Congenital lens dysfunction as a new, undiagnosed cause of decreased visual acuity based on observation over a period of 3 years
Adam Cywinski*, Martyna Michulec, Daria Bloch and Aleksander Lubczyk
Silesian Eye Treatment Centre, Zory, Poland
Submission: May 25, 2023;Published: June 05, 2023
*Corresponding author: Adam Cywinski, Silesian Eye Treatment Centre, Zory, Poland
How to cite this article: Adam C, Martyna M, Daria B, Aleksander L. Congenital lens dysfunction as a new, undiagnosed cause of decreased visual acuity based on observation over a period of 3 years. JOJ Ophthalmol. 2023; 10(1): 555777. DOI: 10.19080/JOJO.2023.10.555777
Abstract
Two groups of patients with diagnosed myopia and astigmatism underwent surgery to have their natural lens removed. The reason of the study was to answer a question if, and how a different level of higher order aberration generated by crystalline lenes, devoid of any visible pathologies can influence visual acuity and quality of vision. A first, examining group, which included 15 patients (29 eyes), had lens removal because of diagnosed lens dysfunction and deteriorated visual acuity to far distances. Second, the control group included 20 patients (31 eyes) with normal visual acuity who had lens removal in the process of refractive lens exchange. The level of higher order aberration generated by the lens examined preoperatively was abnormally higher in examining group as compared with control group. Visual acuity to far distances, measured in examining group was preoperatively deteriorated (mean values = 0.6 logMar) and improved postoperatively (mean values = 0.3 logMar), statistically significantly in contrast to the group undergoing refractive lens exchange, where visual acuity pre and postoperatively comparable.
Background: This article tries to prove that one of the reasons for deterioration of visual acuity, like also quality of vision lies in healthy looking crystalline lens, if it generates high values of higher order aberrations.
Aim of the study: To assess how higher order aberrations, generated by the patient’s healthy-looking lens can influence visual acuity and quality of vision.
Methods: Two groups of patients underwent surgery to have their natural lens removed in the process of refractive lens exchange and congenital lens dysfunction. Congenital lens dysfunction is so far from an undiagnosed cause of deterioration of quality of vision and decreased visual acuity to far distances.
Results: Statistically significant differences were obtained in both preoperative values of higher-order aberration generated by the lens as well as preoperative and postoperative values of visual acuity to far distances. Visual acuity in the group with congenital lens dysfunction improved statistically significantly in contrast to the group undergoing refractive lens exchange.
Conclusions: Lack of visible cause of visual acuity deterioration be an impulse to extend diagnostics to include tests for higher order aberration, generated by the lens.
Keywords: Higher Order Aberrations; Lens Dysfunction; Low Vision; Crystalline Lens Removal; Itrace; Refractive Lens Exchange
Abbreviations: BCVA: Best Corrected Visual Acuity; RE: Right Eye; CLD: Congenital Lens Dysfunction; HOAs: Higher-Order Aberrations; LOAs: Lower-Order Aberrations; RLE: Refractive Lens Exchange
Introduction
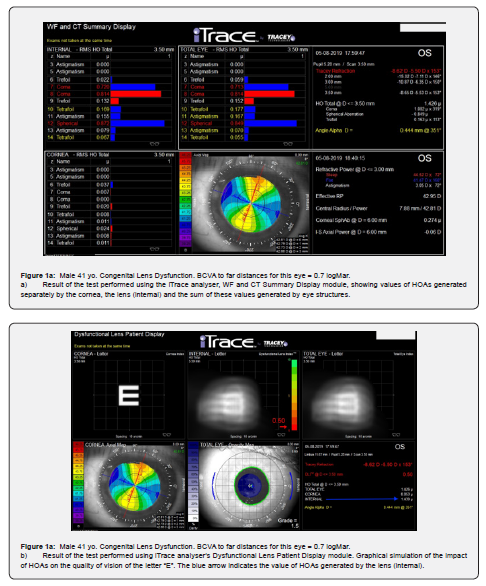
The term “Congenital Lens Dysfunction” (CLD) was introduced by the author of this article to identify the cause of the impairment of visual function in terms of quality of vision and visual acuity to far distances. The underlying pathology is an abnormal lens structure that generates higher-order aberrations (HOAs). A very important element of the diagnosis is the absence of any visible pathologies that could be seen during biomicroscopic examination of the lens. This pathology was discovered thanks to the careful analysis of the test results obtained using the iTraceTM analyzer. This versatile device combining the functions of an aberrometer, and corneal topography allows, among others, for the separate analysis of HOAs generated by the cornea and those generated by the eye lens (Figure 1a, b). The term “Congenital Lens Dysfunction” was first described in the article “Usefulness of iTraceTM in Diagnosing Unclear Cases of the Deterioration in Visual Acuity. Congenital Lens Dysfunction as a New Disease Entity. Preliminary Reports” published in December 2020 [1]. Since then, the author’s view of congenital lens dysfunction has been slightly modified.
The main determinant of the diagnosis of CLD are high values of HOAs generated by the lens, with no obvious structural pathologies. The patients do not have cataracts, lenticonus, or a spherical lens. The patients also do not have any other pathologies, generated by other structures of the eye, cornea, optic nerve, retina. Using the word “congenital”, the author wanted to emphasize that this new term refers to a condition other than the condition of the lens known as “lens dysfunction”, which was introduced to understand the changes that occur in a lens which is undergoing opacification after the age of 40.
Despite the lack of visible pathologies, in most of cases a dysfunctional lens generates large, abnormally high HOA values, which translates into a reduction in the quality of vision and visual acuity to far distances, while maintaining correct vision to near distances. Other abnormalities, the presence of which is necessary in order to make the above diagnosis, include: poor quality of vision from childhood (patient’s medical history), presence of high or moderate myopia with accompanying astigmatism, however myopia is of a mixed, refractive-axial nature. The presence of pathology in the remaining eye structures, i.e., cornea, retina or optic nerve, does not exclude the presence of CLD, but it significantly influences correct diagnosis. Low values of HOAs generated by the cornea greatly facilitate proper diagnosis.
So far, generation of HOAs in the eye optical system has been considered only in the context of evaluation of corneal function, mainly in the processes of qualification to refractive surgery [2,3]. As a reminder, aberrations are divided into lower-order (LOA) and higher-order (HOA) aberrations. LOAs, which account for 85% of all aberrations generated by the optical system of the eye, include commonly known eye defects, including myopia, hyperopia, and regular astigmatism. These aberrations can be easily corrected using glasses or contact lenses [4].
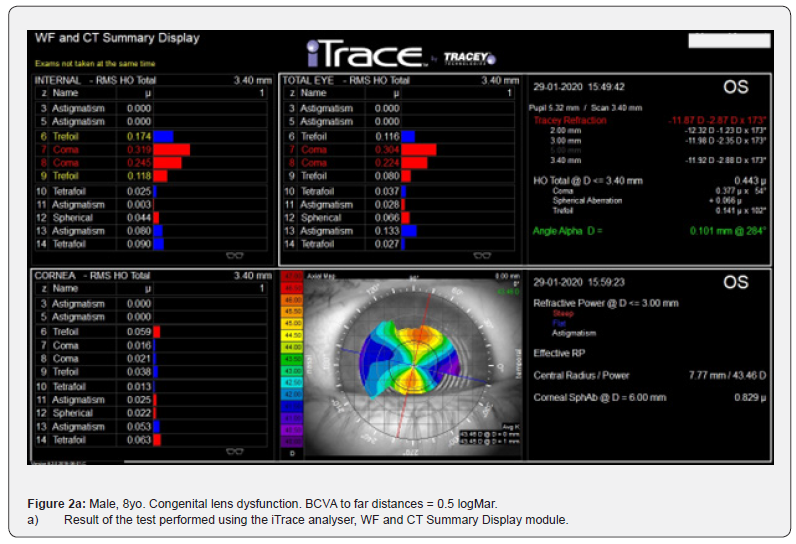
HOAs include, among others, spherical aberration, trefoil, coma, tetrafoil, secondary astigmatism. They are most often written in the form of Zernike polynomials. The existence of HOAs in the optic system of the eye can cause blurry vision, diplopia, decreased contrast, dysphotopsia such as ‘glare’, ‘starbursts’ and ‘halo’, and blurred vision at night. These aberrations have a negative impact on vision, in eyes with a wide pupil, and therefore also in scotopic conditions [5]. The normal ranges of HOA generated by the cornea, depends on the pupil size and are between 0.046-0.338 µm (4mm) and 0.121-0.740 µm (6mm) [6]. The only correlation between the lens and values of HOA were observed in progressive nuclear cataract and concerns spherical aberration [7]. During a 3-year follow up, 59 patients aged 8 to 47, who met the criteria for the diagnosis of “congenital lens dysfunction”, were admitted to the Silesian Eye Treatment Centre (Figure 2a, b). In this group, 15 patients (23 eyes) underwent surgery to remove a dysfunctional lens.

Objective
The aim of the study is to prove the correlation between abnormally high values of HOA generated by the lens, as the only one reason of deterioration of visual acuity, examined preoperatively to far distances, like also correlation between high values of HOA and poor visual quality. A secondary aim is to assess if there is a correlation between normal visual acuity to far distances and low values of HOA, generated by the lens.
Material
Retrospective, comparative analysis of values of HOAs, visual acuity and quality of vision, obtained in two groups of patients. First, the examined group included patients with diagnosed abnormality-congenital lens dysfunction (CLD), second, control group included patients, who were qualified to refractive lens exchange (RLE). The only one abnormality observed in examined group were high values of HOA generated by the lens. 33 people (54 eyes) underwent surgery to remove their natural lens, followed by implantation of an artificial lens into the capsule. 15 patients (23 eyes) formed the examined group and were qualified for surgery to remove the lens due to its dysfunction. The second control group consisted of 20 patients (31 eyes) who wanted to get rid of refractive errors and qualified for refractive RLE (group 2). Because CLD was observed only in eyes with diagnosed myopia and astigmatism, only patients with such eye defects were included into the control group.
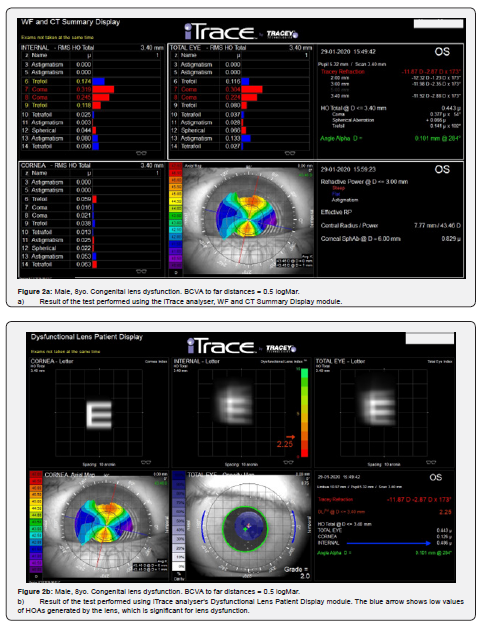
Preoperatively, each patient was examined using the iTraceTM analyser (Trecey® Technologies) version 6.2.0. Average values of HOAs generated by the cornea and the lens were assessed separately. In accordance with the procedure, the examination was repeated three times at short intervals (Figure 3a, b). For each patient, the values of logMar charts (far vision) and Snellen charts (near vision) obtained with best correction were assessed. Considering the subjective assessment of postoperative vision, each participant in both groups was asked about their quality of vision.
Eligibility Criteria for Surgery
Only patients who were diagnosed with myopia and astigmatism were included in the study. Examined group. Patients with abnormally high HOA generated by the lens (INTERNAL) and confirmed deterioration of visual acuity to far distances and concomitant poor quality of vision. There were no pathologies within the cornea, retina, vitreous and lens, which could have a clear impact on the decrease in visual acuity and the quality of vision. Control group Patients, which wanted to be free of eye defect with normal visual acuity too far and near distances after using best correction. Loss of accommodation properties. Another necessary element was to obtain consent for the extraction of the patient’s clear lens was the desire to improve vision in the group with CLD and to get rid of the refractive error in the group undergoing RLE. Only patients whose best corrected visual acuity (BCVA), measured to both far and near distances was normal, were qualified into the group undergoing RLE.
Exclusion Criteria
1. Abnormally high values of HOAs generated by the cornea in both groups. Patients with hyperopia and pure astigmatism.
2. Any pathologies observed in the cornea, retina, optic nerve or vitreous that clearly have a negative impact on visual acuity and the quality of vision.
3. Any visible pathologies in the structure of the lens, i.e., cataracts, lenticonus and keratoglobus, constituted an important exclusion criterion.
4. CLD suspicion in children was also a disqualifying factor, considering the possibility of further growth of the eyeball and thus a change in the scope of the refractive error.
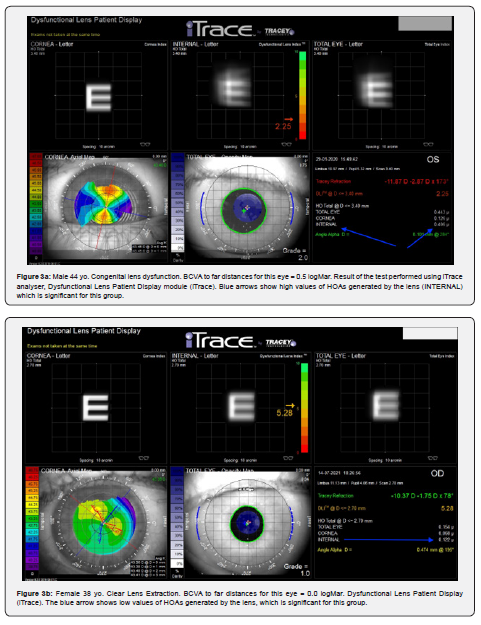
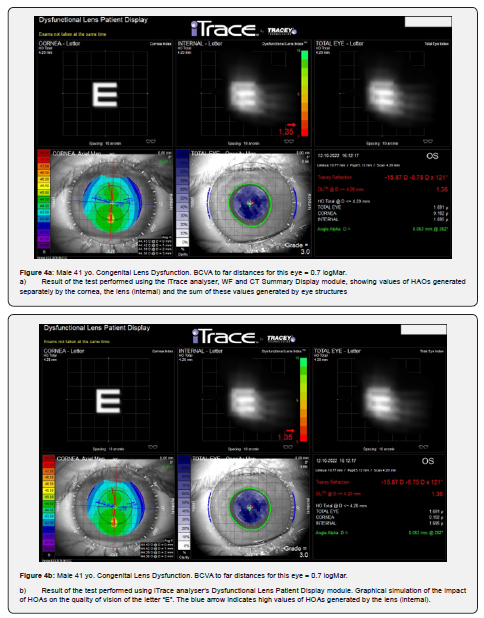
Below is an example of a 4 yr. girl. She was diagnosed because of a very low visual acuity to far distances, observed in both eyes. Refractometry revealed high myopia and astigmatism of the right eye (RE)…….and left eye (LE)………. BCVA to the far in both eyes = 1.4 logMar. BVA without correction, in both eyes, to the near = D-0.5 (from 5cm), axial length: RE = 26.55 mm, LE= 26.28 No pathologies were found in the retina (Electroretinography), optic tract (Visual Evoked Potential), vitreous and cornea. No visible pathologies of the lens were observed. An examination using analyzer iTrace, module “Dysfunctional Lens Patient Display” revealed normal values of HOA generated by the cornea: RE=0.081, LE=0.102mm, and abnormally high HOA generated by the lens: RE=1.695mm, LE=1.695mm (figure 4a, b). Detailed types of HOA generated by above eyes are visible, using module “WF and CT summary display”.
Method
Each patient, apart from basic tests, including refractometry and intraocular pressure measurements, underwent corneal topography, endothelial cell density measurement and macular OCT. Ganglion cells thickness was examined when glaucoma was suspected. Examination of the anterior and posterior segment using direct/indirect bio microscopy, after pharmacological pupil dilation, was an obvious qualifying standard. The patient’s lens was removed using the phacoemulsification or phacoaspiration procedure. Main criteria for choosing intraocular lens have included: a value of preoperative myopia and astigmatism, a value of angle alpha, pupil size, probability to gain good postoperative level of visual acuity to far distances, patient preferences, and economic issue. Because of the above criteria, different types of intraocular artificial lenses was used, including monofocal, bifocal or multifocal toric lenses. All lenses were inserted into the lens capsule. A premium class, toric lens implantation was the surgical standard in the RLE group.
Because we still don’t know how complex structure of intraocular lens can influence the level of HOA, this parameter was not evaluated after lens exchange. Even spherical lens can generate astigmatism, postoperatively [8]. The procedures were performed by one surgeon in a private medical centre - the Silesian Eye Treatment Centre (Zory - Poland)
The following test results were subjected to comparative analysis:
1. Values of HOAs generated by the cornea and the lens (internal HOA) obtained preoperatively in both groups.
2. Values of BCVA to far distances, obtained preoperatively in both groups.
3. Values of BCVA to far distances, obtained before and after surgery in the CLD group.
4. Values of BCVA to far distances, obtained preoperatively and postoperatively in the group undergoing RLE.
5. Values of visual acuity to near distances obtained in both groups, preoperatively and postoperatively.
Additionally, the above results were assessed for the correlation between the values of HOAs generated by the lens and the preoperative values of BCVA to far distances obtained in both groups. In order to assess subjective changes in vision, each patient was asked about changes in the quality of vision and visual acuity to far distances obtained in the postoperative period.
Statistical Analysis
When developing statistical research, the correlation coefficient was examined, then it was checked whether this coefficient is statistically significant. When analyzing the statistical research, the correlation coefficient was considered. At a later stage, it was checked whether this coefficient was statistically significant.
An Information
We haven't asked for approval our institution's ethics committee for this study. Why? Because lens removal is a stable part of every surgery of cataract removal or refractive lens exchange. We haven’t changed the way of lens removal but only a reason.
Results
Analysis of the values of HOAs Obtained
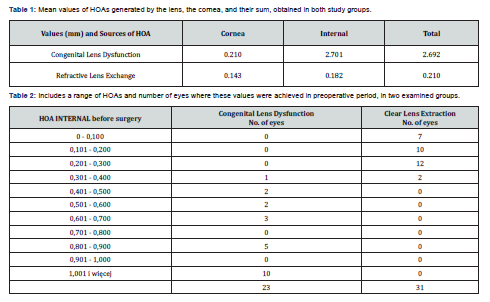
The comparative analysis included averaged values of HOAs generated by the cornea and the lens (HOA internal) and its common value, generated in both groups, obtained in the preoperative period. These values are presented in Table 1. There were no statistically significant differences between the values of HOAs generated by the cornea in both groups. Statistically significant differences were found in the values of HOAs generated by the lens. They were very high in the CLD group. The HOA values obtained in the postoperative period were not analyzed due to the implantation of intraocular lenses of various structures. A range of HOAs and number of eyes where these values were achieved in preoperative period are presented in Table 2.
Visual acuity to far Distances
The mean values of BCVA to far distances obtained preoperatively and 2 months after the procedure in both groups were analyzed. These values are presented in Table 3. A particular value of BCVA, obtained preoperatively to far distances and number of eyes with such parameters are presented in Table 4. No statistical differences were observed in the values of BCVA to far distances obtained in CLE group, in the pre- and postoperative periods. In CLD group, statistically significant differences were found between pre and postoperative visual acuity, measured to far distances. BCVA to far distances improved by an average of 3 lines on logMar charts compared to preoperative visual acuity. Postoperative vision improvement was not achieved in 3 patients (3 eyes) with unilateral high myopia. Patients from CLD group who had preoperative visual acuity to far distances lower than logMar = 0.5 did not achieve full visual acuity to far distances. It is a logical consequence of the presence of an obstacle, practically from birth, which blocked the proper development of vision to far distances, as is the case with amblyopia due to disuse.

Visual Acuity and HOA values
When analyzing the obtained values, statistically significant correlations were found between
1. Normal visual acuity to far distances and low values of HOAs generated by the lens.
2. Deteriorated visual acuity to far distances and high values of HOAs generated by the lens.
3. The mean level of HOA in examining, CLD group was 2.701, as compared with control, CLE group, one the level of 0.182.
Subjective Assessment of Changes in the Quality of Vision
Patients from the CLD Group
Each of the patients undergoing lens extraction bilaterally reported an improvement in acuity and quality of vision. As previously mentioned, three patients with unilateral high myopia did not report an improvement in vision to far distances, only an improvement in the quality of vision. These people have confirmed that they have severe amblyopia.
Patients from RLE Group
Most of the patients did not notice any significant changes in BCVA and quality of vision in relation to the preoperative vision. As usual, there were a few complaints about the occurrence of negative and positive photopsia, seeing circles in the field of vision, related to the artificial lens structure.
Discussion
Lens Dysfunction. This term is synonymous with the progressive opacification of the lens and the resulting changes in vision. The presence of lens opacification, as well as pathologies of other eye structures can be easily diagnosed using appropriate diagnostic methods. Looking at literature on HOAs, no articles were found analyzing the effect of HOAs generated by the lens on the quality of vision and visual acuity. Virtually all articles focus on the descriptions of HOAs generated by the cornea. This is likely due to the lack of access to devices that can separate the aberrations generated by the lens from those generated by the cornea. The iTraceTM analyzer is one of only a few devices used in the world that allows for this type of analysis.
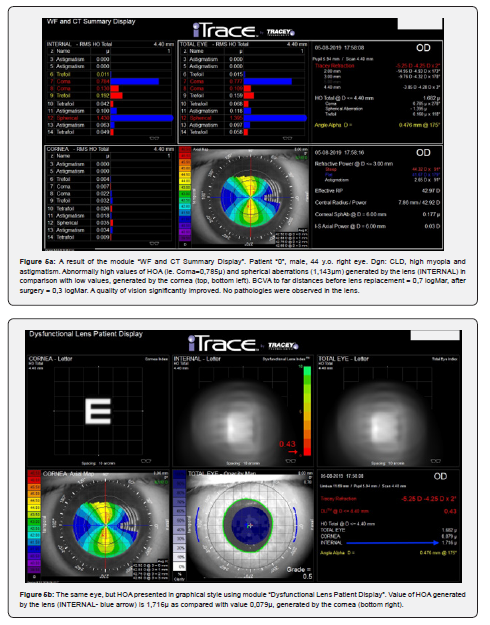
The first patient in whose case it was suspected that the cause of poor quality of vision and visual acuity observed in both eyes had not been described so far was a 44-year-old man. The patient underwent practically all ophthalmological diagnostic tests, and no pathologies were found within the cornea, lens, retina and vitreous body. Also, no pathologies were found in the neurological examination. The patient was diagnosed with myopia accompanied by astigmatism. Despite the use of best correction (right eye -5.0Dsph/-4.25Dcyl, left eye -8.62 Dsph/-5.5Dcyl), visual acuity to far distances did not exceed the value of 0.7 (logMar), with full acuity maintained in vision to near distances (D-0.5 on Snellen charts). Refractometry showed different, smaller values in terms of the size and axis of corneal astigmatism. The axial length of the eyeball indicated that we are dealing with mixed, refractive-axial myopia.
Examination of the eye using the iTraceTM analyzer for HOAs showed enormous values of HOAs generated only by the lens (Figure 5a, b). The patient underwent surgery in both eyes to replace the dysfunctional lens with a bifocal toric lens. There was an improvement in vision to far distances by 4 lines (logMar) and a significant improvement in the quality of vision. The visual acuity measurement repeated after 14 months gave an improvement of one line to far distances. The patient pointed out that the poor quality of vision was noticeable since an early age and that moderate myopia and astigmatism were diagnosed when he was 6.Poor quality of vision since a young age was the main element of vision that patients paid attention to after the extraction of a dysfunctional lens.
The results showed that visual acuity to far distances achieved in the CLD group improved statistically significantly but still has not reached normal values in some patients. Such a situation was observed when preoperative visual acuity to far distances was low and accompanied to abnormally high values of HOA, generated by the lens. This seems logical as the cause of poor vision likely occurred at birth or in early childhood, so vision could not develop properly. That is why the author called this yet unstudied or undescribed pathology ‘Congenital Lens Dysfunction’. There were some patients in the examining group, whose values of BCVA, examined to far distances, were between 0.3 and 0.2 (logMar), and who gained normal visual acuity postoperatively. HOA generated by those lenses, were only slightly elevated (about 400-500m).
A statistically significant correlation between high values of HOAs generated by the lens and abnormal values of visual acuity to far distances was found in the study group despite the absence of any visible pathology within the lens of the eye. Therefore, the question is whether the patient’s natural lens, which does not show any pathologies during ophthalmological examinations, can generate large, abnormal HOA values? The answer is YES, as is the case with the cornea. When evaluating the cornea in bio microscopy, in most cases we cannot know what HOA values it may generate. It is not uncommon that when abnormal visual acuity values are observed and there are no obvious reasons for this, doctors try to match the cause to the diagnosis. This results, among others, in indicating myopia with accompanying astigmatism as the cause of poor vision. As the results of this study show, this is not a good course of action.
Conclusions
Diagnosing poor visual acuity to far distances with good visual acuity to near distances and no visible pathologies within the structures of the eyeball that may cause poor vision, and the presence of moderate and severe myopia with accompanying astigmatism requires the extension of diagnostics to include a test assessing the values of HOA generated by the lens. This abnormal condition may be a consequence of congenial lens dysfunction, a pathology not described so far, the only manifestation of which is the generation of high values of HOA by the natural lens. In the diagnosis of this disease, it is necessary to use a device that allows for the differentiation between higher-order aberrations generated by the cornea and the lens. Such a device is the iTraceTM analyzer.
References
- Cywinski A (2020) Usefulness of Itrace in Diagnosing Unclear Cases of the Deterioration in Visual Acuity. Congenital Lens Dysfunction as a New Disease Entity. Preliminary Reports. Journal of Bioscience & Biomedical Engineering.
- Taskov G, Taskov T (2020) Higher Order Aberrations (HOA) Changes after Femto-LASIK in Topography and Wavefrontguided Treatments. Folia Med (Plovdiv) 62(2): 331-337.
- Anderle R, Ventruba J, Skorkovská Š (2015) Comparison of visual acuity and higher-order aberrations after standard and wavefront-guided myopic femtosecond LASIK. Cesk Slov Oftalmol 71(1): 44-50.
- Kligman BE, Baartman BJ, Dupps WJ (2016) Errors in Treatment of Lower-order Aberrations and Induction of Higher-order Aberrations in Laser Refractive Surgery. Int Ophthalmol Clin 56(2): 19-45.
- Suliman A, Rubin A (2019) A review of higher order aberrations of the human eye. African Vision and Eye Health 78(1).
- Hiraoka T, Kiuchi G, Ueno Y, Oshika T (2018) An attempt to determine the normal range of corneal higher-order aberrations. Investigative Ophthalmology & Visual Science 59(5801).
- Hashemi H, Khabazkhoob M, Jafarzadehpur E, Yekta A, Emamian MH, et al. (2016) Higher order aberrations in a normal adult population. J Curr Ophthalmol 27(3-4): 115-124.
- Cywinski A, Bloch D, Lubczyk A (2022) Assessment of the Value of Astigmatism Generated by Two Models of Spherical Multifocal Lenses: Panoptix® by Alcon® and Acunex® Variomax® by Teleon® using the Toric Alignment Check Module of the Itrace Analyser. Open Access Journal of Ophthalmology 7(2): 000244.






























