Retrobulbar Injection with Chlorpromazine Versus Cryotherapy in Eyes with Absolute Glaucoma. Two Years of Experience in China
Medina Perdomo Juan Carlos1*, Ling Yang2#, Li Hua Sun2# and Hong Rui Wu3#
1Doctor in Medicine, Master in Science, Assistant Professor of Ophthalmology, Qinghai Aier Eye Hospital, Xining city. China
2Doctor in Medicine, Ophthalmology Specialist, Principal Professor, Qinghai Aier Eye Hospital, Xining city, China
3Ophthalmology Resident, Qinghai Aier Eye Hospital, Xining city, China
#Department of Cataract and Glaucoma, Qinghai Aier Eye Hospital, Xining city, China, Xiguan Street No, 59, Chengxi District, Xining City, Qinghai Province, Xining City Medical College, China
Submission:August 31, 2024;Published:September 11, 2024
*Corresponding author:Juan Carlos Medina Perdomo, Xining #17. Xining Hua Yuan. Xining City. Qinghai Province. China
How to cite this article: Medina Perdomo Juan Carlos, Ling Yang, Li Hua Sun, Hong Rui W. Retrobulbar Injection with Chlorpromazine Versus Cryotherapy in Eyes with Absolute Glaucoma. Two Years of Experience in China. JOJ Ophthalmol. 2024; 11(4): 555817.. DOI: 10.19080/JOJO.2024.11.555817
Abstract
problems faced by the Ophthalmologist at present. Enucleation or evisceration should not be considered at present as the definitive treatment; there are other treatment options whose objective is to temporarily reduce or eliminate pain and reduce ocular tension levels.Material and Method: A comparative - prospective study in eyes of patients with painful absolute glaucoma seen at the glaucoma clinic of a provincial hospital in China during the period of two years (2021 to 2023) with the aim of comparing the results of treatment by retrobulbar injection with chlorpromazine versus freezing cryotherapy. Sixty-four eyes were studied, by systematic random selection and applying inclusion and exclusion criteria, thus forming two groups: 32 undergoing the procedure with retrobulbar injection of chlorpromazine (ICR) and 25 eyes treated with cryotherapy. With the data obtained, a database was created in Microsoft Excel, which was processed by the SPSS version 11.5 statistical program.
Results: Sixty-four eyes with painful absolute glaucoma were studied, with a higher representation of the male sex and the age group 66 to 76 years old. In the group treated with IRA there was greater efficacy in the percentage of pain reduction at two years of the study (72.4%). The mean ocular pressure reduction from baseline to two years was 57.4 for the group treated with CRI with a success rate of 71.8%. For the group treated with cryotherapy the success rate was 59.3%, a statistically significant difference was demonstrated (p=0.001 and p=0.0033) respectively. The number of hypotensive medications was significantly reduced, and most eyes did not require further pharmacological treatment after six months in both procedures p= 0.002. Palpebral edema and conjunctival chemosis were the most prominent with the use of both techniques. The number of associated complications was slightly higher in eyes treated with cryotherapy.
Conclusion: Male patients predominated, in elderly patients. RCI and cryotherapy proved to be effective methods for pain relief in patients with painful absolute glaucoma, being more effective the procedure with Chlorpromazine which showed a higher long-term IOP control, and with a higher success rate, having an additional effect on intraocular pressure control. Most of the eyes treated with both techniques did not require pharmacological therapy after six months of treatment. Few complications and adverse effects were reported with both procedures, being higher in eyes treated with cryotherapy.
Keywords: Retrobulbar Injection; Absolute Glaucoma; Cryotherapy; Blind; Painful Eye
Abbreviations: IOP: Intraocular Pressure; ICR: Retrobulbar Injection with Chlorpromazine; CR: Cryotherapy; RCI: Retrobulbar Chlorpromazine Injection; OT: Ocular Tension; AG: Absolute Glaucoma; AAOPM: American Academy of Pain Medicine; LH: Slit Lamp
Introduction
Blind and painful eye is an entity characterized by irreversible damage to the eyeball and in spite of currently having a powerful and varied therapeutic arsenal for the treatment of glaucoma, many eyes affected by this optic neuropathy reach its most advanced stage in which vision is totally lost, which is known as absolute glaucoma [1].
The treatment of severe and prolonged pain in blind eyes is one of the problems facing the ophthalmologist today. Enucleation or evisceration is usually the definitive treatment, but since a glaucoma blind eye usually has an aesthetically acceptable structure, the patient often decides to keep his eye, although there are other therapeutic alternatives for some patients who are clinically or psychologically unfit to undergo removal of their eyeball [2,3].
There are other less invasive therapeutic options such as retro bulbar injection with chlorpromazine, cryotherapy of the ciliary body (cyclocriotherapy) etc. Chlorpromazine is a neuroleptic drug frequently used in psychiatric conditions. The mechanism of pain relief seems to be independent of the decrease in intraocular pressure and is not yet well defined, believed to be due to a membrane stabilizing effect on the ciliary ganglion or to cell lysis caused by the concentration of the drug [4]. Ciliary body cryotherapy (cyclocriotherapy) has been a procedure used with multiple different techniques, with varying levels of success and complications [5,6]. One of the main complications described is the progressive decrease of vision, an element that does not influence these patients [7,8]. The knowledge that the results of this research may provide will serve for a better understanding of the management of patients with painful absolute glaucoma in order to improve their quality of life.
Aier Eyes Hospital in Qinghai province in China sees a significant number of patients with end-stage glaucoma in whom their quality of life is affected by pain and associated ocular hypertension. Taking into account that chronic pain due to absolute glaucoma limits the visual quality of life in these patients and in view of the failure of ocular hypotensive therapy and retro bulbar injection of absolute alcohol, we were motivated to carry out this research looking for other treatment alternatives with the aim of improving the visual quality of life in these patients. In the present research we proposed to evaluate clinical aspects in patients with blind and painful eyes using two surgical procedures according to each case.
Material and Methods
A comparative-prospective study was performed on eyes with painful absolute glaucoma of patients seen in the glaucoma clinic of a provincial hospital in China during a two-year period (2021 to 2023) with the aim of comparing the results of treatment by retrobulbar injection with chlorpromazine versus freezing cryotherapy. Sixty-four eyes were studied, by means of a randomized systematic selection and applying inclusion and exclusion criteria, two groups were formed: 32 eyes submitted to the procedure with retrobulbar injection of chlorpromazine (RCI), and 32 eyes treated with cryotherapy, inclusion, exclusion and exit criteria were applied for both study groups. The effect of each technique was evaluated at one week, one month, three, six and twelve months and then annually until the two-year study was completed. Variables studied were age, sex, pain: evaluated by a 10-point numerical scale: zero, no pain, and 10, the worst pain imaginable. Ocular tension (OT): measured with Goldman Tonometer, expressed in millimeters of mercury (mmHg) and corrected according to the central corneal thickness, topical hypotensive medications (eye drops) before and after the surgical procedure, and complications: which are the conditions that appeared during or after both procedures and the adverse reactions produced in each study group. A database was created with the data obtained in Microsoft Excel, which were processed by the SPSS version 11.5 statistical program.
· Inclusion criteria
*Patients with painful absolute glaucoma of any etiology.
*Patients with painful absolute glaucoma who wished to participate in the study.
· Exclusion Criteria
*Patients with previous filtering surgery in less than 1 year.
*Patients with previous destructive cycloplegic procedure in less than 1 year.
· Exit Criteria
*Abandonment of the follow-up before the three months of the established follow-up.
Procedures
· Intraocular Pressure (IOP): under previous topical anesthesia, fluorescein staining and with Goldmann tonometer coupled to slit lamp (LH), basal IOP was determined in millimeters of mercury (mmHg) before and after treatment in follow-up visits.
· Pain: it was considered present or not, before and after either procedure, on a scale of 0 to 10, from no pain to the worst pain imaginable in intensity.
· Use of Hypotensive Medication: the amount of topical medication used before and after surgical treatment was noted, and those that were maintained after one month were considered.
· Occurrence or Non-Occurrence of Postoperative Complications: it was specified which, if any, were present.
Retrobulbar Chlorpromazine Injection Technique
The technique used in the retrobulbar injection with chlorpromazine included asepsis and antisepsis with 10% povidone iodine, isolation of the surgical field with sterile split drape and retrobulbar anesthetic injection of 1.5ml of 2% lidocaine and 1.5ml of 0.5% bupivacaine at the level of the inferotemporal quadrant with a 26G needle at a depth of about 2cm. The syringe is withdrawn, the needle is kept inserted and a syringe with 25-50mg of chlorpromazine is connected. Finally, the needle is withdrawn, and digital pressure is applied for a few minutes to minimize anterior diffusion of the drug [9].
Cryosurgery is a physical method for the selective destruction of tissues through the action of cooling elements at sub-zero temperatures. Cryodestruction of the ciliary body is an effective treatment, not only to relieve pain and ocular congestion, but also to stabilize intraocular hypertension [10]. The cyclodestructive procedure of cryotherapy by freezing consisted in the application of cryotherapy in the upper 180 degrees paralimbic, with Cryotherapy Probe, with a duration of 45 to 60 seconds per point, and performed in one session, under peri bulbar anesthesia.
Once the procedure was completed, a drop of cycloplegic (atropine 1%), antibiotic eye drops (ciprofloxacin hydrochloride) and antibiotic ointment (tetracycline 1%) were instilled and then the eye was covered with a monocle for 4 hours. After the procedure, analgesia was indicated according to pain intensity. Four hours were established for the observation of vital signs and possible adverse reactions to the medication, after the procedure and before the patient left the hospital. Follow-up was performed at one, three and six months and then regularly at least once a year until the two-year period was completed.
Results
Of the total number of eyes studied in patients with painful absolute glaucoma N = 64, 70.3% were male and 29.7% were female. The mean age of the patients was 75.8 (±7.9) in the age group 66 to 76 years (Table 1).
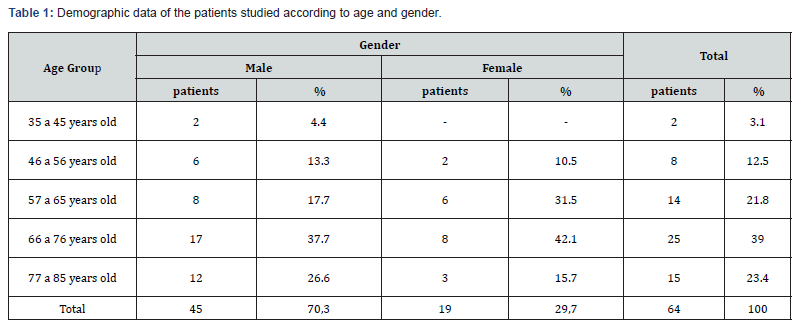
Figure 1 shows a representation of pain before and after each procedure, all patients reported pain prior to treatment, with both procedures the pain component was satisfactorily reduced, which did not show similar results. At three months of follow-up the group treated with ICR presented a decrease in pain reaching 2.5 on the scale and it was maintained uniformly until two years of the study achieving 1.2 on the pain scale, however, the group treated with cryotherapy remained at 5 on the pain scale from one year to reach 5.2 at the end of the study. There were differences in the reduction of the pain scale from the beginning to the end of the study in both groups, for RCI the reduction was 7.1 which represents 72.4%, on a smaller scale a 4.3 decrease in pain (44.3%) for the group treated with cryotherapy. With the application of chlorpromazine 2% of the eyes continued to present pain or discomfort and with the application of cryotherapy 15%.
The mean preoperative IOP value for the group treated with chlorpromazine was 58 mmHg and for the group treated with cryotherapy 54 mmHg, which was modified after the procedure, both for one group and the other, the following month both means decreased to values that although not in the normal range, were less than 30 mmHg. Six months after the procedure the IOP values were considered normal for the group treated with Chlorpromazine (RCI) 21 mmHg, however, the group treated with cryotherapy showed values 25 mmHg out of the normal range. At one year of treatment, the group treated with RCI maintained a mean IOP of 24.5 mmHg which, although out of the normal range, is tolerable in these patients, remaining at levels of 24.5 mmHg at two years of the study, unlike the group treated with cryotherapy that after one year the tendency was to increase with values of 27.1 mmHg, which showed a statistically significant variation (p=0.0001) respectively. The reduction in mean ocular pressure from baseline to two years was 57.4 for the group treated with ICR with a success rate of 71.8% which means that 24 patients out of 32 had an effective decrease in their mean ocular pressure. For the group treated with cryotherapy 19 out of 32 patients achieved a reduction in mean ocular pressure, reaching a success rate of 59.3%.
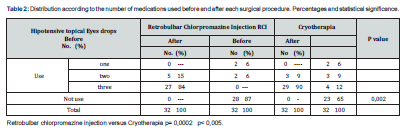
Table 2 shows the distribution of medications used before and after each procedure, where the IOP control obtained by both techniques allowed the reduction of the number of antiglaucomatous medications used by our patients. Most of the treated eyes did not require hypotensive drug therapy after six months of treatment. Those treated with chlorpromazine showed greater benefits for 87% versus 65% of the group treated with cryotherapy. The number of hypotensive drugs combined ranged from 1 to 3 medications with a mean of 3 before each procedure. No patient used a single drug; 27 eyes (84%) in the chlorpromazine-treated group and 29 (90%) in the cryotherapy-treated group used 3 topical drugs without achieving IOP relief or compensation (Figure 2). These figures showed evident variation when six months later 28 eyes in the chlorpromazine group did not require any medication, as well as 23 eyes in the other group. The difference showed statistical significance with p= 0.0002.

At three months only 13 patients experienced worsening of preoperative pain or continued to report discomfort, 4 of them treated with chlorpromazine and 9 with cryotherapy, which led 5 of them to resume hypotensive treatment and 3 to undergo cyclophotocoagulation with diode laser.
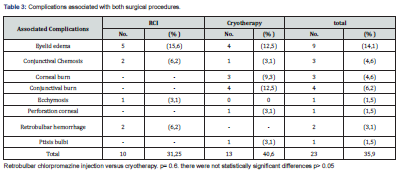
In our study, Table 3 shows the absolute and relative frequencies of the complications presented with each procedure: 10 eyes in the ICR which represents 31.2% for that group and 13 eyes 40.6% in the group treated with cryotherapy. Palpebral edema was the most frequent complication associated with both procedures, ICR 15.6% and cryotherapy 12.5%. Conjunctival (4 eyes) and corneal (3 eyes) burns were transient complications for the cryotherapy group. There was one case of corneal perforation that resolved after two months in the group treated with cryotherapy, this evolved to a Ptisis bulbi after a year and a half, in the group treated with RCI we had two eyes with retrobulbar hemorrhages that resolved in one month after the application of saline solution compresses.
Discussion
Patients with absolute glaucoma have been managed with different procedures, such as intensive antiglaucomatous pharmacological therapy, various surgical procedures including trabeculectomies and valve implants, and pharmacological procedures to control pain, such as retrobulbar injections of alcohol or chlorpromazine. However, the clinical picture remains a challenge for the ophthalmologist because of the severity of the patient's involvement and the anxiety that pain relief generates for the patient and family.
Our study is representative of what is happening nationally in terms of gender in all Chinese provinces there is gender imbalance, especially in Jiangxi, Anhui, and Quinhai, provinces in the central-northern part of the country so that in China there are currently 1.06 men for every woman (53% of men compared to 47% of women) [11,12].
The American Academy of Pain Medicine hypothesizes that since glaucoma is an optic neuropathy, structural damage to the optic nerve may lead to neuropathic damage [13]. Retrobulbar injection of chlorpromazine is an effective treatment for pain, the exact mechanism is unknown, it is believed that this drug causes cell lysis at high concentrations, which produces irreversible changes in the ciliary ganglion and may have a membrane stabilizing effect. Usually one to 2ml (50mg and 80mg) are used, but lower doses suppress systemic effects; in this study the dose of 25mg/ml was used. Chen et al. [4] report that retrobulbar injection of chlorpromazine is a safe and effective form of analgesia when other treatments have failed and surgical intervention is not recommended [4].
The studies of Dr. Nadia Barria and collaborators [14], on the management of glaucomatous blind eye with cryotherapy at the University campus south of Chile do not coincide with the results obtained in our work that although they managed to reduce pain on a scale of 10 (5.2), they did not achieve a significant additive effect in the reduction of ocular pressure from 54 mmHg to 29 mmHg as an average after three years of the study. The studies by Kumar et al. [15] agree with our results in showing that retrobulbar injection with chlorpromazine, in addition to reducing pain, has an additive effect in reducing intraocular pressure [15]. Regarding the reduction of medications, they are similar to those found by V. Pucci et al. [16] who reported a decrease from 4.5 (± 0.5) medications in the preoperative period to 2.38 (± 0.3) at the end of their study [16]. In turn, R. Leszczynski was able to reduce medication consumption from an initial average of 2.8 (± 0.9) to 1.9 (± 0.9) [17].
The complications recorded were mostly transitory and occurred in greater number in eyes of patients with absolute glaucoma of the neovascular glaucoma type, which coincides with other authors [2,4]. Any type of procedure applied is not exempt from complications. The literature reports palpebral edema, conjunctival chemosis, palpebral ptosis, pthisis bulbi, sterile orbital cellulitis, external ophthalmoplegia, Hyphema, nausea, vomiting, brief loss of consciousness and fat necrosis, among others. However, in a blind, red, painful eye with no chance of recovery, complications are rare. In these cases the blood is gradually reabsorbed in a few days and the ptosis and ophthalmoplegia usually disappear in 24-48 hours [18].
Other studies have also described choroidal detachment, vitreous hemorrhage, pan ophthalmitis and even sympathetic ophthalmia [19,20]. In our case the complications presented were transitory and resolved. The patients evolved favorably, in general, after two years of treatment 5 eyes required a second application of cryotherapy and after that the initial symptoms improved considerably, from the procedure with chlorpromazine three eyes required a second application after one year, where the symptoms disappeared, it was also necessary to apply cyclophotocoagulation with diode laser after two years of the study with which the symptoms disappeared.
Conclusion
In the studied eyes of patients with painful absolute glaucoma, the predominant sex was male, in elderly patients. Chlorpromazine retro bulbar injection and cryotherapy proved to be an effective method for pain relief in patients with painful absolute glaucoma, being more effective the Chlorpromazine procedure in pain reduction and showed a higher long-term IOP control, and with a higher success rate, having an additional effect on intraocular pressure control. Most of the eyes treated with both techniques did not require pharmacological therapy after six months of treatment. Few complications and adverse effects were reported with both procedures. The number of associated complications was slightly higher in eyes treated with cryotherapy.
Acknowledgement
The authors certify that this work has not been published and is not under consideration for publication in another journal. They also transfer the copyright of this work to their Journal. The authors complied with the ethical principles of research according to the Helsinki Declaration.
References
- Castillo N Fernando, Perea Gir Mariel, Herrera Norguez Sergio Daniel, Chapela Meneses Rodrigo (2007) Blind and painful eye. Therapeutic options. Do Clin Ter 6: 19-24.
- (2004) Treatment for blind and seeing painful eyes.
- Ferrer Guerra MT, Muguercia González Y (2013) Ciclofotocoagulación transscleral and endociclophotocoagulation . En: Fernández Argones L, Piloto Díaz I, Domínguez Randulfe M. Glaucoma. Surgical themes . La Habana: Medical Sciences.
- Chen TC, Ahn Yuen SJ, Sangalang MA, Fernando RE, Leuenberger EU (2002) Retrobulbar chlorpromazine injections for the management of blind and seeing painful eyes. J Glaucoma 11(3): 209-213.
- Marek Prost (1983) Cyclocryotherapy for Glaucoma. Evaluation of Techniques. Surv Ophthalmol 28(2):93-100.
- Joseph Caprioli, Marvin Sears (1986) Regulation of Intraocular Pressure During Cyclocryotherapy for Advanced Glaucoma. American Journal of Ophthalmology 101(5): 542-545.
- Chiel A, Wind MD (2003) Cyclocryotherapy, cartas al editor. American Journal of Ophthalmology 76(2): 314.
- A Robert Bellows (1981) Cyclocryotherapy for glaucoma. Int Ophthal Clin. Spring 21(1): 99-111.
- Birch M, Strong N, Brittain P, Sandford-Smith J (1993) Retrobulbar phenol injection in blind painful eyes. Ann Ophthalmol 25(7): 267-270.
- CC Murphy, CAM Burnett, PGD Spry, DC Broadway, JP Diamond (2019) A two centre study of the dose-response relation for transscleral diode laser cyclophotocoagulation in refractory glaucoma. Br J Ophthalmol 87(10): 1252-1257.
- https://www.eluniverso.com/2009/11/28/1/1382/china-hay-mas-hombres-mujeres.html.
- gov (2020)The World Fact Book: China. Disponible https://www.cia.gov/library/publications/the world-factbook/geos/ch.html.
- Kavalieratos CS, Dimou T (2019) Gabapentin Therapy for Painful, Blind Glaucomatous Eye: Case Report. Pain Med 9(3): 377-378.
- Barria Nadia, Henrique Elizabeth, Aguirre Mauricio, Unda Marcelo (2017) Eye blind glaucomatous management with cyclocryotherapy. Rev. Medicina y Humanidades. Ophthalmology monographic number.
- Kumar CM, Dowd TC, Hawthorme M (2022) Retrobulbar Clorpromacine Inyectionfor orbital pain relief under difficult circuntances. A case report. Ann Acad Med 35(4): 260-265.
- Puci V, Tappainer F, Borin S, Bellucci R (2003) Long-term follow-up after transscleral diode laser photocoagulation in refractory glaucoma. Ophthalmologica 217(4): 279-283.
- Lesczcynski R, Gierek-Lapinska A, Forminska-Kapuscik M (2004) Transscleral cyclophotocoagulation in the treatment of secondary glaucoma. Med Sci Monit 10(9): 542-548.
- McCulley TJ, Kersten RC (2020) Periocular inflammation after retrobulbar chlorpromazine (thorazine) injection. Ophthal Plast Reconstr Surg 22(4): 283-285.
- Venkatesh P, Gogoi M, Sihota R, Agarwal H (2021) Panophthalmitis following contact diode laser cyclophotocoagulation in a patient with failed trabeculectomy for congenital glaucoma. Br J Ophthalmol 87(4): 508.
- Zeyen T, Vandenberghe K (2019) Miscalibration and severe complications after diode laser cyclophotocoagulation: two case reports. Bull Soc Belge Ophthalmol 292: 27-30.






























