Role Of Nutrition on Myopia Progression
Amani Omari Masenya*
School of Advanced Education, Research and Accreditation (SAERA), Spain
Submission: February 01, 2023;Published: February 28, 2023
*Corresponding author: Amani Omari Masenya, School of Advanced Education, Research and Accreditation (SAERA), Spain
A Thesis Submitted to the Department of Optometry, School of Advanced Education, Research and Accreditation, In Partial Fulfillment of the Requirements for a Master’s Degree 2022 Supervised by Raúl Pérez
Amani Omari Masenya. Role Of Nutrition on Myopia Progression. JOJ Ophthalmol. 2023; 9(4): 555770. DOI: 10.19080/JOJO.2023.09.555770
Abstract
This is a descriptive research based on a systematic review of previously published articles in order to examine the relationship between nutrition and the progression of myopia in children. The literature encompasses the published articles from 2015 to 2022 examined the exclusive role of various nutritional factors influencing myopia progression. The deficiencies and supplement administration are also taken into consideration while selecting the influencing variables during the progression of the disease. These include primarily Vitamin A, and D, Zinc deficiencies, administration of dietary supplements, and healthcare behavioral change studies in particular. The extensive literature review agrees with the findings of most of the research and clinical studies done previously as there are no significant, proven connection between nutrition and myopia progression.
Keywords: Myopia, Diet, Nutrition, Myopia Progression, Vitamin A, Vitamin D, Diet supplements, Refractive Errors, Deficiencies
Abbreviations: BMI: Body Mass Index; NHANTS: National Health and Nutrition Test Survey; WHO: World Health Organization; GEHP: Global Eye Health Plan; 7-MX: 7-methylxanthine; FFQ: Food Frequency Questionnaire
Introduction
Myopia is a very common refractive error, corrected by glasses and contact lenses. The first glasses were made by some monks in Italy in the 13th century, from hand-carved glass. At the end of the 19th century, Fick and Kalt carried out the first tests on contact lenses [1]. Today there is also refractive eye surgery, a surgical technique capable of definitively eliminating the defect of myopia. The name of myopia is due to the habit of myopic individuals squinting their eyelids when looking at distant objects. In this way, myopia is a form of refractive error in which parallel light rays arrive at a focus in front of the retina, that is, the image focus is located in front of the retina and not directly on it when the eye is at rest; the eye, then, is relatively too long. Due to this visual problem, nearby objects are seen clearly, but distant ones are blurred [1]. This paper addresses the impact of nutrition on the prevention of myopia progression. The concept has shown, while proper nutrition has been shown to play a role in slowing the progression of myopia, inadequate nutrition can exacerbate the condition, worsening it over time.
Etiology
Following is the basic classification of myopia [2]:
• Axial myopia. It is due to an increase in the antero-posterior diameter of the eye. It is usually of congenital type.
• Curvature myopia. It may be accompanied by an increase in the curvature of the cornea or one or both sides of the lens. It is related to late-acquired myopia.
• Index myopia. Caused by an alteration of the refractive index of the aqueous or vitreous humor. It is usually senile acquired myopia.
In the vast majority of cases, and mainly in the most intense forms, myopia is of the axial type. Clinically, myopia is classified into benign or simple myopia and pathological or degenerative myopia. Simple myopia is a state of limited progression, in which the refractive defect does not exceed 6 diopters (D) and does not cause problems in the fundus of the eye (retina). On the other hand, in pathological myopia, the process is clearly of a more serious nature since there is an alteration of the fundus. In this case, the refractive error exceeds 6 diopters, and the pathology can rapidly increase to a degree where it warrants consideration as an individual clinical entity [3]. The etiology of pathological myopia is not entirely clear. The weakness of the sclera and its consequent inability to withstand intraocular pressure without collapsing and expanding was generally considered. It was accepted that the fundus abnormalities were due to this but it seems more likely that they are generally due to a developmental genetic defect affecting the entire posterior segment of the eye.
Whatever the cause, it is likely that the primary defect of myopia is a developmental disorder. This seems to be indicated by the fact that the process, although rarely congenital, can present early and is typically hereditary. It can be said that myopia only develops during the period of active growth of the individual, since the elongation of an eye that has remained up to 25 years with normal dimensions is very rare. The eye shares with the brain the peculiarity of having earlier growth than the rest of the organism, and around 20 years of age the eye and the brain have already reached their adult dimensions [4]. It has been suggested that myopia is the result of a continuation of this precocity, due to the absence of a braking influence.
According to Han et al., [5], in the past, it was considered that the key to the problem laid in the sclera. Today, it is believed to be due to the retina, since the retina develops considerably in postnatal life, almost doubling its area, and it is quite understandable that the length of the axial axis of the eye accommodates this tissue. For this reason, when the retina grows more quickly and extensively than normal, the sclera becomes distended, and myopia appears. However, there are also factors that have some influence on its progression. Such would be the case for the importance of close work in etiology. Taken together, it would seem true that the influence of close visual work is secondary in the etiology of a process that is essentially predetermined and constitutional, and not environmental. The latter will only have an impact when it is associated with poor eye hygiene and a lack of adequate facilities for normal and healthy visual development.
Myopia Progression
It is very rare that there are cases of newborn myopia, although in some cases the myopia is congenital, and in some of these cases the process remains static. The usual process in childhood is an alteration of refraction in the form of hyperopia that will decrease with the passage of time, and in some cases, it will end in simple myopia. This alteration will not cause vision error symptoms until adolescence, although it can occur early in some people. From this moment on, these cases will generally progress in the following years to 5 or 6 diopters, finally stabilizing around the age of 21, or somewhat earlier in women [6]. It is very rare, but not impossible, for myopia to start after adolescence.
In this case, great care must be taken to eliminate other causes of the myopic process, such as early diabetes, and, of course, the presentation of a myopic state at this stage of life may in no way indicate its origin at this time: it may have started earlier and to have gone unnoticed until then. If the error progresses rapidly in early youth, it is less likely to stabilize, and may reach 20, 25, or even 30 diopters; in these cases, the fastest period of progression is generally between 15 and 20 years old. Subsequently, the process is usually delayed, but in cases of great intensity, degenerative alterations generally appear in later decades, so vision can deteriorate in a very pronounced way until around the age of 60 blindness appears [3]. To lesser degrees, the tendency to hyperopia typical of lens disorders that occur in advanced age (presbyopia or eyestrain) decreases myopia.
Myopia Complications
Retinal detachment can occur due to high myopia of 15-18 diopters or due to trauma (accidents or sports). It may happen that due to detachments, tears, or hemorrhages of the vitreous humor, the retina is also dragged. In addition, degenerative changes in the vitreous may also cause some loss of vision (e.g., degenerated and liquefied vitreous results in floaters and floating opacities, and because these project abnormally large images onto the retina, they produce large images in the patient, resulting in discomfort and anxiety). Degenerative processes of the lens can lead to the formation of opacities (cataracts) [7]. It can be complicated by cases of glaucoma, such as high-grade myopic simple glaucoma.
Problem Statement
There has been a lot of study into the potential risk factors for myopia development and progression, and they include both close work and, more recently, less time spent outside. Myopia is certainly caused by more than one item, although there is not much consensus on the components that play a part in its development. For example, in the first epidemiological investigation, nearsightedness was shown to be associated with the implementation of standardized school education. Despite this, dietary patterns saw significant shifts throughout this period as the influence of the West grew.
In general, there are not many studies that look at the link between nutrition and nearsightedness. Werbach, [7] who described high-glycemic-load meals as a risk factor for myopia in an early observational analysis, hypothesized hyperinsulinemia as a possible underlying mechanism, as it can be seen in Table 1. Myopia is a condition in which the eye becomes more nearsighted. On the other hand, the results of a cross-sectional study that was conducted on Singaporean children (aged 7-9 years) showed that children who were shorter in height but had a higher body mass index (BMI) had fewer instances of myopic refractions. This was assuming that BMI reflects glycemic load. Caffeine and one of its metabolites, 7-methylxanthine, have been shown to have protective effects against the development of myopia, with choroidal and scleral targets as possible sites of action [8]. However, evidence linking insulin with increased eye growth has been found in animal models of myopia.
Objective
Myopia’s fast ascent in incidence is a major global public health problem that cannot be attributed to heredity alone, but rather to a combination of genetic and environmental variables.
The potential impact of diet on myopia has received little research attention. Since the huge National Health and Nutrition Test Survey (NHANTS) dataset contains vision examination results, researchers may look at the link between myopia and various nutrition-related parameters, such as body metrics.
Research Question and Hypothesis
RQ: What is the role of nutrition in preventing Myopia progression in children?
The research question has been formulated in a clear and precise manner because it determines the rest of the review. For this, they have drawn inspiration from other reviews, and the recommendations of the PICOT method (Participants, Interventions, Comparisons, Outcomes, Time). The question has been targeted (e.g., how can nutrition help in preventing the progression of myopia). The choice of the research question depends on the relevance of the review. There are many methods that can be used to answer research questions and take variability into account. With a well-planned study, researchers may find solutions to their problems and lay the groundwork for future investigations.
H1: There is a direct correlation between diet and body development and the development and severity of myopia in children.
H2: Environmental factors play a vital role in myopia progression and specific interventions can reduce the progression of myopia in children.
Literature Review
There is a lot of debate over the significance of continuous exposure to highlight levels outdoors, but it is significant to keep in mind that the amount of time spent in the sun has a significant positive link with the amount of vitamin D in the blood.
Data Selection
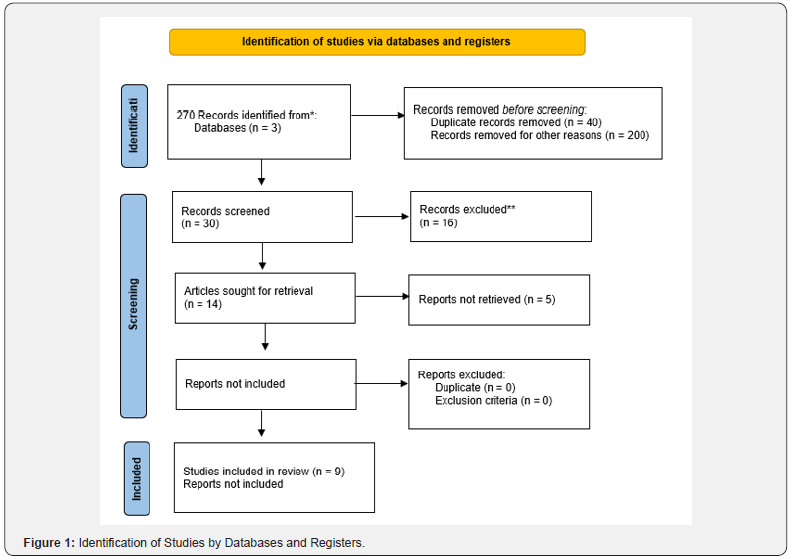
All studies that were chosen were retrospective case-control or cohort studies. Because of the lack of control groups, we did not evaluate case series, reviews, case reports, thoughts, letters, opinions, or editorials. The synopses were not included since they were not peer-reviewed and were published as complete papers. Each study was assessed for both internal validity (how well the cases and controls were matched) and external validity (how well the results could be applied to other contexts). In total, 270 articles have been selected for review and out of which 30 articles met the inclusion criteria for literature review. They are both general and specific. But for meta- analysis only 9 articles were left that met all the inclusion and exclusion criteria, as it can be seen in Figure 1.
Factors Contributing to Myopia and Its Manifestations
The World Health Organization (WHO) estimates that 285 million individuals worldwide have some sort of vision impairment, with an additional 39 million being completely blind. There were 1012 million individuals in the world with some degree of vision impairment due to uncorrected refractive errors in 2010, and 6.8 million people with blindness (visual acuity poorer than 3/60) due to the same condition [9]. To address this issue, the World Health Organization (WHO) devised the Global Eye Health Plan (GEHP) for 2014-2019 to deal with this public health problem, with one of its main goals being to increase people’s access to eye-care services to decrease the number of people who suffer from preventable blindness. Whether or not an individual wears corrective lenses, the vast majority of eyes have some degree of refractive error. The purpose of this article is to provide a synopsis of the known hereditary and environmental factors that contribute to the onset of refractive errors, with a focus on myopia.
Refractive errors result from an incongruity between the axial length and optical power of the eye, leading to blurred retinal images. While some infants are born with significant refractive errors, these often improve as their eyes grow and their cornea and intraocular crystalline lens adapt to their new focal lengths [6]. This passive emmetropization procedure works with an active, visually-emmetropisation process to rectify any remaining refractive defects [10], as it is seen in Table 1. A failure of the later emmetropization process is shown by the existence of refractive defects in children. Myopia, often known as nearsightedness, is the particular refractive defect that will be investigated in this dissertation. Myopia develops when an eye’s axial length is excessive relative to its optical power. Because their eyes are considerably stronger than average, faraway objects concentrate in front of the retina, causing maximum blur at long ranges and reduced blur at close ranges. Sometimes myopia, known as syndromic myopia, develops in utero as part of a systemic congenital disease affecting several organs and systems.
Most cases of myopia, however, do not fit into this group and are instead classified according to when they first appeared: congenital (existing at birth, frequently at high levels, and notably in preterm newborns), preschool, preteen-onset or school, and adult. Myopia, both juvenile and adult-onset, is often axial in character and results from a poorly controlled development mechanism(s). Due to the delayed onset of symptoms and the fact that uncorrected myopes often have the normal near vision, uncorrected myopia does not provide the same significant amblyogenic risk as uncorrected hyperopia. Although the risk of visual impairment is greatest in the case of extreme myopia, even mild to moderate myopia poses a substantial danger, since it is connected to retinal detachments, myopic maculopathy, glaucoma, and cataracts.
This article will try to summarize the known genetic and environmental variables that lead to the development of refractive anomalies, with an emphasis on myopia. When the eye’s axial length and optical power are mismatched, refractive errors occur. As a consequence, the images that develop on the retina are distorted. Even though many children are born with significant refractive abnormalities, they often correct themselves as the child develops because the cornea and intraocular crystalline lens can adapt to their changing shape and size [11] as it is seen in Table 1. When used in tandem with an active, visually mediated emmetropization procedure, this passive emmetropization technique may help rectify any remaining refractive errors. Unfortunately, this doesn’t describe the vast majority of myopic instances, which are instead classified according to when the problem originally appeared.
Premature babies are more likely than full-term babies to be born with congenital myopia. The most prevalent kind of myopia is that which develops in children or young adults, often known as juvenile myopia or school-related myopia. Myopia is not limited to childhood, and may develop at any age, but its cause is the same whether it begins in infancy or later in life. A developmental process that was not carefully monitored/ untreated myopia, on the other hand, does not provide as big of a danger of developing amblyopia since its symptoms do not manifest until later in life and uncorrected myopes often have normal near vision. However, untreated hyperopia does pose a significant risk of developing amblyogenic conditions. Even moderate myopia is risky because of its link with retinal detachments, myopic maculopathy, glaucoma, and cataracts. The risk of visual impairment is greatest for those with extreme myopia, but even moderate myopia poses a risk.
Wu et al., [12] have pointed to the possible relevance of close work and, more recently, of reduced time spent outdoors as risk factors in the beginning and progression of myopia. There is not a lot of agreement on the factors that play a role in the development of myopia, although it is likely that myopia is caused by more than one thing. For example, in the first epidemiological investigation, nearsightedness was shown to be associated with the implementation of standardized school education. Despite this, dietary patterns saw significant shifts throughout this period as the influence of the West grew.
Nutritional Deficiencies
Chiang et al., [13] attribute the rise in the number of myopes to the shift from an agricultural and illiterate society to an industrial and literate one, citing differences in food as the cause of the increase in myopia. Myopia advancement, however, is not entirely impacted by a single cause, such as diet. More likely to affect increases in the incidence of myopia than changes in diet are the many societal changes that occurred as our society got more industrialized, such as the mainstreaming of the ability to read and write. Some research suggests that eating more like a “hunter-gatherer” may slow the advancement of myopia because of the role that newer high-glycemic-load carbohydrates have in the development of insulin resistance. Myopic children consumed less numerous nutrients than their non-myopic peers. Energy, fat, protein, vitamins B, B2, and C, iron, phosphorus, and cholesterol consumption all varied significantly but can affect the development of the body [14].
The Connection between Poor Diet and Myopia
There has been little study on the link between poor diet and myopia. High-glycemic-load meals were noted as a risk factor for myopia, in an early observation in research by Werbach et al. [7] and they postulated that hyperinsulinemia was the underlying cause. Increasing nearsightedness of the eye is called myopia. However, myopic refractions were less frequent among kids who were shorter in height but had a higher body mass index (BMI) according to a cross-sectional study of Singaporean kids (aged 7-9 years). This is based on the hypothesis that body mass index reflects blood glucose levels. It is known that caffeine and one of its metabolites, 7-methylxanthine, may act on the choroids and sclera, respectively, to prevent the advancement of myopia. Animal models of myopia, however, have shown a correlation between insulin and accelerated eye development.
According to Edwards [4], four randomized controlled studies conducted on Asian children found that increasing the amount of time spent playing outside during recess reduced the chance of developing myopia. Wang et al., [15] discovered in a randomized controlled study that exposure to outdoor natural light might lessen myopia brought on by defocusing. Rhesus monkeys’ early exposure to sunshine may also encourage normal growth in maturity, lowering the likelihood that they would acquire myopic refractive defects. According to Ashby et al.’s [16], findings, chicks exposed to both natural and artificial light (15,000 lux) were less likely to acquire myopia than those subjected to standard experimental lighting settings (500 lux). In an 18-month longitudinal research, Read et al. [17] discovered that kids with higher average daily light exposure had slower axial eye development.
According to the study done in Taiwan by Wu et al. [12] it was discovered the group of students who had outdoor excursive had a lower new incidence rate of myopia (8.41%) than students in the control group (17.65%). Myopia can be prevented and controlled with the help of outdoor activity treatments for kids who are not myopic. While the importance of prolonged exposure to bright outdoor light is hotly debated, it is clear that time spent in the sun significantly correlates with vitamin D levels in the body. Two substantial cohort studies that examined the relationship between blood vitamin D levels and refractive error discovered inconsistent results regarding the significance of low serum vitamin D levels as a risk factor for the emergence of myopia. For example, one study revealed that those who spent more time outside had higher levels of vitamin D in their blood than those who spent less time outdoors (p=.03).
Consistent with the results of a previous genome-wide association study (GWAS), this conclusion is reliable. Only three other previous research that Han et al. [5], really used the NHANES database to investigate the impact of the environment on the onset of myopia, including Ashby et al., [16], Read et al., [17] and Wu et al., [12]. Two of these studies [16,17], focused entirely on body measurements, whereas the third Wu et al., [12] also included dietary factors. The study indicated that myopia was more common among women than men at every age. Myopia and myopic refractive errors are more common in women and become more common as people age. Although there was a clear disparity in mean SERs across ethnic groups in univariate analysis, the multivariate analysis failed to find a correlation between race and myopia prevalence or severity. It was revealed that individuals with elevated insulin levels had a substantially higher likelihood of being myopic, but no other dietary variables were found to be significantly related to the incidence of myopia in this participant cohort.
Height may have a role in the development of nearsightedness and farsightedness since other worldwide population-based research has shown links between longer eye length and/or myopia among taller people. The results of this research agree with those of these previous international surveys of whole populations. The vast majority of these investigations have included individuals over the age of 40, whose refractive errors are more likely to remain consistent throughout the course of their lives. Nonetheless, two Asian studies conducted with children aged 7-9 have shown exceptions to this rule.
According to research that was conducted on Taiwanese children 48 and a population-based study that was conducted on Chinese adults, height is positively related to longer eyes but is not associated with myopia. This apparent disparity is most likely explained by the fact that persons who are taller have anterior chambers that are deeper, lenses that are thinner, and corneas that are flatter. The results of Edwards [4] who hypothesized a relationship between hyperinsulinemia and the development of myopia were found to be coherent with those of his investigation. This was one of the things that Edwards [4] discovered, as well as a study conducted by Berticat, et al., [18], which has shown a connection between diabetes and myopia (nearsightedness).
The findings of a second, more limited study by Edwards [4], by some of the same researchers, on the other hand, lend credence to the hypothesis that lenticular alterations are responsible for the increased prevalence of myopia in diabetics, as it can be seen in Table 1. The glycemic profiles of individuals all over the world might be to blame for the observed increases in myopia prevalence rates, according to a new analysis of relevant epidemiological research. A discussion on the possible paths via which insulin could boost ocular development came before this.
However, evidence supporting the latter comes from research that was carried out on animal models, and it is not conclusive.
For instance, although it was discovered that insulin promoted the development of myopia in a few studies involving chicks, such as Ashby et al., [16], the pattern of axial elongation was atypical in the sense that anterior segment changes contributed the most to the overall increases in eye length. This was because the pattern of axial elongation was atypical.
Since increasing the amount of time spent outside is known to be advantageous against myopia, there has been some speculation over whether vitamin D alone would be protective against the condition and is also directly connected to the amount of vitamin D found in the blood [19]. Several hypotheses have been proposed to explain how low blood levels of vitamin D can increase the risk of myopia [20], as it is shown in Table 1. These hypotheses include an increase in scleral extracellular remodeling as well as a synergistic interaction with retinoic acid, which is well-known for its role as an ocular growth regulator. However, four significant cohort studies, including one analysis of the NHANES cohort, were unable to reveal a relationship between low levels of vitamin D and myopia, which is consistent with the results of the current research. The current study revealed that African Americans had the lowest proportion of myopes (35%, 1% lower than the average), which matched the findings of earlier research [3], demonstrating that African Americans had the lowest blood levels of vitamin D. However, the new study also indicated that African Americans had the lowest number of myopes.
A number of new animal model studies have provided evidence for the therapeutic potential of caffeine and its metabolite 7-methylxanthine (7-MX), which is a non-selective adenosine receptor antagonist, as it can be seen in Table 1. These investigations have been conducted recently. Vitale et al., [3] results are consistent with those of earlier Danish pediatric clinical research utilizing oral 7-MX. That investigation revealed a relative reduction in axial elongation and the development of myopia, and these findings support that conclusion. The longterm clinical investigations that Danish researchers have been doing on 7-MX tablets as a therapy for myopia are still ongoing [10].
The investigations that were reported here were, regrettably, limited to using caffeine intake data from the NHANES survey since data on caffeine metabolites in urine are only available beginning in 2009, which is when assessments of refractive error were stopped. To the best of my knowledge, there have only been two further thorough investigations based on the NHANES dataset. Both of these researchers focused on the association between myopia and other dietary characteristics. In a study of adolescents and young adults that was part of the National Health and Nutrition Examination Survey, there was no correlation found between myopia and total zinc intake [21], as it can be seen in Table 1.
Because axial length data were inaccessible, the availability of objective refractive error data is an additional strength of the current research. This strength is bolstered by the large and ethnically diverse NHANES participant cohort as well as the analyses that are utilized within it. The dependability of the data was increased by the fact that all NHANES sites followed the same processes for obtaining measurements using predetermined protocols. Competent specialists carried out these procedures. The research does have several drawbacks, the most notable of which concerns the ethnic groups that were utilized during the study years that were analyzed.
However, it is crucial to bear in mind that the research does have several problems. Considering the substantial prevalence of nearsightedness among Asian people, both in Asia and in the United States, the lack of a category labeled “Asian” is a fundamental weakness that has to be addressed. It is probable that the inclusion of individuals of Asian ethnicity in the Other/ Mixed ethnicity category explains why this group had the highest number of myopes [3], as well as why they were much more myopic overall. As a result of the high prevalence of myopia in the population that served as the basis for Vitale et al., [3] research, the collection of data on refractive errors was limited to children older than 12 years of age. This represents a time point that is later than the average age at which myopia first presents itself in children. This may help to explain why Berticat et al., [18] found age to be only marginally significant in our multivariate modeling, even though it has been proven to affect the refractive error in numerous previous studies. In addition to this, it’s probable that the dietary records that are maintained on adolescents will be different from the ones that are kept on younger children.
The study’s potential generalizability is reduced, however, because of its cross-sectional design. It was discovered by Ng et al. [22] those borderline significant relationships existed between daily crocetin administrations and reduced myopic development and AL elongation, as it is shown in Table 1. Myopia prevalence has been shown to be poorly correlated with secular variations in height or weight, although healthier diets tend to lead to larger populations.
The results of this research disprove the hypothesis that a healthy diet may help avoid myopia [18], as it can be seen in Table 1. That being said, Han et al., [5] can’t endorse particular diet forwarding against myopia. Increasing education and reduced time outdoors are both strongly associated with increased chances of myopia in youngsters. Preschools and other early learning programs, as well as extended after-school tutoring, are more common in countries with a high myopia burden. It has been shown via outdoor experiments that spending an extra 40- 80 minutes outside each day may lower myopia incidence by as much as 9 percent - an absolute reduction [5].
Myopia is more common in those who have a family history of the condition or who themselves are nearsighted [5], as it is seen in Table 1. Several genes, including those that regulate circadian rhythms and light-induced signaling, have been linked to the development of refractive errors in meta-analyses of genomewide association studies. On the other hand, the research conducted by Ng et al., [22] did not identify any link between myopia and dietary variables, and the data so far suggests that dietary factors have little role in the pathophysiology of myopia. It follows that near work and less time spent outside are the most probable two environmental risk factors for myopia. They investigated myopia with cycloplegia and the dietary habits of Asian children across time using an age-appropriate, validated Asian Food Frequency Questionnaire (FFQ) to measure the consumption of a wide variety of nutrients and food categories. Additionally, they understood that alone evaluation of typical consumption over the preceding month was insufficient to identify dietary alterations. Therefore, they suggest bigger prospective trials that evaluate food over long periods of time and with more participants.
Methodology
The technique for this study was a systematic review. A systematic review is a difficult endeavor that adheres to the same guidelines as any other research project. Therefore, creating a protocol is the first stage in the process. This allows for the systematic review to have the highest level of impartiality while limiting prejudice. The writer can rely on the Cochrane collaboration’s suggestions for its writing. To guarantee the study’s transparency, it is strongly advised that the systematic review methodology be registered in advance [23]. This enables readers to highlight registered but unpublished protocols or identify potential reporting bias (differences between the original protocol and the published review).
As per the guidance in the study by Elliot et al., [23] to assess the potential for bias in the research’s methodology, the full text was independently. Because of the limited sample sizes in this research, broad conclusions should be drawn with caution. The selection process could have been skewed because only papers in English were considered. The inclusion criteria were so stringent that few studies met them, since they required the viewpoints and experiences of student midwives, a population underrepresented in the literature. If the sample had been more representative of the population, perhaps other conclusions would have been drawn. Considering the limited number of mentioned studies, the results should be interpreted with caution. The primary goal of such a study is to provide an accurate depiction of the state of affairs inside the study’s setting. When a study population is too big to observe in person, researchers turn to survey research methodologies. Recent research suggests that descriptive research is the way to go if they want to draw firm conclusions from the data [23].
Search Strategy
The Google Scholar platform was used to conduct literature searches in the ERIC and NCBI databases from January 1, 2000, to December 30, 2022. ERIC is publicly accessible at https:// www.ebsco.com/products/research-databases/eric and NCBI is publicly accessible at https://pubmed.ncbi.nlm.nih.gov/. The search approach was based on Boolean logic. The names “myopia” and “nutrition” were used both as free words and as MeSH terms. Supplementary Table 1 provides thorough search tactics. It was manually checked to see if there were any more articles in the reference lists of the eligible papers and reviews that the computerized search had missed.
The search strategy employed has allowed for an exhaustive search to collect the most considerable number of studies and reduce selection bias. There is no ideal strategy, and each question has led to an appropriate search. The search strategy has been based on a list of keywords and synonyms, which are listed in reference articles. These keywords, taken from a free text or controlled vocabulary, have appeared in the search according to precise logic. The PICOT method has helped identify an appropriate search strategy by guiding the use of keywords and Boolean operators (AND, OR, NOT). Finally, it is possible to use predefined search strategies to filter studies according to their type. The words for searching the relevant articles are “Myopia” and “Nutrition”. And only the articles that were in the range of 2000 to 2022 have been selected. The total search results were 270 articles, from which the most relevant articles have been selected to meet the inclusion criteria. For the metaanalysis, only 9 articles have been selected out of 14 articles that were meeting the exclusion and inclusion criteria, as it can be seen in Figure 1.
The primary goal of such a study is to provide an accurate depiction of the state of affairs inside the study’s setting. When a study population is too big to observe in person, researchers turn to survey research methodologies. Recent research suggests that descriptive research is the way to go if they want to draw firm conclusions from the data [23].
Eligibility Criteria
Once the research question has been defined, it is necessary to specify the eligibility criteria for the studies. The specifications on which the authors base themselves to select the studies to include in the review are a combination of the types of studies, the participants, the types of interventions, and the endpoints. This step is again fundamental. For example, in this research, the researchers carry out a review of the interventions intended to improve myopia, it is necessary to define what is meant by myopia, the age groups considered (children), the care context (nutrition-based therapy), the endpoints to be analyzed in the studies, and the minimum duration of patient follow-up. A total of 270 articles that have the word “nutrition” and “myopia” have been selected. However, only 9 articles that were related to children have been included in this study, as it has shown in Figure 1. Animal studies, case studies, reviews, abstracts from conferences, editorials, non-English papers, and reports with insufficient data were all disregarded.
Data Extraction
Data extraction has been done after the final decision to include research in the evaluation. It was taken from the research by at least two different individuals. All the information required for the analysis of the research, such as the eligibility requirements, the methodologies, the participants, the treatments, the endpoints, or the findings, have been collected by using a data collecting form. To evaluate the strength of each study’s evidence, bias risks have also been taken into consideration.
Risk of Bias Assessment
To avoid bias, it is recommended to carry out a search of gray literature, that is, literature not controlled by a commercial publisher. These may include conference proceedings, government or industry publications, expert opinions, or various reports. This paper will also include gray literature with the use of other relevant literature from different databases.
Data Analysis
Although their level of evidence is lower than that of randomized trials, these studies are sometimes the only option for evaluating the effect of an intervention. Their inclusion or exclusion depends on the type of intervention being assessed and should be discussed between review authors, particularly nutrition for preventing myopia progression. All the eligibility criteria are used to guide the search strategy and refine the selection of studies. To ensure the exhaustiveness of the search, it is essential to search for the studies in several databases because no database contains them all. The main bibliographic databases for researching intervention studies are Google Scholar, ERIC, and NCBI, to which they have added regional or disciplinespecific databases. A total of 270 articles have been obtained. But specifically, only 30 articles met the inclusion criteria for literature review and meta-analysis. And only 9 articles met the exclusion and inclusion criteria for a meta-analysis. A literature review is a broad area that converges to this specific research. However, for a meta-analysis, specifically, 9 articles have been used that perfectly met inclusion and exclusion criteria, as it can be seen in Figure 1.
Results
After searching ERIC, Google Scholar, and NCBI, a total of 30 references were located out of 270 which were easily accessible in full-text format. Only 9 of the 30 records eligible for qualitative synthesis were usable for the quantitative metaanalysis (one study had all predictors analyzed as continuous numerical measures, so no data were usable from the article’s description; four other articles did not have data clearly available in the two intervention groups of this meta-analysis), as it can be seen in Figure 1. All the studies had the characteristic of being retrospective, but beyond that, there were numerous other parallels and variances.
This systematic review’s strength is its wide range of likely diet effects and many observational studies in general populations. The study is more likely to include a representative sample of the at-risk population and reflect actual adverse event kinds and rates. Observational studies are useful, but often biased and confounded. This meta-analysis may have been biased by a “healthy-user effect” or enhanced scrutiny. Despite the investigation of the robustness of the results across three dimensions, the pooled observational data may be heterogeneous due to different populations analyzed, or outcome criteria (study design, sample size, and quality of the studies). All systematic reviews that use public data cannot assess outcome definition homogeneity. A random selection of 10% of titles and numbers collected identified no conflicts, although having a single reviewer examine all data extraction and validity is a limitation. Publication bias affects observational meta-analyses most.
Even though they requested unpublished material, observational studies with significant outcomes are more likely to be published, and thus they may be overrepresented in the meta-analysis. This bias may exaggerate pooled effect sizes. Limited myopia and nutrition literature makes updating this study difficult. Keeping this in mind, they did a fast Medline update search and added major new findings to the discussion. In a recent meta-analysis of randomized controlled trials and observational studies, diet intake was not linked to myopia progression.
Research has identified two main risk factors. You can act on both when you are a parent of a child. The first factor: is the little time spent outdoors. For example, a recent study compared the vision of Chinese children living in Sydney and Singapore. Result: 3% of myopia among the Chinese in Sydney and 29% among those in Singapore. But in Australia, Chinese children spent about 13 hours a week outdoors, compared to 3 hours in Singapore. Another example: in Taiwan, teachers left children outside for 80 minutes a day rather than allowing them to stay inside during the break. After a year, doctors diagnosed myopia in 8% of these children, compared to 18% in a nearby school. When they spend too little time outdoors during childhood, the eye cannot retain its elasticity which comes from constantly accommodating between nearby objects and the horizon. When this horizon is usually a few tens of centimeters away, or it takes the form of a screen, the eyeball is no longer stressed enough, and myopia sets in (and presbyopia later).
Food makes up the second element of progressive myopia, as a result of the stimulation of the cell growth factor IGF-1 (insulin-like growth factor-1), a Western-style diet high in dairy products, sugars, and refined carbohydrates with a high glycemic index is becoming increasingly linked to the development of myopia. Actually, myopic children develop more quickly than other kids do. All foods that increase insulin production, such as sugary and refined foods and dairy products, encourage the growth of the eyeball, causing it to enlarge excessively. It should be encouraged to kids to spend time outside rather than watching a screen to prevent myopia, and make sure the family’s diet is of high quality, too. Therefore, it is encouraged to improve family nutrition by reading various books on the best options for kids and eating techniques.
Discussion
Meta-analysis is a useful technique for summarizing data from a range of studies and is therefore only valid if the data from each study are comparable. According to Kerlinger (1973), who stated that there are many methods that can be used to answer research questions and account for variability, he added that with the help of a well-planned study, researchers can find solutions to their problems and explain the basis for future investigations. Thus, according to the hypotheses of this study, it depends on the relevance of the assessments that have been identified, with the first hypothesis exploring a direct relationship between nutrition and physical growth and the occurrence and severity of myopia in children, while the second hypothesis examines what environmental factors are significant in the onset of myopia and what specific measures can be taken to slow its progression in children.
According to the findings which hypothesized by Morgan et al. [6], a link between hyperinsulinemia and the development of myopia, which were found to be consistent with those of their research, this was one thing they discovered. The results of a second, smaller study by Edwards [4], however, confirmed the hypothesis that lenticular changes are responsible for the increased prevalence of myopia in diabetics, indicating that the glycemic profiles of individuals worldwide may explain the observed increase in the prevalence of myopia rates, according to a new analysis of relevant epidemiological research. This was preceded by a discussion of possible pathways by which insulin could stimulate eye development. The evidence to support the latter, however, comes from research conducted in animal models and is inconclusive. For example, while insulin has been found to promote the development of myopia in some chick studies, as anterior segment modification accounted for most of the total eye length increase, the pattern of axial elongation was unusual.
Quoting Hsu et al. [20], who found vitamin D blood levels to be of interest in knowing whether vitamin D alone would be protective or not. Several hypotheses have been proposed to explain how low blood levels of vitamin D may increase the risk of myopia, as it has shown in Table 1. These hypotheses include an increase in scleral extracellular remodeling and a synergistic interaction with retinoic acid, known for its role as an ocular growth regulator. However, the NHANES cohort analysis failed to reveal an association between low vitamin D levels and myopia, which is consistent with the findings of the present study. The current study revealed that African Americans had the lowest proportion of myopes [24], which matched the findings of earlier research demonstrating that African Americans had the lowest blood levels of vitamin D. However, the new study also indicated that African Americans had the lowest number of myopes. A recent study by Vitale et al., [3] that investigated the importance of low blood vitamin D levels in the development of myopia found no evidence of a direct relationship. This study excluded the potentially confusing impact of outdoor activity, which may have contributed to the findings. Interestingly, the study in which myopia was artificially induced in tree shrews also failed to demonstrate a benefit from vitamin D3 therapy; this was the case, although the control animals in the experiment were not low in vitamin D3 [2], as it is seen in Table 1.
Similarly, a number of new animal model studies have provided evidence for the therapeutic potential of caffeine and its metabolite 7-methylxanthine (7-MX), which is a non-selective adenosine receptor antagonist [14], as it can be seen in Table 1. The results are consistent with those of earlier Danish pediatric clinical research utilizing oral 7-MX. That investigation revealed a relative reduction in axial elongation and the development of myopia, and these findings support that conclusion.
The long-term clinical investigations that Danish researchers have been doing on 7-MX tablets as a therapy for myopia are still ongoing. The investigations that were reported here were, regrettably, limited to using caffeine intake data from the NHANES survey since data on caffeine metabolites in urine are only available beginning in 2009, which is when assessments of refractive error were stopped. Chiang et al. [13] mentioned that, only two further thorough investigations of this publicly accessible NHANES dataset have been undertaken, to the best of the knowledge, in connection to the start and/or development of myopia and dietary factors. According to the NHANES study of adolescents and young adults that was part of the National Health and Nutrition Examination Survey, there was no correlation found between myopia and total zinc intake. There may be no immediate benefit from dietary supplements used to prevent or cure myopia [13], as it is seen in Table 1.
Because axial length data were inaccessible, the availability of objective refractive error data is an additional strength of the current research. This strength is bolstered by the large and ethnically diverse NHANES participant cohort as well as the analyses that are utilized within it. The dependability of the data was increased by the fact that all NHANES sites followed the same processes for obtaining measurements using predetermined protocols competent specialists carried out these procedures. The research does have several drawbacks, the most notable of which concerns the ethnic groups that were utilized during the study years that were analyzed. However, it is crucial to bear in mind that the research does have some problems. Considering the substantial prevalence of nearsightedness among Asian people, both in Asia and in the United States, the lack of a category labeled “Asian” is a fundamental weakness that has to be addressed.
It is probable that the inclusion of individuals of Asian ethnicity in the Other/Mixed ethnicity category explains why this group had the highest number of myopes [25]. As a result of the high prevalence of myopia in the population that served as the basis for the research, the collection of data on refractive errors was limited to children older than 12 years of age. This represents a time point that is later than the average age at which myopia first presents itself in children. This may help to explain why they found age to be only marginally significant in the multivariate modeling, although it has been proven to affect the refractive error in many of previous studies. In addition to this, it is probable that the dietary records that are maintained on adolescents will be different from the ones that are kept on younger children. Finally, it is essential to separate the possible confounding effects of outdoor activities when studying the association between blood vitamin D levels and myopia. However, information on sun exposure, outside activities, and collection season is missing from this dataset.
Despite this, there is still a lack of understanding of the many factors that may set off or intensify myopia. This is the situation due to the paucity of relevant research. Myopic patients often consult their doctors for advice on how to alter their daily habits in an effort to slow the progression of their condition. Although gender and age seem to have the most correlation, the findings presented here suggest that insulin levels may also play a key role in the onset of myopia and the degree to which it affects a person’s vision [26-28], as it can be seen in Table 1. There does not seem to be any additional strong links between myopia and dietary habits or other physical characteristics.
This meta-analysis may have been biased by a “healthy-user effect” or enhanced scrutiny. Despite the investigation of the results across three dimensions, the pooled observational data may be heterogeneous due to different populations analyzed or outcome criteria study design sample size and quality of the studies. Public data can’t be used to assess outcome definition homogeneity. A random selection of 10 of titles and numbers collected identified no conflicts, although having a single reviewer examine all data extraction and validity is a limitation. Publication bias affects observational meta-analyses most. Even though they requested unpublished material, observational studies with significant outcomes are more likely to be published, and thus they may be overrepresented in the meta-analysis, pooled effect sizes may be overstated by this bias. Updating this study is difficult due to limited literature. They added major new findings to the discussion after doing a fast Medline update search. In a recent meta-analysis of randomized controlled trials and observational studies, diet intake was not linked to myopia progression. The need for more research into other environmental factors, such as those related to the visual environment, is highlighted by the conflicting findings.
Conclusion
A good method for compiling data from several research is meta-analysis. It is only reliable, though, if the data from each research are comparable. Nutrition is one of the variables that determine relevant myopia progression rate, approaches that may accurately identify minute variations in refraction over time, as well as the use of suitable exclusion criteria. The studies that were analyzed in this meta-analysis provided a link between nutrition and myopia. Results, which include genetic factors as well as the impacts of outdoor activities, near-work activities, and the usage of screen devices, are generally in accordance with the findings of previous research. The following are some further repercussions that may be drawn from the findings.
To begin with, there was no indication that supplement usage reduced the development of myopia in school-aged children. This was the most significant finding. However, an alternative argument may be made, which suggests that the impact of food supplements may be both good and negative. This meta-analysis also suggests that a good diet is essential for health and wellbeing, a balanced diet also allows us to see well. Indeed, taking care of your eyesight also goes through the plate. Diet has a direct influence on visual health and some foods even preserve visual acuity while preventing eye disorders.
It is noteworthy that a trial in which tree shrews had their myopia artificially produced likewise failed to show a benefit from vitamin D3 treatment. Danish researchers are still conducting long-term clinical studies on 7-MX pills as a treatment for myopia. Unfortunately, since data on caffeine metabolites in urine are only available starting in 2009, which is when assessments of refractive error were terminated, the research that was described here was restricted to utilizing caffeine consumption data from the NHANES survey. The absence of an “Asian” category is a basic issue that has to be rectified given the significant incidence of nearsightedness among Asians, both in Asia and the United States.
The fact that people of Asian ancestry were counted under the Other/Mixed ethnicity category is probably what led to the largest number of myopia sufferers among this group. The group that served as the foundation for the study had a high prevalence of myopia, hence only children older than 12 were included in the data collection on refractive errors. This may help to explain why, despite the fact that age has been shown to affect refractive error in several prior research, they only found it to be weakly significant in the multivariate modeling.
Additionally, it is likely that the nutritional records collected on teenagers will differ from those kept on younger children. Finally, when examining the relationship between blood vitamin D levels and myopia, it is critical to isolate the potential confounding effects of outdoor activities. The results given here imply that insulin levels may also play a significant role at the beginning of myopia and the extent to which it impairs a person’s vision, although gender and age seem to have the most links.
References
- Sherwin JC, Mackey DA (2013) Update on the epidemiology and genetics of myopic refractive error. Expert Review of Ophthalmology 8(1): 63-87.
- Chua SY, Sabanayagam C, Tan CS, Lim LS, Toh JY, et al. (2018) Diet and risk of myopia in three-year-old Singapore children: the GUSTO cohort. Clinical & experimental optometry 101(5): 692-699.
- Vitale S, Sperduto RD, Ferris FL (2019) Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Archives of ophthalmology (Chicago, Ill.: 1960) 127(12): 1632-1639.
- Edwards MH (1996) Do variations in normal nutrition play a role in the development of myopia? Optometry and vision science: official publication of the American Academy of Optometry 73(10): 638-643.
- Han SB, Jang J, Yang HK, Hwang JM, Park SK (2019) Prevalence and risk factors of myopia in adult Korean population: Korea national health and nutrition examination survey 2013-2014 (KNHANES VI). PloS one 14(1): e0211204.
- Morgan IG, Wu PC, Ostrin LA, Tideman JWL, Yam JC, et al. (2021) IMI Risk Factors for Myopia. Investigative ophthalmology & visual science 62(5): 3.
- Werbach MR (2003) Myopia (nearsightedness) and diet. (Nutritional Influences on Illness). Townsend Letter for Doctors and Patients 237: 152-153.
- Xiang ZY, Zou HD (2020) Recent Epidemiology Study Data of Myopia. Journal of ophthalmology 2020: 4395278.
- Mahto H (2016) Natural Ways of Myopia Control: A Public Health Approach for the Prevention of Myopia. College of Optometry Pacific University. Oregon Thesis 34: 14.
- Kaiti R, Shyangbo R, Sharma IP, Dahal M (2021) Review on current concepts of myopia and its control strategies. International journal of ophthalmology 14(4): 606-615.
- Li M, Tan CS, Foo LL, Sugianto R, Toh JY, et al. (2022) Dietary intake and associations with myopia in Singapore children. Ophthalmic and Physiological Optics 42(2): 319-326.
- Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, et al. (2018) Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology 125(8): 1239-1250.
- Chiang SY, Weng TH, Lin CM, Lin SM (2020) Ethnic disparity in prevalence and associated risk factors of myopia in adolescents. Journal of the Formosan medical association 119(1): 134-143.
- Marks AR (2010) Nutrition, Vitamin D and Refractive Error (Doctoral dissertation, The Ohio State University). Columbus, Ohio, United States.
- Wang Y, Ding H, Stell WK, Liu L, Li S, et al. (2015) Exposure to sunlight reduces the risk of myopia in rhesus monkeys. PloS one 10(6): e0127863.
- Ashby R, Ohlendorf A, Schaeffel F (2009) The effect of ambient illuminance on the development of deprivation myopia in chicks. Investigative ophthalmology & visual science 50(11): 5348-5354.
- Read SA, Collins MJ, Vincent SJ (2015) Light Exposure and Eye Growth in Childhood. Investigative ophthalmology & visual science 56(11): 6779-6787.
- Berticat C, Mamouni S, Ciais A, Villain M, Raymond M, et al. (2020) Probability of myopia in children with high refined carbohydrates consumption in France. BMC ophthalmology 20(1): 1-8.
- Jiang N, Zhang G, Zhang L, Liu L (2020) Re: COVID-19, sweat, tear …and myopia?. Clinical & experimental optometry 103(5): 717.
- Hsu YA, Chen CS, Wang YC, Lin ES, Chang CY, et al. (2021) Anti-Inflammatory Effects of Resveratrol on Human Retinal Pigment Cells and a Myopia Animal Model. Current issues in molecular biology 43(2): 716-727.
- Burke N, Butler JS, Flitcroft I, McCartney D, Loughman J (2019) Association of Total Zinc Intake with Myopia in U.S. Children and Adolescents. Optometry and vision science: official publication of the American Academy of Optometry 96(9): 647-654.
- Ng FJ, Mackey DA, O Sullivan TA, Oddy WH, Yazar S (2020) Is Dietary Vitamin a Associated with Myopia from Adolescence to Young Adulthood? Translational vision science & technology 9(6): 29.
- Elliott JH, Synnot A, Turner T, Simmonds M, Akl EA, et al. (2017) Living systematic review: 1. Introduction-the why, what, when, and how. Journal of clinical epidemiology 91: 23-30.
- Harb EN, Wildsoet CF (2021) Nutritional Factors and Myopia: An Analysis of National Health and Nutrition Examination Survey Data. Optometry and vision science: official publication of the American Academy of Optometry 98(5): 458-468.
- Menéndez-Acebal C, Martínez-González MA, Bes-Rastrollo M, Moreno-Montañés J, García-Layana A, et al. (2021) The influence of alcohol intake in myopia development or progression: The SUN cohort study. Drug and alcohol dependence 229(Pt A): 109149.
- Abdel-Aal ESM, Akhtar H, Zaheer K, Ali R (2013) Dietary sources of lutein and zeaxanthin carotenoids and their role in eye health. Nutrients 5(4): 1169-1185.
- Li M, Tan CS, Foo LL, Sugianto R, Toh JY, et al. (2022) Dietary intake and associations with myopia in Singapore children. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians (Optometrists) 42(2): 319-326.
- Salehi A, Meamarzadeh SE, Akhlaghi M, Rismanchian A, Jafari A (2008) Effect of Ramadan fasting on physiologic myopia. Journal of Shahrekord Uuniversity of Medical Sciences 10.






























