Exceptional Etiological Fungal Keratitis with Scedosporium Apiospermum Sensitive to Fluconazole: About One Case
Diagne Jean Pierre1*, Ka Aly Mbara1, Aw Aissatou1, Fall Insa DIAW2, Mbaye Soda1, Sy El Hadji Malick1, Ba Alassane1, Senghor Ousmane1, Diallo Hawo Madina1, Samra Audrey1, De Meideros Marguerite Edith Quenum1 and Ndiaye Papa Amadou1
1University ophtalmological center of Abass Ndao Hospital, Senegal
2Biology department of Abass Ndao Hospital, Senegal
Submission: April 05, 2023;Published: May 07, 2023
*Corresponding author: Diagne Jean Pierre, University ophtalmological center of Abass Ndao Hospital, Senegal
Diagne Jean Pierre, Ka Aly Mbara, Aw Aissatou, Fall Insa DIAW, Mbaye Soda, et al. Exceptional Etiological Fungal Keratitis with Scedosporium Apiospermum Sensitive to Fluconazole: About One Case. JOJ Ophthalmol. 2023; 9(5): 555774. DOI: 10.19080/JOJO.2023.09.555774
Abstract
Purpose: To report a rare case of Scedosporium apiospermum fungal keratitis treated with fluconazole.
Observation: This was a 28-year-old security guard patient received for a painful red right eye with decreased visual acuity. Interrogation revealed an ocular trauma from a foreign body of unknown nature three weeks ago, and treated with topical antibiotics and corticosteroids without improvement. The ophthalmological examination showed to the right eye a visual acuity limited to see the hand move, a diffuse conjunctival hyperemia, a perikeratic circle, an epithelial infiltrate with blurred edge of 4 mm of diameter, para-central, yellowish white. Examination of the left eye was normal. In front of this picture, the patient was hospitalized, and after a two-day therapeutic window, a microbiological examination of corneal scratching was performed, highlighting a filamentous fungus: Scedosporium apiospermum. The patient had received local antifungals (fluconazole 2mg/ml, Betadine 1% eye drops) and general antifungals (fluconazole). The evolution was marked by visual acuity increased to 4/10, and complete healing, at 1 month.
Conclusion: Keratitis with Scedosporium apiospermum are rare and of functional and anatomical prognosis often pejorative due to delayed diagnosis and resistance to common antifungals. Fluconazole is a broad-spectrum, second-generation triazole antifungal. Its preparation for topical instillation, still not widespread, is easy.
Keywords: Keratitis; Mycosis; Antifungal
Introduction
Scedosporium apiospermum is a ubiquitous filamentous fungus found in soil, polluted water and decaying plant material. Scedosporium apiospermum keratitis are rare and most often post-traumatic [1]. Their functional and anatomical prognosis is often pejorative due to delayed diagnosis and resistance to common antifungals [2]. We reported Scedosporium apiospermum keratitis in a patient treated with topical and oral fluconazole.
Observation
This was a 28-year-old patient, security guard, with no particular ophthalmological history. It was received for painful red right eye with decreased visual acuity. Interrogation revealed an ocular trauma from an unknown foreign object, dating back to three weeks. Initially, it was treated with topical antibiotics and corticosteroids in the first host structure, without improvement. Ophthalmological examination on the right showed limited visual acuity to see the hand move, diffuse conjunctival hyperemia, perikeratic circle, purulent secretions, superficial epithelial infiltrate of 4 mm of para-central diameter, yellowish white. Examination of the left eye was without particularity (visual acuity 10/10).
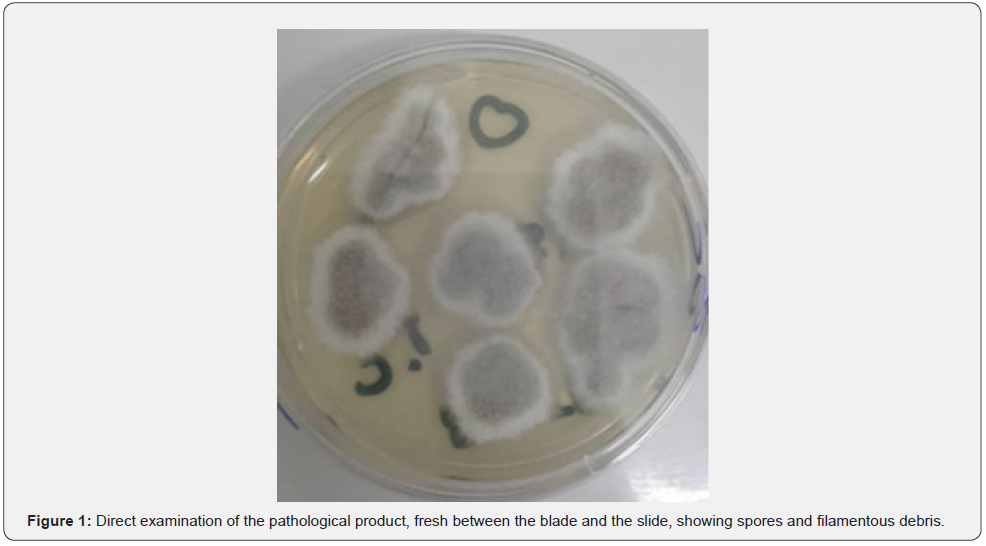
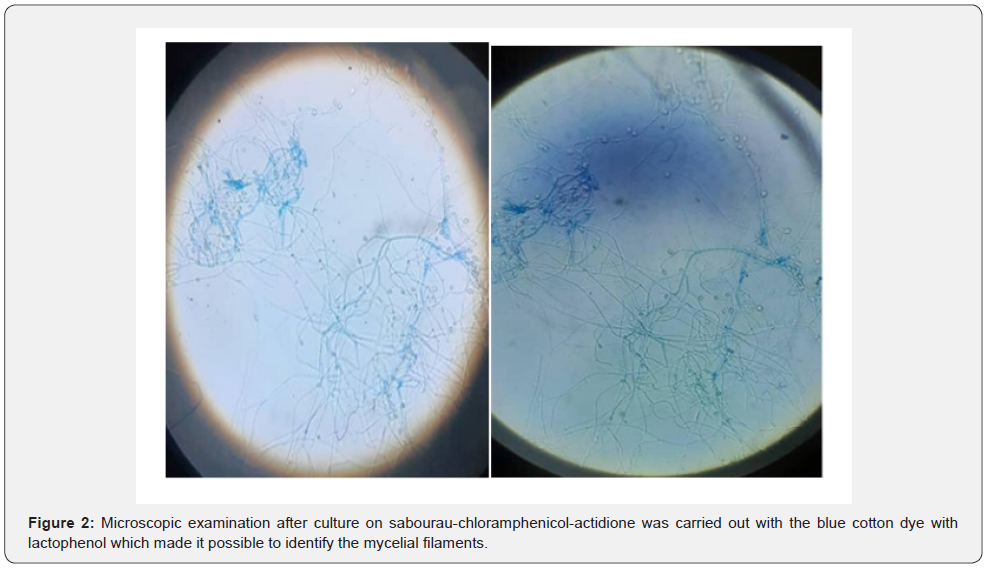
In front of this picture, the patient was hospitalized. After a two-day therapeutic window, a microbiological examination of corneal scratching was done. Before the results of the microbiological examination, a probabilistic treatment with fortified eye drops based on third-generation cephalosporin and vancomycin was introduced, always without improvement. Direct examination of the pathological product was conducted in the fresh state between the blade and the slide, and showed spores and filamentous debris (Figure 1). Microscopic examination after culture on sabourau-chloramphenicol-actidione was carried out with the blue cotton dye with lactophenol which made it possible to identify the fungal species: Scedosporium apiospermum (Figure 2).
The patient was treated by instillation of local antifungals (fluconazole at a concentration of 2mg/ml administered every 5 minutes for the first hour then every hour for 48h, betadine 1% at a rate of 4 instillations per day) and antifungals per os (fluconazole 400 mg twice daily at Day 1 and half dose for 30 days). At one month, visual acuity in the right eye increased to 4/10 with a disappearance of all inflammatory signs and a scarring of the ulcer.
Discussion
Scedosporium apiospermum keratomycosis are rare. In one study of 654 cases of fungal keratitis, 5 cases of keratitis were due to Scedosporium apiospermum (0.8%) [3]. This is the first case described in Senegal. A notion of plant trauma is often found [1,4]. One case was described after LASIK [5]. The diagnosis is guided by elements of the history such as plant or telluric trauma, clinical elements such as necrotizing ulcer, and confirmed by a microbiological examination. The severity of this fungus is explained by the delay in diagnosis associated with rapid tissue invasion, frequent co-infections and resistance to common antifungals [6].
Fluconazole is a broad-spectrum, second-generation triazole antifungal indicated for the treatment of cryptococcus, candidas and dimorphic fungi. It has good bioavailability, few adverse effects and diffuse well in the cornea after oral administration. These masterful preparations have good local tolerance and good intraocular penetration. Fluconazole does not exist as an ophthalmic solution in pharmacies, and requires a special magistral preparation done by the ophthalmology team, and kept for 15 days at 4°. The adverse effects of eye drops are mainly superficial punctuated keratitis. It’s the least toxic of the azoles. It can also be used in sub-conjunctival injection (1ml at 2%) and intacameral injection (0.35 ml at 0.1%). The ocular instillation of fluconazole improves local corneal effectiveness and intraocular penetration [7]. Oral administration allows for better systemic concentration.
The patient received an attack dose of 800 mg on the first day and 400 mg daily for 15 days. Other triazoles such as voriconazole is also used in the treatment of fungi. It is indicated in particular in the treatment of invasive aspergillosis and serious fungal infections with Scedosporium apiospermum and Fusarium in case of resistance to other antifungals [6,8]. Its oral bioavailability is high and the oral treatment is started with the attack dose (400 mg, 2 times/day) on the first day, allowing to obtain plasma concentrations close to steady state. His intraocular diffusion is good. Klont [8] reports that after 12 days of maintenance-dose oral therapy (200 mg, 2 times/day), its concentration in aqueous humor was 53% of that in plasma and its. These disorders begin 30 minutes after taking, are transient and completely reversible. Thiel [9] found concentrations of voriconazole in aqueous humor between 2.93 and 3.40 mg/L after oral and ocular joint dosing at 1 drop per hour. Concentration in the glass was 38% of that in the plasma. The most common adverse effects are visual disturbances and liver enzyme elevations. Approximately 30% of patients have vision disorders with colour change, blurred vision and photophobia [8].
Plasma concentrations were 3.20 to 4.20 mg/l. Scedosporium keratitis frequently progress to corneal perforation and mycotic spread [10,11]. After one month of topical and per os treatment of fluconazole, at the above doses, our patient showed a clear improvement in functional but also physical symptomatology. The non-specific inflammatory syndrome had disappeared. Visual acuity at 1 month was 4/10th in the right eye with a central nepheline.
Conclusion
Corneal scratching must be systematic in front of any corneal abscess. Scedosporium apiospermum keratosis are very rare. The oral and topical fluconazole expands the antifungal therapeutic arsenal at our disposal.
References
- Legeais JM, Blanc V, Basset D (1994) Kératomycoses sévè Diagnostic et traitement. J Fr Ophtalmol 10(5): 68-73.
- Wu Z, Yinf H, Yiu S, Irvine J (2003) fungal keratitis caused by scedosporium apiospermum succeefuly treated with a cornea transplant and voriconazole. J Clin Microniol 41: 2261-2264.
- Xie L, Zhong W, Shi w, Sun S (2006) Spect rum of fungal keratitis in north China 113: 1943-1948.
- Hermandez Prats C, Limores Tello F, Burgos San Joe A (2004) Voriconazole in fungal keratitis caused by scedosporium. Ann Pharma cother 38(3): 41-47.
- Sridhor MS, Gorg P, Basal AK, S Sharma (2000) Fungal keratitis after LASER in situ keratomilensis. J cataract Refract surg 26(4): 613-615.
- Ponchel C, Cassaing S, Linas MD, JL Arné, P Fournié (2007) Keratite fongique à scedosporium apiospermum. J Fr Ophtalmol 30(9): 933-937.
- Bourcier T, Sauer A, Letscher-Bru, E Candolfi (2011) keratites fongiques. J Fr Ophtalmol 34(8): 563-567.
- Pisella PJ, Baudouin C, Hoang-xuan T (2015) Surface oculaire. Rapport de la sfo elsevier Masson, Paris, pp. 677.
- Michael A Thiel, Annelies S Zinkernage, Jürgen Burhenne, Claude Kaufmann, Walter E Haefeli (2007) Voriconazole concentrationin human aqueous humor and plasma during tropical or combined and systemic administration for funga keratitis. Antimicrob Agents chemother 51(1): 239-244.
- Leck A, Matheson M, Tuf S, Waheed K (2003) Scedosporium apiospermum keratomycosis with secondary endophtalmitis Eye 17(7): 841-843.
- Wu Z, Ying H, Yiu S, Irvine J, Smith R (2002) Fungal keratitis caused by scedosporium apiospermum. Report of two cases and review of treatment. Coornea 21(5): 519-523.






























