retrospective study carried out by Park et al [60]. Compared with blepharoplasty alone, the combined treatment showed more noticeable aesthetic improvement and greater patient satisfaction. This improvement was more significant in the reduction of skin wrinkles, the volume restoration of the middle third of the face and the interzygomatic distance, although the combined procedure involved longer surgical time. Lee et al [61] analyzed the effect of PDO threads independently in a group of 40 patients aged 25 to 56 years old, observing the benefits and effectiveness of this technique to treat pronounced infraorbital sulcus without fat protrusion, with more than 77.5% of satisfied patients.
Neuromodulators
Botulinum toxin type A (BT-A), as the main neuromodulator, is widely used to reduce dynamic wrinkles by relieving tension on the adjacent skin by weakening or paralyzing selected muscles. Since its approval for the treatment of wrinkles in the glabellar region in 2002, its use has spread within the field of aesthetics for the treatment of the frontalis, corrugator supercilii and orbicularis muscle. Sweis et al [62] conducted a retrospective study in patients who underwent blepharoplasty. Those with hyperactivity of the frontalis muscle at rest were treated with 15- 20 units of Botox® Cosmetic two weeks before surgery. After the neuromodulator procedure and before blepharoplasty surgery, of the total of 521 patients, 39 with eyelid ptosis and 131 with eyebrow ptosis were detected. Therefore, this procedure proved capable of unmasking pathology concomitant to dermatochalasis, revealing the true anatomical position of the eyebrow and thus optimizing the surgical plan to also correct the associated eyelid or eyebrow ptosis.
BT-A has also been used to improve scar quality, used synergistically with lower eyelid blepharoplasty, as demonstrated by a study carried out by Huang et al [63]. In this prospective clinical trial, botulinum toxin injections were performed in the lateral orbicularis muscle, immediately after suturing the wound at the end of surgery. The width of the scar was significantly smaller compared to the control group in the postoperative period, without additional complications.
Plasma exeresis
Plasma exeresis is a technique based on a handpiece that produces ionic energy and generates heating of the superficial tissue without direct contact. In recent years it has become a non-surgical alternative to dermatochalasis. This limited and controlled thermal damage transforms the solid matter into a gaseous state, generating mild coagulation, increasing collagen formation and skin contraction. Studies carried out by Rossi et al [64] provide a histological explanation for what happens in the skin after treatment with plasma technology. Using confocal microscopy, they observed the induction of a change in the conformation of collagen fibers with the production of smoother and elongated fibers.
Ferreira et al [65] showed promising results of this treatment in a cohort of 16 patients who underwent upper blepharoplasty using plasma technology. Their prospective study provided high patient satisfaction with few associated adverse effects. Vernel et al [66] and Rossi et al [64] showed comparable results in patients treated with plasma exeresis to correct excess upper eyelid skin. Furthermore, a significant decrease in eyelid laxity after treatment was found by Hassan et al [67] in a study carried out on 40 patients. Finally, Giroux et al [68] conducted a study in which 25 patients with moderate dermatochalasis were treated with plasma exeresis, obtaining an average reduction in the amount of eyelid skin of 2.5 mm at 12 months of follow-up, with satisfaction levels of up to 80%.
Surgery
Most patients undergoing blepharoplasty require a combined surgical procedure to correct periorbital involutional changes. A detailed preoperative evaluation is essential to choose the most appropriate surgical technique in each case, which can determine the final aesthetic result. Schaal et al [69] conducted a retrospective study in which they evaluated patients who had undergone upper eyelid blepharoplasty and a complementary surgical procedure. Of a total of 1.068 interventions, only blepharoplasty was carried out exclusively in 31% of them. Eyebrow ptosis surgery was the most common concomitantly performed procedure (21.5%), followed by eyelid ptosis repair (19.1%).
Eyebrow Lift
The normal male eyebrow sits on the orbital rim and is relatively flat, while the female eyebrow is located above the orbital rim and is arched in the temporal part. If the patient is young and shows no evidence of brow ptosis, upper eyelid blepharoplasty is the obvious choice for the treatment of dermatochalasis. However, if the eyebrow is ptotic, there are three alternatives: raising the entire eyebrow, the temporal portion of it (with or without blepharoplasty), or performing only the blepharoplasty at first. The decision will depend largely on the patient’s expectations. If the eyebrow is low and the patient wants a purely aesthetic result, a suitable option would be to elevate the forehead through an endoscopic or coronal lifting. With this surgery, the entire forehead is elevated and its furrows and glabellar folds are eliminated. However, if the primary goal is visual function, direct eyebrowplasty is preferable. Another alternative in men with deep furrows on the forehead is the endoscopic or midfrontal lifting, removing a horizontal strip or two ellipses of tissue from the central portion of the forehead. The majority of patients over 50 years of age have an element of temporal eyebrow ptosis that would be resolved simply with a direct temporal eyebrowplasty, being a useful complement to upper eyelid blepharoplasty [70].
Correction of Eyelid Ptosis
Eyelid ptosis is commonly detected in association with dermatochalasis in many patients undergoing blepharoplasty surgery. Its identification is key since surgical management will involve additional procedures to the removal of excess skin. Eyelid ptosis is defined as a decrease in the margin-reflex distance of the upper eyelid, the lower eyelid or the palpebral fissure, with normal values being 4, 5 and 9 mm, respectively. The levator function is the most important determination to establish the type of ptosis. In the case of involutional ptosis, the levator function is good, the skin wrinkle of the upper eyelid is high, and a drooping of the eyelid occurs when looking down. Surgery in these cases will require an operation to advance the aponeurosis of the levator muscle [71].
In certain patients, eyelid ptosis does not meet the numerical criteria that characterize it, but there are indirect signs that denote its presence; this is what is known as subclinical eyelid ptosis. This is defined as the existence of a normal superior margin-reflex distance and symptoms or signs of hyperactivation of the frontal muscle with ocular opening. This pathology is very prevalent in patients from certain geographic areas, such as the Asian continent. Its identification is crucial before performing upper blepharoplasty, since concomitant levator muscle advancement surgery will optimize its results. Wong et al [72] conducted a prospective study in which 97 Asian patients with subclinical eyelid ptosis underwent blepharoplasty with complementary levator muscle advancement surgery, obtaining a more predictable aesthetic and functional result for the surgeon and satisfactory for the patient.
Lateral Canthoplasty
When there is a component of eyelid laxity, the eyelid should be tightened if any skin and muscle resection is planned. The operation indicated for this purpose is the lateral tarsal strip using a procedure similar to that performed during involutional ectropion surgery [73]. This operation usually needs to be performed in combination with lower eyelid blepharoplasty, obtaining good results with few complications [74]. Codner et al. [75] conducted a retrospective study of 264 patients in whom reinsertion of the lateral canthal tendon was routinely performed using canthopexy, canthoplasty, and suspension of the orbicularis muscle. Of the total, only 9 patients required a second intervention due to eyelid malposition, so they concluded that the treatment of eyelid laxity should be considered routine in all cases of lower eyelid blepharoplasty (Table 1).
 >
>
Discussion
Aging of the eyelid and periorbital region can be treated using a wide variety of medical and surgical procedures that, used in association with blepharoplasty, can optimize its results. Laser treatment of the periocular area gives the skin a smoother, luminous and more toned appearance [29], in addition to treating hyperpigmentation [38,39]. By causing the contraction of collagen fibers, the fractional CO2 laser raises the height of the eyelid crease and the position of the eyebrow, increases the margin-reflex distance of the upper eyelid and softens periocular rhytids [33,34]. This can be useful in patients with mild or moderate dermatochalasis and is presented as an ideal complement to blepharoplasty with the aim of correcting not only excess skin but also improving its quality. It could even be considered in patients with dermatochalasis who do not wish to undergo surgery and are content with a partial improvement in periocular aesthetics. With a similar purpose, peels are presented, which improve eyelid laxity, hyperpigmentation and fine wrinkles, being a cost-effective treatment that is postulated in association with surgery to optimize its results [41], without the need for additional technology as required by the laser treatments.
In relation to fillers, HA is useful for restoring volume in the treatment of patients with a deep upper palpebral sulcus, either due to excess skin resection during surgery, aging itself or atrophy of the orbital fat. When it produces lagophthalmos and exposure keratopathy (alterations that define the syndrome), HA injections improve eyelid closure and therefore the associated symptoms [43,51]. At the level of the lower eyelid, HA improves dark circles in patients with a pronounced tear groove. In very advanced cases, grafts or fat transposition surgery are necessary for significant aesthetic improvement [52,53]. Lower eyelid retraction secondary or not to blepharoplasty also improves with HA infiltration, as observed with the margin-reflex distance [44]. As a more occasionally used filler material, PMMA microspheres improve skin wrinkles when used in the infraorbital region [58], while DC injections are useful in addressing the fatty compartments of the lower eyelid region [59]. PDO threads restore the volume of the middle third of the face, the interzygomatic distance and reduce skin wrinkles when used in conjunction with blepharoplasty surgery [60]. Furthermore, it has been shown that they independently improve the pronounced inferior tear groove [61], also a target of the treatment with HA injections.
As the main neuromodulator, botulinum toxin contributes to blepharoplasty surgery thanks to two well-differentiated functions. On the one hand, its use in patients with hyperactivity of the frontal muscle at rest shows the true anatomical position of the eyebrow. In this way, it allows us to assess before surgery whether blepharoplasty alone will correct the patient’s aesthetic alteration or whether eyebrow or eyelid ptosis surgery will be necessary in a complementary manner [62]. On the other hand, like intradermal PRP treatment, the toxin improves the quality of the scar and can be injected for this purpose at the end of surgery [63].
Similar to the results observed with lasers, plasma exeresis technology produces tissue contraction and improves mild or moderate dermatochalasis, and can even reduce excess skin [65- 68]. Before surgery, an adequate preoperative study is an essential requirement to achieve optimal results after blepharoplasty. Subclinical eyelid ptosis, much more common in Asian patients, must be detected with the aim of performing simultaneous levator advancement surgery, with one of the studies even establishing a formula to determine the amount of levator advancement based on the need of ptosis correction, elevation of the eyebrow with opening and ocular dominance [72]. It is also necessary to determine if the position of the eyebrow is adequate or whether its height should be corrected during surgery. At the level of the lower eyelid, a lateral canthoplasty will improve the results of blepharoplasty as there is almost always a certain component of eyelid laxity [74-75].
Conclusion
The eyelid region has been and will always be considered one of the main therapeutic targets of aesthetic treatments. Surgery tends to be the first choice to provide radical, long-term change in cases of more severe dermatochalasis. However, there are numerous techniques and tools currently available that can produce improvements in mild or moderate disorders. Less invasive and non-surgical options have been growing in the last decade, with the aim of achieving a comparable result while limiting risks, complications and recovery time. Lasers, peels, fillers, PDO threads and new technologies are destined to shape the future in modern aesthetic medicine by improving surgical results when used in combination. Certain intraoperative procedures have also been associated with blepharoplasty, providing a significant final aesthetic improvement.
References
- De Biasio F, Miotti G, Zingaretti N (2019) Study on the aging dynamics of the periorbital region: from observation to knowledge of physiopathology. Ophthalmic Plast Reconstr Surg 35(4): 333-341.
- Baroni A (2020) Non-surgical blepharoplasty with the novel plasma radiofrecuency ablation technology. Skin Res Technol 26: 121-124.
- Drolet BC, Sullivan PK (2014) Evidence-based medicine: Blepharoplasty. Plast Reconstr Surg 133(5): 1195-1205.
- Zoumalan CI, Roostaeian J (2016) Simplifying blepharoplasty. Plast Reconstr Surg 137(1): 196e-213e.
- Wolfort FG, Kanter WR (1995) History of blepharoplasty. Wolfort FG, Kanter WR, eds. Aesthetic blepharoplasty. Boston, Mass: Little Brown & Co.
- Dupuis C, Rees TD (1971) Historical notes on blepharoplasty. Plast Reconstr Surg 47(3): 246-251.
- Graf D (1836) Oertliche erbliche Erschlaffung der Lidhaut. Wochenschrift fur die gesammte Heikunde.
- Spadoni D, Cain CL (1989) Facial resurfacing using the carbon dioxide laser. Am Operating Room Nurses J 50(5): 1009-1013.
- Weinstein C (1994) Ultrapulse carbon dioxide laser removal of periocular wrinkles in association with laser blepharoplasty. J Clin Laser Med Surg 12(4): 205.
- Kaufman R, Hibst R (1990) Pulsed 2.94 um Erbium: YAG laser skin ablation: Experimental results and first clinical application. Clin Exp Dermatol 15(5): 389-393.
- Carruthers JDA, Carruthers JA (1992) Treatment of glabellar frown lines with C. botulinum – an exotoxin. J Dermatol Surg Oncol 18(1): 17.
- Keen M, Blitzer A, Aviv J, Prystowsky J, Smith H, et al. (1994) Botulinum toxin A for hyperkinetic facial lines: results of a double-blind, placebo-controlled study. Plast Reconstr Surg 94(1): 94-99.
- DeVore DP, Fagien S, Kelman CD (1993) Autologous injectable dermal collagen. In Bosniak S (ed): Principles and Practice of Ophthalmic Plastic and Reconstructive surgery, London, W.B. Saunders, pp. 670-675.
- Fagien S (2000) Facial soft tissue augmentation with injectable autologous and allogeneic human tissue collagen matrix (Autologen and Dermalogen). Plast Reconst Surg 105(1): 362.
- Cohen SR, Holmes RE (2004) Artecoll: A long-lasting injectable wrinkle filler material. Report of a controlled, randomized, multicenter clinical trial of 251 patients. Plast Reconstr Surg 114(4): 960.
- Sand JP, Zhu BZ, Desai SC (2016) Surgical anatomy of the eyelids. Facial Plast Surg Clin North Am 24(2): 89-95.
- Rankin BS, Arden RL, Crumley RL (2009) Lower eyelid blepharoplasty. In: Papel ID, Frodel J, Holt GR, et al, editors. Facial plastic and reconstructive surgery. (3rd edition). New York: Thieme; pp. 271-273.
- Branham G, Holds JB (2015) Brow/upper lid anatomy, aging and aesthetic analysis. Facial Plast Surg Clin North Am 23(2): 117-127.
- Ridgeway JM, Larrabee WF (2010) Anatomy for blepharoplasty and brow-lift. Facial Plast Surg 26(3): 177-185.
- Most SP, Mobley SR, Larrabee WF (2005) Anatomy of the eyelids. Facial Plast Surg Clin North Am 13(4): 487-492.
- Papadopulos NA, Hodbod M, Henrich G, Lazlo K, Othon P, et al. (2019) The Effect of Blepharoplasty on Our Patient's Quality of Life, Emotional Stability, and Self-Esteem. J Craniofac Surg 30(2): 377-383.
- Bhattacharjee K, Misra DK, Deori N (2017) Updates on upper eyelid blepharoplasty. Indian J Ophthalmol 65(7): 551-558.
- Neves JC, Medel Jiménez R, Arancibia Tagle D, Luz Maria V (2018) Postoperative Care of the Facial Plastic Surgery Patient-Forehead and Blepharoplasty. Facial Plast Surg 34(6): 570-578.
- Kokubo K, Katori N, Hayashi K, Jun S, Akiko F, et al. (2019) Evaluation of the eyebrow position after aponeurosis advancement. J Plast Surg Hand Surg 53(1): 60-64.
- Yang P, Ko AC, Kikkawa DO, Bobby SK (2017) Upper eyelid blepharoplasty: Evaluation, treatment, and complication minimization. Semin Plast Surg 31: 51-57.
- Rodrigues C, Carvalho F, Marques M (2023) Upper Eyelid Blepharoplasty: Surgical Techniques and Results-Systematic Review and Meta-analysis. Aesthetic Plast Surg 47(5): 1870-1883.
- Bhattacharjee K, Ghosh S, Ugradar S, et al. (2020) Lower eyelid blepharoplasty: An overview. Indian J Ophthalmol 68(10): 2075-2083.
- Murri M, Hamill EB, Hauck MJ, Douglas PM (2017) An Update on Lower Lid Blepharoplasty. Semin Plast Surg 31(1): 46-50.
- Bae-Harboe YS, Geronemus RG (2014) Eyelid tightening by CO2 fractional laser, alternative to blepharoplasty. Dermatol Surg 40(Suppl 12): S137-S141.
- Fathi R, Pfeiffer ML, Tsoukas M (2015) Minimally invasive eyelid care in dermatology: medical, laser, and cosmetic therapies. Clin Dermatol 33(2): 207-216.
- Fitzpatrick RE, Rostan EF, Marchell N (2000) Collagen tightening induced by carbon dioxide laser versus erbium: YAG laser. Lasers Surg Med 27(5): 395-403.
- Balzani A, Chilgar RM, Nicoli M (2013) Novel approach with fractional ultrapulse CO2 laser for the treatment of upper eyelid dermatochalasis and periorbital rejuvenation. Lasers Med Sci 28(6): 1483-1487.
- Toyos MM (2017) Continuous wave fractional CO2 laser for the treatment of upper eyelid dermatochalasis and periorbital rejuvenation. Photomed Laser Surg 35(5): 278-281.
- Garcia CP, Badin AZD (2019) Treating excess lower eyelid skin without incisions. Aesthetic Plast Surg 43(5): 1320-1325.
- De Filippi Sartori J, Osaki TH, Osaki MH (2022) “Split-Face” Evaluation of collagen changes induced by periorbital fractional CO2 laser resurfacing. Aesthet Surg J 42(3): 239-248.
- Guida S, Nisticò SP, Farnetani F, Ester DD, Nathalie De C, et al. (2018) Resurfacing with ablation of periorbital skin technique: indications, efficacy, safety, and 3D assessment from a pilot study. Photomed Laser Surg 36(10): 541-547.
- Michelle L, Pouldar Foulad D, Ekelem C, Nazanin S, Natasha AM (2021) Treatments of periorbital hyperpigmentation: a systematic review. Dermatol Surg 47(1): 70-74.
- Samaan CB, Cartee TV (2022) Treatment of periorbital vascularity, erythema, and hyperpigmentation. Facial Plast Surg Clin North Am 30(3): 309-319.
- Vrcek I, Ozgur O, Nakra T (2016) Infraorbital dark circles: a review of the pathogenesis, evaluation and treatment. J Cutan Aesthet Surg 9(2): 65-72.
- Kim JS, Ginter A, Ranjit-Reeves R (2021) Patient satisfaction and management of postoperative complications following ablative carbon dioxide laser resurfacing of the lower eyelids. Ophthalmic Plast Reconstr Surg 37(5): 450-456.
- Orra S, Waltzman JT, Mlynek K, Duraes EFR, Kundu N, et al. (2015) Periorbital phenol-croton oil chemical peel in conjunction with blepharoplasty: an evolving technique for periorbital facial rejuvenation. Plast Reconst Surg 136(4S): 99-100.
- Tan P, Kwong TQ, Malhotra R (2018) Non-aesthetic indications for periocular hyaluronic acid filler treatment: a review. Br J Ophthalmol 102: 725-735.
- Leyngold IM, Berbos ZJ, McCann JD, Brett P, Ariel RL, et al. (2014) Use of hyaluronic acid gel in the treatment of lagophthalmos in sunken superior sulcus syndrome. Ophthalmic Plast Reconstr Surg 30: 175-179.
- Xi W, Han S, Feng S, Ke Li, Beniamino B, et al. (2019) The injection for the lower eyelid retraction: a mechanical analysis of the lifting effect of the hyaluronic acid. Aesthetic Plast Surg 43(5): 1310-1317.
- Morax S, Touitou V (2006) Complications of blepharoplasty. Orbit 25(4): 303-318.
- Mancini R, Taban M, Lowinger A, Tanuj N, Angelo T, et al. (2009) Use of hyaluronic acid gel in the management of paralytic lagophthalmos: the hyaluronic acid gel “gold weight”. Ophthalmic Plast Reconstr Surg 25(1): 23-26.
- Martín-Oviedo C, García I, Lowy A, Miguel A, Bartolome S (2013) Hyaluronic acid gel weight: a nonsurgical option for the management of paralytic lagophthalmos. Laryngoscope 123(12): E91-E96.
- Romero R, Sanchez-Orgaz M, Granados M, Alvaro A, Ananda C, et al. (2013) Use of hyaluronic acid gel in the management of cicatricial ectropion: results and complications. Orbit 32(6): 362-365.
- Hoenig J, Hoenig D (2013) Minimally invasive periorbital rejuvenation. Facial Plast Surg 29: 295-309.
- Romeo F (2019) Upper eyelid filling approach technique: state of the art after 500 consecutive patients. Aesthetic Plast Surg 43: 663-672.
- Romeo F (2016) Upper eyelid filling with or without surgical treatment. Aesthetic Plast Surg 40(2): 223-235.
- Montes JR (2012) Volumetric considerations for lower eyelid and midface rejuvenation. Curr Opin Ophthalmol 23(5): 443-449.
- Jiang J, Wang X, Chen R, Xueying X, Sai S, et al. (2016) Tear through deformity: different types of anatomy and treatment options. Postepy Dermatol Alergol 33(4): 303-308.
- Diaspro A, Calvisi L, Sito G (2022) Hyaluronic gel injection for the treatment of tear through deformity. A multicenter, observational, single-blind study. Aesthetic Plast Surg 46(4): 1860-1867.
- Aust M, Pototschnig H, Jamchi S, Kay-Hendrik P (2018) Platelet-rich plasma for skin rejuvenation and treatment of actinic elastosis in the lower eyelid area. Cureus 10: e2999.
- Parra F, Morales-Rome DE, Campos-Rodríguez R, Maria Elisa DS (2018) Effect of platelet-rich plasma on patients after blepharoplasty surgery. Orbit 37(2): 81-86.
- Gao S, Li C, Yi M, Baixue L, Rong Z, et al. (2023) Application of surgery combined with platelet-rich plasma in the correction of mild to moderate blepharoptosis. J Craniofac Surg 34(7): e710-e713.
- Mani N, McLeod J, Sauder MB, Daniel NS, Marcella RB (2013) Novel use of polymethyl methacrylate (PMMA) microspheres in the treatment of infraorbital rhytids. J Cosmet Dermatol 12(4): 275-280.
- Amore R, Sbarbati A, Amuso D, Leonardi V, Alsanafi S, et al. (2019) Non-surgical treatment of lower eyelid fat pads with an injectable solution acid deoxycholic based. J Biol Regul Homeost Agents 33: 109-114.
- Park JH, Jeong JW, Park JU (2024) Advanced Facial Rejuvenation: Synergistic Effects of Lower Blepharoplasty and Ultrasound Guided Mid-Face Lift Using Polydioxanone (PDO) Threads. Aesthetic Plast Surg 48(9): 1706-1714.
- Lee W, Oh W, Kim HM, Ben-Li C, Eun-Jung Y (2020) Novel technique for infraorbital groove correction using multiple twisted polydioxanone thread. J Cosmet Dermatol 19(8): 1928-1935.
- Sweis IE, Hwang L, Cohen M (2018) Preoperative use of neuromodulators to optimize surgical outcomes in upper blepharoplasty and brow lift. Aesthet Surg J 38(9): 941-948.
- Huang YL, Wallace CG, Hsiao YC, Mei-Ching L, Jung-Ju H, et al. (2021) Botulinum toxin to improve lower blepharoplasty scar: A double-blinded, randomized, vehicle-controlled clinical trial. Aesthet Surg J 41(9): 1003-1010.
- Rossi E, Farnetani F, Trakatelli M, Silvana C, Giovanni P (2018) Clinical and confocal microscopy study of plasma exeresis for nonsurgical blepharoplasty of the upper eyelid: a pilot study. Dermatol Surg 44(2): 283-290.
- Ferreira FC, Sathler CSCO, Hida IY, Alessandra AK, Ana Clara VC, et al. (2021) Upper eyelid blepharoplasty using plasma exeresis: evaluation of outcomes, satisfaction, and symptoms after procedure. J Cosmet Dermatol 20: 2758-2764.
- Verner I, Naveh HP, Cotofana S (2020) A novel ablative radiofrecuency microplasma nonsurgical blepharoplasty for dermatochalasis. Dermatol Ther 33(6): e13717.
- Hassan AM, Rady AAE, Shalaby OE, Heba MS, Engi Seif ES (2022) Evaluation of plasma exeresis as a new technique for non surgical treatment of dermatochalasis. J Dermatolog Treat 33: 1017-1022.
- Giroux PA, Hersant B, SidAhmed-Mezi M, Chiara P, Simone La P, et al. (2019) The outcomes assessment of the plasma blade technology in upper blepharoplasties: a prospective study on a series of 25 patients. Aesthetic Plast Surg 43(4): 948-955.
- Schaal LF, de Souza Meneghim RL, Padovani CR, Schellini SA (2022) Upper eyelid blepharoplasty and associated ancillary procedures to improve cosmesis. J Fr Ophtalmol 45(1): 53-56.
- Lyon DB (2010) Upper blepharoplasty and brow lift: state of the art. Mo Med 107(6): 383-390.
- Lee TY, Shin YH, Lee JG (2020) Strategies of upper blepharoplasty in aging patients with involutional ptosis. Arch Plast Surg 47(4): 290-296.
- Wong CH, Hsieh MKH, Mendelson B (2024) Subclinical Upper Eyelid Ptosis in Asian Patients: The role of levator advancement in optimizing outcomes in "cosmetic" upper blepharoplasty. Aesthetic Plast Surg 48(2): 141-151.
- Naik MN, Honavar SG, Das S, Savari Desai, Niteen D (2009) Blepharoplasty: an overview. J Cutan Aesthet Surg 2(1): 6-11.
- Kim JY, Kim JI, Choi HG, Ki Il U, Dong Hyeok S (2014) Efficacy of lateral canthoplasty combined with transconjunctival lower blepharoplasty in young asian patients. Arch Plast Surg 20(3): 155-159.
- Codner MA, Wolfli JN, Anzarut A (2008) Primary transcutaneous lower blepharoplasty with routine lateral canthal support: a comprehensive 10-year review. Plast Reconstr Surg 121(1): 241-250.






























