Ocular, Corneal and Internal Wavefront Analysis in Refractive Surgery Candidates
Seyed Javad Hashemian1, Azin Asadzadeh2, Parisa Ahmadian3, Seyed Mahyar Hashemian4, and Sepehr Roozdar1*
1Eye Research Center, The Five Senses Health Institute, Rassoul Akram Hospital, Iran University of Medical Sciences, Tehran, Iran
2Department of Nuclear Medicine, 5azar hospital, Golestan University of Medical Sciences
3Department of Pediatrics, School of Medicine, Children’s Medical Center, Tehran University of Medical Sciences, Tehran, Iran
4School of Medicine, Deparment of Anesthesiology, Tehran University of Medical Sciences, Tehran, Iran
Submission: July 21, 2024; Published: July 30, 2024
*Corresponding author: Sepehr Roozdar, Eye Research Center, The Five Senses Health Institute, Rassoul Akram Hospital, Iran University of Medical Sciences, Tehran, Irance
How to cite this article: Seyed Javad Hashemian, Azin Asadzadeh, Parisa Ahmadian, Seyed Mahyar Hashemian, and Sepehr Roozdar*. Ocular, Corneal and Internal Wavefront Analysis in Refractive Surgery Candidates. JOJ Ophthalmol. 2024; 11(2): 555810; DOI: 10.19080/JOJO.2024.11.555810
Abstract
Purpose: To assess the ocular, corneal and internal higher order aberrations in an adult population who were candidates of laser refractive surgeries with a pyramidal wavefront sensing (PWS) aberrometer (PERAMIS® by SCHWIND eye-tech-solutions GmbH).
Methods: 203 consecutive patients who were referred for refractive surgery between November 2022 and May 2023 to the Iranian Eye Clinic (Private Center, Tehran, Iran) were studied in this descriptive cross-sectional study. Inclusion criteria were age ≥ 18 years old, ≤ 8 D myopia, ≤ 6 D hyperopia and ≤ 6 D astigmatism. Besides thorough ophthalmic examinations, ocular wavefront aberrometry by PERAMIS® (SCHWIND eye-tech-solutions GmbH) preformed for all patients. Mean ± standard deviation (SD) was used to report the results of aberrometry. P values < 0.05 were considered significant.
Results: Mean ocular, corneal and internal HOAs were 0.28 μm, 0.31 μm and 0.29 μm respectively. All the variables including HOA, coma, trefoil and spherical aberration were significantly different between the ocular and the corneal groups (all P values < 0.05). Similar results were found in the comparison of ocular variables with internal variables (all P values < 0.05). Mean of HOAs was higher in >30 y/o group. There was a significant difference between age groups for corneal trefoil, corneal spherical aberration, internal HOA and internal coma (P values: 0.002, 0.001, 0.004 and 0.001 respectively). Mean ocular, corneal and internal HOAs were higher in myopia ± astigmatism group.
Conclusion: In an adult population who were candidates of laser refractive surgeries, ocular measurements of aberrations differed significantly with corneal and internal measurements. Ocular, corneal and internal aberrations increased with age. Mean ocular, corneal and internal HOAs were higher in myopia ± astigmatism group.
Keywords: Wavefront Aberrometry; Refractive Surgery; Refractive Error
Abbreviations: RMS: Root Mean; PWS: Pyramidal Wavefront Sensing; SD: Standard Deviation; TRMS: Total Root Mean Square; HOA: Higher Order Aberrations
Introduction
Advances in aberrometry technology have revolutionized wavefront-based corneal refractive surgery in recent years [1,2]. Excimer laser technology has made it possible to apply wavefront guided treatments for the correction of both lower and higher order aberrations, helping eyes with even more aberrations. Using wavefront analysis, aberrometers determine the refractive parameters of the eye [3]. Wavefront aberration is defined as the departure of a reflected wave from an unaberrated reference wave [4,5]. The most popular metric in use today is the Root Mean (RMS) wavefront error, which is defined as the root square of the wavefront variance over the pupil size of interest [6]. Extremely aberrated eyes have been connected to specific visual anomalies such as glare and halos during low light conditions [7]. The measurement and correction of these wavefront abnormalities can help both with the customization of a refractive procedure and with the improvement of artificially induced aberrations after surgery [8].
Companies that design wavefront aberrometers for use in clinical settings use specific techniques and methods [4,5,9]. The use of such systems is often involved in consultation and decision-making related to refractive surgery [10]. Wavefront aberrometers show the aberration of a light wave after it has passed through the eye’s optical system [11,12]. Zernike and Fourier expansion series polynomials are mathematical tools used in modern optics to quantify aberrations and characterize the optical surface in three dimensions [1]. Every technique has advantages and disadvantages, mainly related to the amount of processing power and optical aberration. A Hartmann-Shack sensor is used by most wavefront-sensing devices that work in tandem with excimer lasers [12,13]. Additional techniques with their own benefits and drawbacks include the Tscherning method, ray tracing, dynamic skiascopy, and pyramidal wavefront sensing (PWS) [11].
In order to assess ocular, corneal and internal aberrations in a normal population who were candidates of laser refractive surgeries, a descriptive cross-sectional study was created. Due to lack of such report with pyramidal wavefront sensing (PWS) aberrometers, PERAMIS® (SCHWIND eye-tech-solutions GmbH) was selected which utilizes PWS to obtain aberrations.
Materials & Methods
Patients
203 consecutive patients who were referred for refractive surgery between November 2022 and May 2023 to the Iranian Eye Clinic (Private Center, Tehran, Iran) were studied in this descriptive cross-sectional study. Inclusion criteria were age ≥ 18 years old, ≤ 8 D myopia, ≤ 6 D hyperopia and ≤ 6 D astigmatism. Patients with abnormal or suspicious tomography, history of previous ocular surgery, trauma or infectious keratitis and systemic diseases such as uncontrolled diabetes mellitus and collagen vascular disorders were excluded. A thorough ophthalmic examination including subjective refraction, best corrected visual acuity, slit-lamp bio microscopy, indirect ophthalmoscopy, corneal tomography by Orbsan® (Bausch and Lomb, Rochester, NY), and ocular wavefront aberrometry by PERAMIS® (SCHWIND eye-tech-solutions GmbH) preformed for all patients. Written informed consent was provided by the participants. The Helsinki Declaration’s guiding principles were followed in this study.
PERAMIS® Aberrometry
PERAMIS® (SCHWIND eye-tech-solutions GmbH) combines a pyramidal wavefront sensor (PWS) with high-resolution topography. In the PWS system, four pupillary images are created when emergent infrared light from the retina is split into four parts by means of an oscillating pyramid [14]. A CCD camera is used to identify and record these images. The aberrations are represented mathematically as Zernike terms, derived from the variations in light intensities of corresponding points on these four images. PERAMIS® employs aberrometry using 45000 measured points in maximum pupillary diameter with a spatial resolution of 41 μm [9,15-17]. The device then displays the eye’s ocular, corneal, and internal aberrations. “Ocular” refers to total aberration of the eye, “corneal” refers to the aberrations originating from the cornea and “internal” refers to the aberrations originating from internal structures of the eye (mainly the crystalline lens and to a lesser extent, the retina and vitreous). PERAMIS® also measures the refractive errors in the range of ± 15.00 D for sphere and ± 10.00 for cylinder. Images were obtained by a single expert technician on the same day, under mesopic condition. At least three image captures were done by the device to obtain the best image quality, selected via own device software.
Satistical Analysis
For describing continuous variables, mean ± standard deviation (SD) was used and if the data was qualitative, frequency and percent was replaced. Independent t-test was used for comparing between subgroups and paired t-test was perfomed for comparing the ocular aberrations with corneal and internal measurements. All of the analysis was done by SPSS 25. P value < 0.05 was considered significant.
Results
After exclusion, 372 eyes of 186 patients were enrolled. 59.6 % were female and 40.4% were male. Mean age was 31.16 ± 7.04 years (ranged from 18 to 59 years old).
Aberrometry
PERAMIS® reports aberrations in three separated categories including ocular, corneal and internal.
Ocular Aberrations
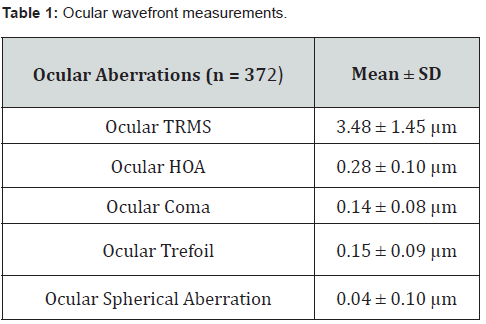
The mean ocular aberrations reported by the device including total root mean square (TRMS), higher order aberrations (HOA), coma, trefoil and spherical aberration are presented in table 1. The mean ocular HOA was 7.2% of mean ocular TRMS. The highest ocular higher order aberration was ocular trefoil (0.15 ± 0.09 μm) followed by ocular coma (0.14 ± 0.08 μm). Ocular spherical aberration was the lowest (0.04 ± 0.10 μm).
Corneal Aberrations
The mean corneal aberrations reported by the device including total root mean square (TRMS), higher order aberrations (HOA), coma, trefoil and spherical aberration are presented in table 2. Corneal HOA was 27.1 % of corneal TRMS. The highest corneal higher order aberration was coma (0.21 ± 0.09 μm) and the lowest was spherical aberration (0.08± 0.13 μm).

Internal Aberrations
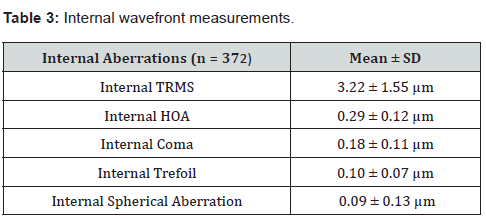
The mean internal aberrations reported by the device including total root mean square (TRMS), higher order aberrations (HOA), coma, trefoil and spherical aberration are presented in table 3. The internal HOA was 8.9% of internal TRMS. The highest internal higher order aberration was coma (0.18 ± 0.11 μm) while the spherical aberration was the lowest (0.09 ± 0.13 μm).
Ocular Aberrations Versus Corneal and Internal Aberrations
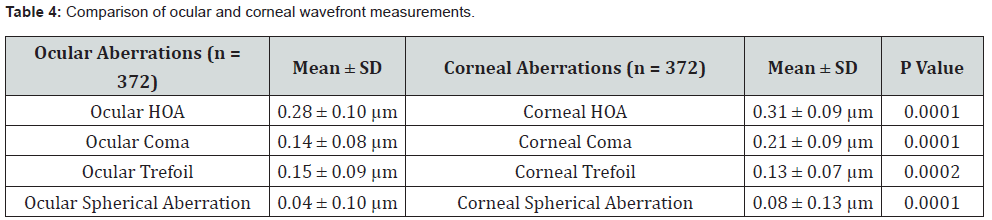
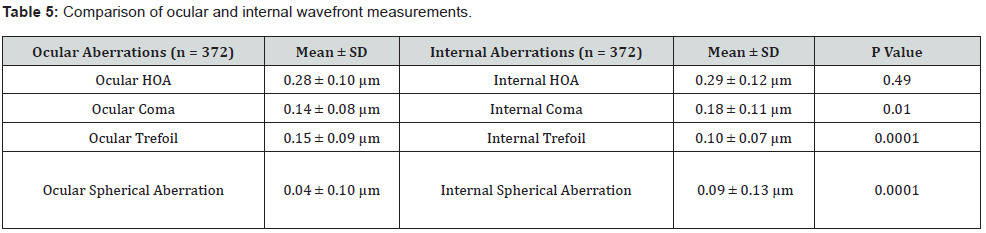
We compared the ocular aberrometry results with the corneal and internal ones. The result of this comparison is shown in tables 4 and 5. All the variables including HOA, coma, trefoil and spherical aberration were significantly different between the ocular and the corneal groups (all P values < 0.05). Similar results were found in the comparison of ocular variables with internal variables (all P values < 0.05).
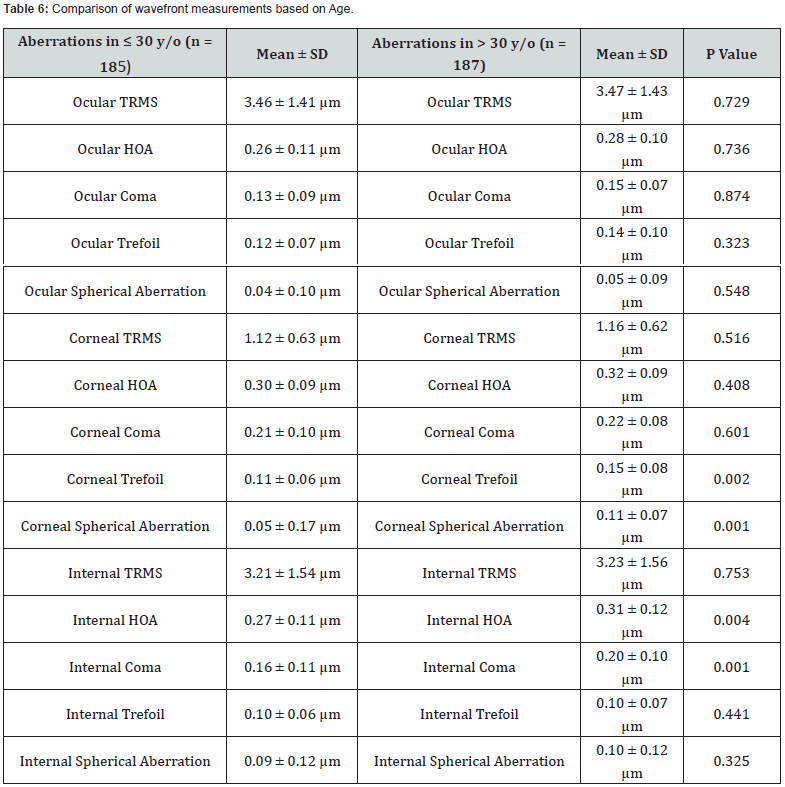
Subgroup Report of Aberrometry: Age
The mean reported aberrations and their comparison according to the age are presented in table 6. Among all variables, the difference of corneal trefoil, corneal spherical aberration, internal HOA and internal coma was statistically significant between two age groups (P values < 0.05). For the other variables, the difference was not statistically significant (P values >0.05).
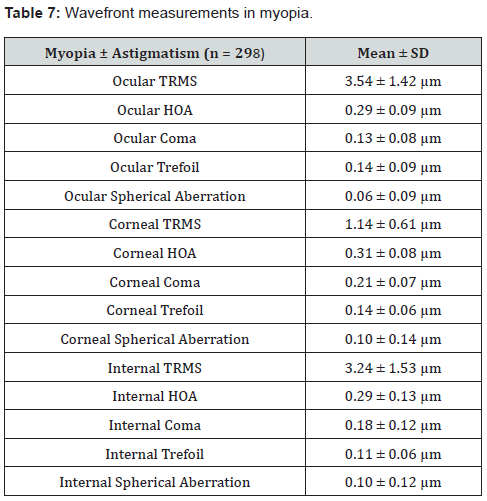
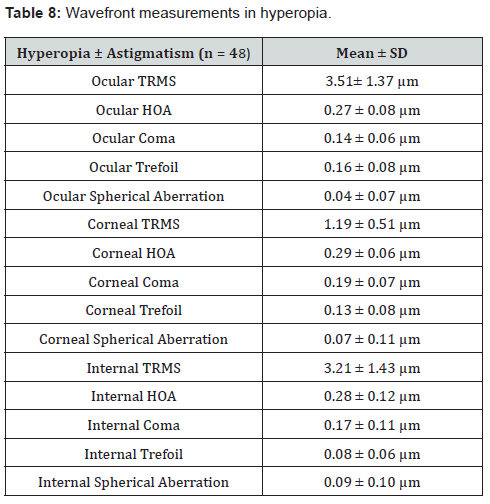
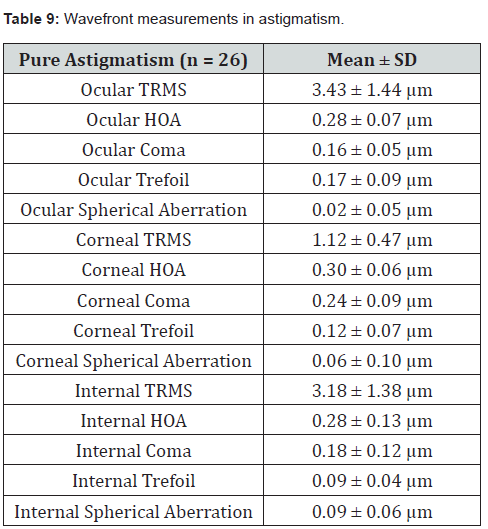
Subgroup Report of Aberrometry: Refractive Error
The mean reported aberrations in three types of refractive errors including (1) Myopia ± Astigmatism, (2) Hyperopia ± Astigmatism and (3) Pure Astigmatism are presented in tables 7,8 and 9.
Discussion
PERAMIS® is a PWS including aberrometer combined with a topographer. The primary benefit of a PWS is its ability to achieve much higher resolution because the wavefront is sampled at the very end of the measuring process. For example, the wavefront is discretized at the lenslet stage by a Hartmann-Shack sensor, and the number of lenses on the lenslet controls the number of measured samples. Typically, a Hartmann-Shack sensor has 1000-2000 lenses with a resolution of 250-1250 μm. In contrast, PERAMIS® boasts a resolution of 41 μm, which equates to 45,000 samples at the maximum pupil size [14-17].
Mean ocular HOA in our study was 0.28 μm. According to earlier research, mean total HOA varies widely from 0.554 μm in the Malaysian population to 0.23 μm in the Caucasian race [18- 26]. These studies utilized Hartmann-Shack based devices to obtain aberrations. The use of various instruments to calculate aberrations and Zernike indices is one of the main issues with comparing results with those of other studies. Comparisons must be done carefully because each study’s participants had different visual and refractive statuses, different age distributions, different measuring instruments, and non-equal pupil sizes in the eyes that were measured. To our best knowledge, there is no report of aberrations with pyramidal wavefront sensing (PWS) devices in an adult population who are candidates of laser refractive surgeries.
In previous works, HOA was reported to be approximately 8-10% of total RMS [27-32]. Except for corneal HOA that was 27.1 % of corneal TRMS, the percentage was 7.2% and 8.9% for ocular and internal HOAs.
The ocular measurements of aberrations were significantly different with the corneal and the internal measurements. It is important to take into account the source of the aberrations because it affects the decision between corneal wavefront guided treatment and ocular wavefront guided treatment. Apparently, when correcting refractive errors, we should take internal aberrations into account.
Age is the most significant variable which correlates with Zernike indices. The correlation between age and aberrations has been shown in numerous studies [19,20,26,33-37]. Our results show that the mean of HOAs was higher in >30 y/0 group than ≤30 y/o group. Although most of the differences were not statistically significant, there was a significant difference between age groups for corneal trefoil, corneal spherical aberration, internal HOA and internal coma (P values: 0.002, 0.001, 0.004 and 0.001 respectively). Age-related increases in coma were noted in previous studies particularly in corneal coma [33]. There was also evidence of this relationship and an age-related increase in trefoil [19]. The increase in ocular aberrations with age appears to be caused by the development of an imbalance between the anterior corneal surface and the internal aberrations [26]. In general, other research has indicated that aberrations increase with aging [20,26]. However, some studies also demonstrate that emmetropization and optical structure reduce age-related aberrations up to the third decade of life, and lens changes cause an increase in ocular aberrations beyond the third decade of life [34,35], as the results of our study show.
According to refractive errors, mean ocular, corneal and internal HOAs were higher in myopia ± astigmatism group than hyperopia ± astigmatism and pure astigmatism groups. In myopia ± astigmatism group, ocular trefoil, corneal coma and internal coma were the highest HOAs in their own categories, while ocular trefoil, corneal coma and internal coma were the highest HOAs in hyperopia ± astigmatism and pure astigmatism groups. Due to lack of an emmetrope group, analyzing how these types of refractive errors impact the aberrations was not possible in our study. There are conflicting findings in this area, despite the fact that the majority of studies claim that myopes have more aberrations. Third-order aberrations were found to be higher in myopia [38], while other research revealed that myopes had higher rates of coma [39]. However, in certain investigations, the aberrations of the various refractive groups did not significantly differ from one another [40]. A significant increase in corneal spherical aberrations with higher degrees of myopia is reported in young adults [41]. Young hyperopic eyes had higher total ocular spherical aberration and third-order aberrations (coma and trefoil) than young myopic eyes, in previous studies [20,42]. However, internal spherical aberration did not differ significantly between the two groups [42].
Small sample size and lack of an emmetrope group to evaluate the impact of refractive errors on aberrations, were limitations of the study.
Conclusion
In an adult population who were candidates of laser refractive surgeries, ocular measurements of aberrations differed significantly with corneal and internal measurements. Ocular, corneal and internal aberrations increased with age. Mean ocular, corneal and internal HOAs were higher in myopia ± astigmatism group.
References
- Cade F, Cruzat A, Paschalis EI, Espírito Santo L, Pineda R (2013) Analysis of four aberrometers for evaluating lower and higher order aberrations. PLoS One 8(1): e54990.
- Cerviño A, Hosking SL, Montes-Mico R, Bates K (2007) Clinical ocular wavefront analyzers. Journal of refractive surgery 23(6): 603-616.
- Lombardo M, Lombardo G (2010) Wave aberration of human eyes and new descriptors of image optical quality and visual performance. Journal of cataract & refractive surgery 36(2): 313-331.
- Howland HC (2000) The history and methods of ophthalmic wavefront sensing. SLACK Incorporated Thorofare, NJ. pp. S552-S553.
- Maeda N (2009) Clinical applications of wavefront aberrometry–a review. Clinical & experimental ophthalmology 37(1): 118-129.
- Pepose JS, Applegate RA (2005) Applegate, Making sense out of wavefront sensing. American journal of ophthalmology 139(2): 335-343.
- Bühren J, Martin T, Kühne A, Kohnen T (2009) Correlation of aberrometry, contrast sensitivity, and subjective symptoms with quality of vision after LASIK. Journal of Refractive Surgery 25(7): 559-568.
- Alió JL, Montés-Mico R (2006) Wavefront-guided versus standard LASIK enhancement for residual refractive errors. Ophthalmology 113(2): 191-197.
- Cook WH, McKelvie J, Wallace HB, Misra SL (2019) Comparison of higher order wavefront aberrations with four aberrometers. Indian Journal of Ophthalmology 67(7): 1030-1035.
- Perrin Marshall D, Acton D Scott, Lajoie Charles-Philippe, Knight J Scott, Lallo Matthew D, et al. (2016) Preparing for JWST wavefront sensing and control operations. in Space Telescopes and Instrumentation 2016: Optical, Infrared, and Millimeter Wave. 2016. SPIE. 9904: 19.
- Vacalebre M, Frison R, Corsaro C, Neri F, Conoci S, et al. (2022) Advanced optical wavefront technologies to improve patient quality of vision and meet clinical requests. Polymers 14(23): 5321.
- Dobos MJ, Twa MD, Bullimore MA (2009) An evaluation of the Bausch & Lomb Zywave aberrometer. Clinical and Experimental Optometry 92(3): 238-245.
- Alberto López-Miguel, Miguel José Maldonado, Arnaldo Belzunce, Jesús Barrio-Barrio, María Begoña Coco-Martín, et al. (2012) Precision of a commercial Hartmann-Shack aberrometer: limits of total wavefront laser vision correction. American journal of ophthalmology 154(5): 799-807.e5.
- Iglesias I, Ragazzoni R, Julien Y, Artal P (2002) Extended source pyramid wave-front sensor for the human eye. Optics express 10(9): 419-428.
- Frings A, Hassan H, Allan BD (2020) Pyramidal aberrometry in wavefront-guided myopic LASIK. Journal of Refractive Surgery 36(7): 442-448.
- Alio JL, D'Oria F, Toto F, Balgos J, Palazon A, et al. (2021) Retinal image quality with multifocal, EDoF, and accommodative intraocular lenses as studied by pyramidal aberrometry. Eye and Vision 8(1): 1-11.
- D'Oria F, Scotti G, Sborgia A, Boscia F, Alessio G (2023) How Reliable Is Pyramidal Wavefront-Based Sensor Aberrometry in Measuring the In Vivo Optical Behaviour of Multifocal IOLs? Sensors 23(7): 3534.
- Carkeet A, Velaedan S, Tan YK, Lee DY, Tan DT (2003) Higher order ocular aberrations after cycloplegic and non-cycloplegic pupil dilation. Slack Incorporated Thorofare, NJ 19(13): 316-322.
- Hashemi H, Khabazkhoob M, Jafarzadehpur E, Yekta A, Emamian MH, et al. (2015) Higher order aberrations in a normal adult population. Journal of current ophthalmology 27(3-4): 115-124.
- Hashemian SJ, Soleimani M, Foroutan A, Joshaghani M, Ghaempanah MJ, et al. (2012) Ocular higher-order aberrations and mesopic pupil size in individuals screened for refractive surgery. International journal of ophthalmology 5(2): 222.
- Lim KL, HB Fam (2009) Ethnic differences in higher-order aberrations: Spherical aberration in the South East Asian Chinese eye. Journal of Cataract & Refractive Surgery 35(12): 2144-2148.
- Nakano EM, Bains H, Nakano K, Nakano C, Portellinha W, et al. (2006) Wavefront analysis in asian-brazilians. 2006, Slack Incorporated Thorofare, NJ 22(9 Suppl): S1024-S1026.
- Netto MV, Ambrósio R Jr, Shen TT, Wilson SE (2005) Wavefront analysis in normal refractive surgery candidates. J Refract Surg 21(4): 332-338.
- Prakash G, Sharma N, Choudhary V, Titiyal JS (2008) Higher-order aberrations in young refractive surgery candidates in India: establishment of normal values and comparison with white and Chinese Asian populations. Journal of Cataract & Refractive Surgery 34(8): 1306-1311.
- Wang L, Koch DD (2003) Ocular higher-order aberrations in individuals screened for refractive surgery. Journal of Cataract & Refractive Surgery 29(10): 1896-903.
- Wei RH, Lim L, Chan WK, Tan DT (2006) Higher order ocular aberrations in eyes with myopia in a Chinese population. J Refract Surg 22(7): 695-702.
- Castejón-Mochón JF, López-Gil N, Benito A, Artal P (2002) Ocular wave-front aberration statistics in a normal young population. Vision research 42(13): 1611-1617.
- Jesson M, P Arulmozhivarman, A Ganesan (2004) Higher order aberrations of the eye in a young Indian population. Asian J. Ophthalmol 6(2): 10-16.
- Lawless MA, Hodge C (2005) Wavefront's role in corneal refractive surgery. Clinical & experimental ophthalmology 33(2): 199-209.
- Porter J, Guirao A, Cox IG, Williams DR (2001) Monochromatic aberrations of the human eye in a large population. JOSA A, 18(8): 1793-803.
- Mirko Resan, Miroslav Vukosavljević, Milorad Milivojevic (2012) Wavefront aberrations. Advance in ophthamology Rijeka. In Tech, pp. 191-204.
- Kalikivayi V, Kalikivayi L, Ganesan AR (2021) Analyses on the distribution and influence of higher-order aberrations both clinically and experimentally among varied refractive errors. Saudi Journal of Ophthalmology 35(1): 21-28.
- Amano S, Amano Y, Yamagami S, Miyai T, Miyata K, et al. (2004) Age-related changes in corneal and ocular higher-order wavefront aberration. Am J Ophthalmol 137(6): 998-992.
- Brunette I, Bueno JM, Parent M, Hamam H, Simonet P (2003) Monochromatic aberrations as a function of age, from childhood to advanced age. Investigative Ophthalmology & Visual Science 44(12): 5438-5446.
- He JC, Sun P, Held R, Thorn F, Sun X, et al. (2002) Wavefront aberrations in eyes of emmetropic and moderately myopic school children and young adults. Vision Research 42(8): 1063-1070.
- Salmon TO, van de Pol C (2003) Normal-eye Zernike coefficients and root-mean-square wavefront errors. Journal of Cataract & Refractive Surgery 32(12): 2064-2074.
- Calver RI, Cox MJ, Elliott DB (1999) Effect of aging on the monochromatic aberrations of the human eye. JOSA A 16(9): 2069-2078.
- Kirwan C, M O’Keefe, H Soeldner (2006) Higher-order aberrations in children. American journal of ophthalmology 141(1): 67-70.
- Buehren T, Collins MJ, Carney L (2003) Corneal aberrations and reading. Optometry and Vision Science 80(2): 159-166.
- Atchison DA, Schmid KL, Pritchard N (2006) Neural and optical limits to visual performance in myopia. Vision research 46(21): 3707-3722.
- Marcos S (2002) Are changes in ocular aberrations with age a significant problem for refractive surgery? Journal of refractive surgery 18(5): S572-S578.
- Llorente L, Barbero S, Cano D, Dorronsoro C, Marcos S (2004) Myopic versus hyperopic eyes: axial length, corneal shape and optical aberrations. Journal of vision 4(4): 5-5.






























