Differential Diagnosis of Enophthalmos: A Case Report of Silent Sinus Syndrome
Denismar Borges de Miranda*, Brenda Cavalieri Jayme and Adriana Cristina Gaeta Aquino Costa
Department of Ophthalmology, Hospital de Base do Distrito Federal, Brazil
Submission: May 25, 2023;;Published:June 07, 2023
*Corresponding author: Denismar Borges de Miranda, Department of Ophthalmology, Hospital de Base do Distrito Federal, Brazil JOJ Ophthalmol
How to cite this article: Denismar Borges de M, Brenda Cavalieri J, Adriana Cristina Gaeta Aquino C. Differential Diagnosis of Enophthalmos: A Case Report of Silent Sinus Syndrome. JOJ Ophthalmol. 2023; 10(1): 555778. DOI: 10.19080/JOJO.2023.10.555778
Abstract
Purpose: To report a rare case of Silent Sinus Syndrome, emphasizing the importance of the differential diagnosis of cases of enophthalmos.
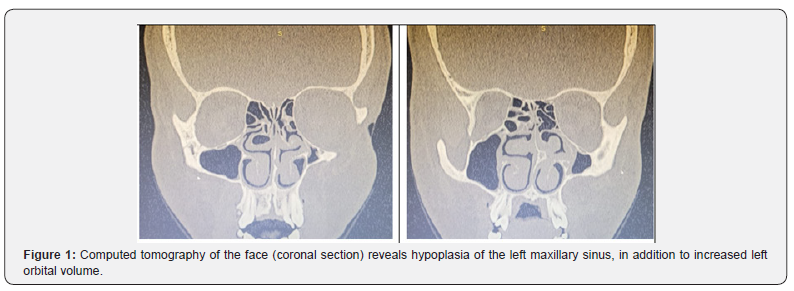
Case Report: JPL, male, 23 years old, refers to low visual acuity in both eyes, worse in the left, associated with an ipsilateral deep eye that started three years ago. He also complains of long-standing nasal obstruction and intermittent rhinorrhea. On examination, he had better visual acuity of 20/30 in the right eye and light perception in the left eye. The bio microscopy of the right eye showed no changes, the left eye showed enophthalmos, total corneal opacity and 360º neovascularization. Investigation of enophthalmos through computed tomography of the face revealed hypoplasia of the maxillary sinus on the left.
Conclusion: SSS, although rare, should always be considered as a differential diagnosis in patients with enophthalmos not justified by other etiologies
Keywords: Silent Sinus Syndrome; Maxillary Atelectasia; Enophthalmos; Case Report
Keywords: Higher Order Aberrations; Lens Dysfunction; Low Vision; Crystalline Lens Removal; Itrace; Refractive Lens Exchange
Introduction
Spontaneous, asymptomatic enophthalmos, not related to trauma or surgery, constitutes a set of findings called Silent Sinus Syndrome (SSS) or implosive antrum syndrome. Reported for the first time in 1964, two cases of enophthalmos secondary to destruction of the orbital floor resulting from asymptomatic mucoceles [1]. Already in 1986 there is a description of the first case of enophthalmos secondary to chronic sinusitis [2].
SSS is a very rare condition, presents as a characteristic a painless enophthalmos associated with volumetric decrease progression of the maxillary sinus causing chronic atelectasis, veiling of the cavity and centripetal displacement of its walls [3-7]. In addition, it comprises as clinical characteristics the asymmetry of the eyes, spontaneous enophthalmos and hypoglobus [4]. Eminently surgical treatment involving two steps: sinus clearance, with functional re-establishment of the drainage route; and reconstruction of normal orbital architecture. The approach can be performed via endonasal route with uncinectomy and endoscopic maxillary antrostomy and removal of obstructive soft tissue [8]. This work aims to report a rare case of Silent Sinus Syndrome, emphasizing the importance of the differential diagnosis of cases of enophthalmos. It is emphasized that the patient's consent to voluntarily participate in the study, and this only started after signing the free and informed consent form.
Case Presentation
JPL, male, 23 years old, comes to the cornea department for evaluation and follow-up for keratoconus. He refers to low visual acuity in both eyes, worse in the left, associated with an ipsilateral deep eye that started three years ago. He also complains of long-standing nasal obstruction and intermittent rhinorrhea. Patient denied previous orbitofacial trauma. On ophthalmologic examination, he had better visual acuity of 20/30 in the right eye and light perception in the left eye. The bio microscopy of the right eye showed no changes, the left eye showed enophthalmos, total corneal opacity and 360º neovascularization. Measurement of intraocular pressure within the normal range. Fundoscopy of the right eye without alterations and not viable in the left eye (corneal opacity). Investigation of enophthalmos through computed tomography of the face revealed hypoplasia of the maxillary sinus on the left, seen in figure 1.
The joint evaluation by the otorhinolaryngology team showed, at rhinoscopy, obstructive septal deviation to the left and at nasal video endoscopy, it revealed the presence of degeneration and edema in the middle turbinate on the left. The multidisciplinary planning included: first, the otorhinolaryngologist will perform the septoplasty with inferior and medial turbinectomy associated with maxillary astrostomy on the left; and later reconstruction of the orbital architecture by ocular plastic surgery. The patient is being followed up at a joint outpatient clinic by ophthalmology (corneal and ocular plastic department) and otorhinolaryngology. There is currently no surgical indication for keratoconus in the right eye and a corneal transplant for the left eye was indicated. With 12 months of follow-up there was no progression of enophthalmos and no worsening of visual acuity.
Discussion
Due to its rarity, studies often highlight confusion surrounding its definition, diagnosis and appropriate treatment. SSS is characterized by maxillary atelectasis, usually unilateral. It has a pathophysiology that is still not very well defined. The probable pathophysiological explanation would be chronic obstruction of the maxillary sinus, which would cause negative pressure and retraction of the sinus walls, consequently leading to enophthalmos and lowering of the orbital floor [4-6]. For the definitive diagnosis of SSS, it is necessary to rule out other causes of enophthalmos, such as trauma, neoplasms, osteomyelitis, lipodystrophies, scleroderma and Parry-Romberg syndrome.
Sporadically, the disease is accidentally found in imaging tests in the investigation of another pathology. As reported in this study, computed tomography (CT) of the paranasal sinuses and orbit was essential for diagnostic confirmation. Already described by other authors, CT is the best radiological examination to observe bone anatomy, being superior to magnetic resonance imaging [4,6,9]. CT in SSS may demonstrate total or partial opacification of the maxillary sinus with or without secretion [9]. Surgical treatment emerges as an important therapeutic option, aiming at better aeration of the compromised maxillary sinus and reconstruction of the orbital floor, when possible. Early intervention can be beneficial in terms of preventing long-term orbital complications and alterations [4,6]. This makes it necessary to evaluate and work together with an ophthalmologist, an otorhinolaryngologist, among others.
Conclusion
Silent Sinus Syndrome, although rare, should always be considered as a differential diagnosis in patients with enophthalmos not explained by other etiologies. Imaging exams are essential to confirm the diagnosis. Multidisciplinary evaluation and management, including ophthalmology and otorhinolaryngology, are fundamental for therapeutic optimization (functional and aesthetic) and improvement of quality of life.
References
- Montgomery WW (1964) Mucocele of the maxillary sinus causing enophthalmos. Eye Ear Nose Throat Mon 43: 41-44.
- Wesley RE, Johnson JJ, Cate RC (1986) Spontaneous enophthalmos from chronic maxillary sinusitis. Laryngoscope 96(4): 353-355.
- Blackwell KE, Goldberg RA, Calcaterra TC (1993) Atelectasis of the Maxillary Sinus with Enophthalmos and Midface Depression. Ann Otol Rhinol Laryngol 102(6): 429-432.
- Cury A de S, Manfrim A, Demeneghi P, Roithmann R, Tesser S (2007) Silent sinus syndrome: case report and literature review. Rev AMRIGS 51(1): 53-57.
- Cobb ARM, Murthy R, Cousin GCS, El Rasheed A, Toma A, et al. (2012) Silent sinus syndrome. Br J Oral Maxillofac Surg 50(6): 81-85.
- Rosso C, Saibene AM, Felisati G, Pipolo C (2022) Silent sinus syndrome: systematic review and proposal of definition, diagnosis and management. Acta Otorhinolaryngol Ital 42(4): 305-316.
- Fonseca FL da, Mazoti L, Polati M (2014) Unusual ocular manifestations of silent sinus syndrome. Rev Bras Oftalmol 73(1): 44-46.
- Chariba I, Lazard DS, Sain OC, Lecanu JB (2014) Correlation between the rate of asymmetry volume of maxillary sinuses and clinical symptomatology in the silent sinus syndrome: A retrospective study about 13 cases. Rev Laryngol Otol Rhinol (Bord) 135(4-5): 197-200.
- Albadr FB (2020) Silent Sinus Syndrome: Interesting Computed Tomography and Magnetic Resonance Imaging Findings. J Clin Imaging Sci 10: 38.






























