Privileged Immunity for The Human Eye
PD Gupta*
Founder Director, Former Director Grade Scientist, Centre for Cellular and Molecular Biology, India
Submission: September 27, 2021;Published: March 02, 2023
*Corresponding author: PD Gupta, Former Director Grade Scientist, Centre for Cellular and Molecular Biology, India
PD Gupta. Privileged Immunity for The Human Eye. JOJ Ophthalmol. 2023; 9(5): 555771. DOI: 10.19080/JOJO.2023.09.555771
Abstract
The visual system in humans is unique and privileged in many ways. The reflected light from the object passes through the transparent cornea and lens gets converted into electrical signals by the retina, which is richly supplied with blood, passing through the optic nerve to the brain where these signals are processed and form the image. Because the eye must maintain transparency, there are ocular blood barriers present at different levels. And since there is no supply of the blood, the immune system must be unique. Another feature for the eye to see the objects, it remains always in touch to environment it requires extra protection to infections therefore the eye is provided a unique immune system designated as “immune privilege (IP)”-- the term coined by Sir Peter Medawar, in the 1948.
Keywords: Retina; Blood Barriers; Immune Privilege; Human Eye; Microbes
Abbreviations: IP: Immune Privilege; BAB: Blood-Aqueous Barrier; BRB: Blood-Retinal Barrier; SLC: Solute Carrier
Introduction
A pair of the eyes are unique sense organs placed on the face of human beings. The human eye is an important sense organ that reacts to light all the time. It is made up of three parts,
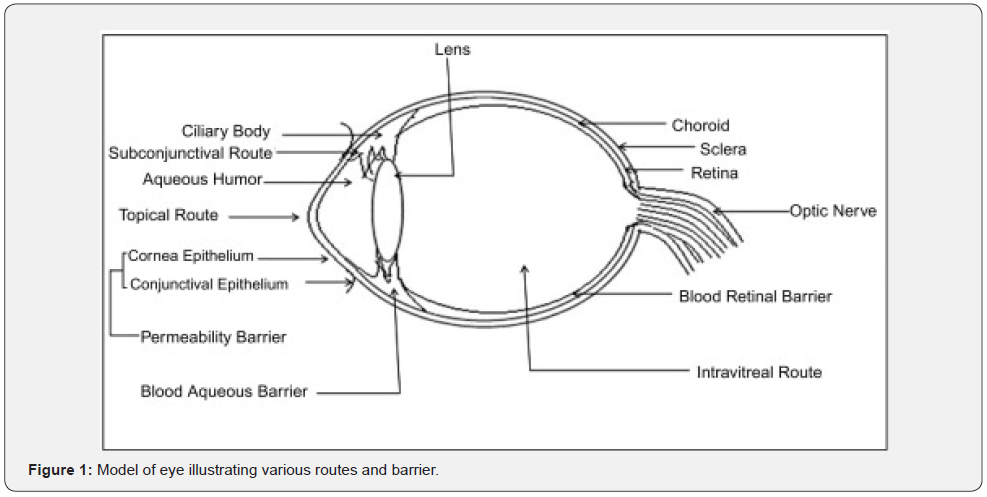
i. The outermost part consists of the cornea and the sclera, the optically clear aqueous humor, lens, and vitreous body.
ii. The middle portion contains the main blood supply to the eye and consists, from the back forward, of the choroid, the ciliary body, and the iris.
iii. The last one consists of rod and cone cells in the retina and optic nerve allowing conscious light perception and vision, including color differentiation and the perception of depth. The human eye can distinguish about 10 million colors. This part is also richly supplied with the blood [1,2].
iv. The eyes are also unique in a way to keep the anterior portion transparent; they have ocular- blood barrier system at various levels. Since there is no blood supplied in the anterior portion of the eye it is also provided a n unique immune system designated as “immune privilege (IP)”- the term coined by Sir Peter Medawar, in the 1948 [3].
Two immune systems
There are two main parts of the immune system in the human body:
a. The innate immune system, which we are born with.
b. The adaptive immune system, which we develop when our body is exposed to microbes or chemicals released by microbes. (For the details of the origin of immune system refer Gupta and Tyagi [4])
Ocular Immune System
The ocular immune system protects the eye from infection and regulates healing processes following injuries. The interior of the eye lacks lymph vessels but is highly vascularized, and many immune cells reside in the uvea, including mostly macrophages, dendritic cells, and mast cells [3]. These cells fight off intraocular infections, and intraocular inflammation can manifest as uveitis (including iritis) or retinitis. The eye attempts to limit local immune and inflammatory responses to preserve vision. The eye has a special relationship with the immune system, known as “immune privilege (IP)”. The term was coined by Sir Peter Medawar, in the 1940s for the first time noticed that foreign tissue grafts placed in the anterior chamber (see above) of the eye were not rejected since it lacks vasculature and relative immune separation from the rest of the body, so it lacks immune rejection [3]. The ocular (IP) is mediated by a combination of local and systemic mechanisms. While immune privilege is believed to protect the eye from day-to-day inflammatory insults, it is not absolute, and its mechanisms are still incompletely understood [5].
The cornea of the eye is immunologically a very special tissue. Its constant exposure to the exterior world means that it is vulnerable to a wide range of microorganisms while its moist mucosal surface makes the cornea particularly susceptible to attack. At the same time, its lack of vasculature and relative immune separation from the rest of the body makes immune defense difficult. Lastly, the cornea is a multifunctional tissue. It provides a large part of the eye’s refractive power, meaning it must maintain remarkable transparency, but must also serve as a barrier to keep pathogens from reaching the rest of the eye, like function of the dermis and epidermis in keeping underlying tissues protected. Immune reactions within the cornea come from surrounding vascularized tissues as well as innate immune responsive cells that reside within the cornea. The relationship between the immune system and the eye is much more complex. The eye is the prototypic immune-privileged organ. On the one hand, immune privilege is now known to involve not only sequestration but also active mechanisms that
i. inhibit innate and adaptive immune processes within the eye and
ii. shape the response that develops systemically to antigens released from the eye. On the other hand, retinal antigens are found in the thymus and have been shown to shape the eye-specific T- cell repertoire. However, thymic elimination of self-reactive T cells is incomplete, and such ‘escapee’ T cells are tolerized in the periphery as they recirculate through the body by encounter with self-antigen in healthy tissues [6] Figure 1.
Blood ocular barrier
The blood–ocular barrier is a barrier created by endothelium of capillaries of the retina and iris, ciliary epithelium, and retinal pigment epithelium [7]. It is a physical barrier between the local blood vessels and most parts of the eye itself and stops many substances including drugs from traveling across it. The tight capillary endothelium of the iris and the ciliary body epithelium form the blood-aqueous humor barrier. The iris and ciliary body express a variety of drug transporters in the ATP-binding cassette and solute carrier (SLC) families [8]. The blood-retinal barrier is located at two levels, forming an outer barrier in the retinal pigment epithelium and an inner barrier in the endothelial membrane of the retinal vessels. Both these membranes have tight junctions of the “nonleaky” type. The blood-aqueous barrier (BAB) is the anterior barrier of the eye that is composed of endothelial cells of blood vessels in the iris and the non- pigmented cell layer of the ciliary epithelium [9]. The blood–retinal barrier (BRB) is composed of retinal capillary endothelial cells (inner BRB) and retinal pigment epithelial cells (outer BRB). The inner and outer BRB [10]. are equipped with a variety of transporters and receptors and regulate nutrient flux between the circulating blood and the retina.
References
- Gupta PD (2014) Biochemistry of Vision. e book, National Institute of Science Communication, and Information Resources (NISCAIR). New Delhi, India.
- Nagpal K, Vasavada AR, Gupta PD (2005) Salient features of ocular biochemical status. In: Concepts of Biochemistry for Medical students Ed Prof LM Shrivastva. CBS Publishers pp. 479-514.
- Medawar PB (1948) Immunity to homologous grafted skin; the fate of skin homografts transplanted to the brain, to subcutaneous tissue, and to the anterior chamber of the eye. Br J Exp Pathol 29: 58-69.
- Gupta PD, Tyagi S (2020) Development of Immune System from Newborn to Adult: A New Insight. J Cell Tissue Res 20(1): 6853-6860.
- Zhou R, Caspi RR (2010) Ocular immune privilege. F1000 Biol Rep 2: 3.
- Caspi RR (2006) Ocular autoimmunity: the price of privilege? Immunol Rev 213: 23-35.
- Cunha-Vaz J (1979) The blood-ocular barriers. Surv Ophthalmol 23(5): 279-296.
- Wu W, Dnyanmote AV, Nigam SK (2011) Remote communication through solute carriers and ATP binding cassette drug transporter pathways: an update on the remote sensing and signaling hypothesis. Mol Pharmacol 79(5): 795-805.
- Hornof M, Toropainen E, Urtti A (2005) Cell culture models of the ocular barriers. Eur J Pharm Biopharm 60(2):207-225
- Campbell M, Humphries P (2012) The blood-retina barrier: tight junctions and barrier modulation. Adv Exp Med Biol 763: 70-84.






























