Perioperative Corneal Injury: An Unseen Casualty of Covid-19
Cindy B Yeoh1*, Kenneth P Seier2, Jasmine Francis3, David H Abramson4, Kay See Tan5 and Luis E Tollinche6
1 Department of Anesthesiology and Critical Medicine, Memorial Sloan Kettering Cancer Center, New York
2 Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York
3 Ophthalmic Oncology Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York
4 Ophthalmic Oncology Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York
5 Department of Epidemiology and Biostatistics, Memorial Sloan Kettering Cancer Center, New York
6 Department of Anesthesiology, MetroHealth Medical Center of Case Western Reserve University, Ohio
Submission: November 10, 2021;Published: April 26, 2022
*Corresponding author: Cindy B Yeoh, Department of Anesthesiology and Critical Care Medicine, Memorial Sloan Kettering Cancer Center, New York
How to cite this article: Cindy B Y, Kenneth P S, Jasmine F, David H A, et al. Perioperative Corneal Injury: An Unseen Casualty of Covid-19. JOJ Ophthalmol. 2022; 9(2): 555757. DOI: 10.19080/JOJO.2022.09.555757
Abstract
Introduction: This study is the first to reveal an increased incidence in perioperative corneal injuries during the COVID era and should alert clinicians to this observation. This study could inform investigations into practice or patient factors that changed because of the COVID pandemic. We were aware of several adverse corneal injury reports during COVID and as a result did a formal IRB approved retrospective review to see if corneal injuries were more common during that period.
Methods: This is a retrospective cross-sectional observational study based on the hospital reporting. Of corneal injuries in the peri-operative time-period during the COVID pandemic. Comparison to known incidence of corneal injuries from the same institution in the pre COVID era were made. The objective was to examine if there were increased peri-operative corneal injuries during the COVID pandemic at Memorial Sloan Kettering Cancer Center (MSKCC).
Results: All corneal injury event reports were aggregated for the time including January 1, 2015, through April 30, 2021. Data include all patients who underwent anesthesia for any procedure at all sites within the hospital system.
Conclusion: This study reveals an increased incidence in perioperative corneal injuries during the COVID era and should alert clinicians to this observation. This study may inform investigations and may ultimately drive processes that could mitigate preventable causes of perioperative corneal injury.
Keywords: Perioperative; Corneal injury; COVID-19
Introduction
The first detected case of SARS-CoV-2 was reported in November of 2019 in Hubei province, China. Since then, SARS-CoV-2 has become a pandemic infection, that has infected 142 million people and caused 3.1 million deaths [1]. While pathognomonic symptoms of COVID-19 include fever, cough, shortness of breath, sore throat, and fatigue; gastrointestinal, renal, and neurologic manifestations are not uncommon, and more recently, ophthalmologic symptoms have also been described. Some of these ocular manifestations include dry eye, foreign body sensation, itching, blurring of vision, conjunctivitis, and photophobia. In a review article by Nasiri et al., it was reported that approximately one in ten patients with COVID-19 have at least one ocular symptom [2]. This rate was reported to be 20.5% based on a cross-sectional study by Bostanci Ceran [3]. Ocular manifestations associated with COVID-19 have been attributed to the potential route of SARS-CoV-2 on the ocular surface. The ocular surface is known to be vulnerable to respiratory viruses. Like the respiratory tract, corneal and conjunctival epithelia provide a mucosal pathway that allows for viral entry. Studies have shown that ACE2 facilitates viral entry and infection, and while it is expressed at a great level in heart and lung tissues, it is also expressed in the human cornea and conjunctiva [4]. At our Institution (Memorial Sloan Kettering Cancer Center) post anesthesia complications are routinely tabulated and investigated. We were aware of several adverse corneal injury reports during COVID and as a result did a formal IRB approved retrospective review to see if corneal injuries were more common during that period.
Methods
This retrospective cross-sectional observational study received approval from the Institutional Review Board at Memorial Sloan Kettering Cancer Center (New York, NY). IRB 21-104 (March 5, 2021). The requirement for written informed consent was waived by the IRB. The Strengthening the Reporting of the Observational Studies in Epidemiology (STROBE) statement was used to report this study, and the article adheres to the applicable guidelines [5]. Corneal injuries are reported at our institution through a centralized system that allows staff to report actual events and near misses. Reporting to Improve Safety and Quality (RISQ) corneal injury reports are reviewed by the Division of Quality and Safety in collaboration with Anesthesia. Departmental Quality Assurance Chairs to ensure accuracy. All corneal injury RISQ reports were aggregated for the time including January 1, 2015, through April 30, 2021. The RISQ reports include all patients who underwent anesthesia for any procedure at all sites within the hospital system.
Every RISQ report of corneal injury was investigated to verify accuracy of report. Each of these reports was independently verified by examination of the medical record by a staff anesthesiologist. Review was also conducted to ensure that each report reflected unique patients and that the same patient did not have repeat surgery (or complaints). Control plots were used to visualize the proportion of corneal abrasions and RISQ reports per month. Three-sigma rule is a threshold and defined as 3 times the standard deviation and was then used to identify months where the proportions were significantly higher than average [6]. Poisson regression models with an offset for total number of surgeries were used to model abrasion rate over time. Time was split into three groups 1) prior to March 2018, 2) March 2018 to Feb 2020, and 3) March 2020 to April 2021 to formally test if corneal abrasion and RISQ rates were increased during “COVID era”.
Results
Prior to March 2020, most months had 0% corneal abrasion rates except June 2015 (.03%), February 2016 (.06%), Sept 2017 (.03%), May 2018 (.02%), November 18 (.05%), May 19(.02%), and September 2019 (.02%) (Table 1). After March 2020 most months had > 0% corneal abrasion rates March 2020 (.23%), April 2020 (.06%), May 2020 (.11%), June 2020 (.05%), October 2020 (.19%), November 2020 (.12%), December 2020 (.02%), January 2021 (.02%), and February 2021 (.05%). Control plots were used to visualize the corneal abrasion rate and RISQ rate over time. The mean corneal abrasion rate was .01% and the upper limit sigma 3 was .13% and the mean RISQ rate was 5.29% and the upper limit sigma 3 was 7.22%. Two months were identified where corneal injury rates were significantly higher than average, March 2020, and October 2020. There were no months where RISQ rate was greater than the sigma-three threshold (Figures 1 & 2).
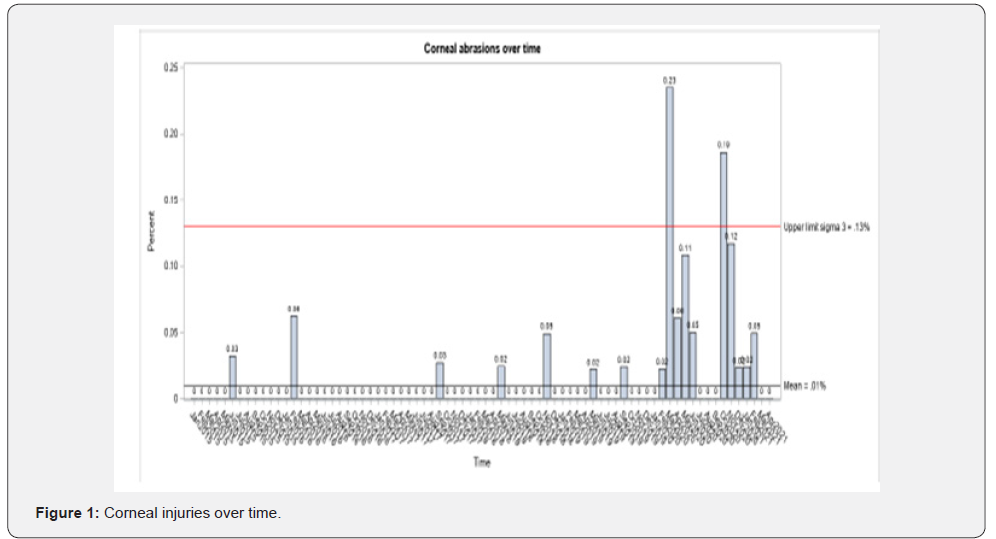
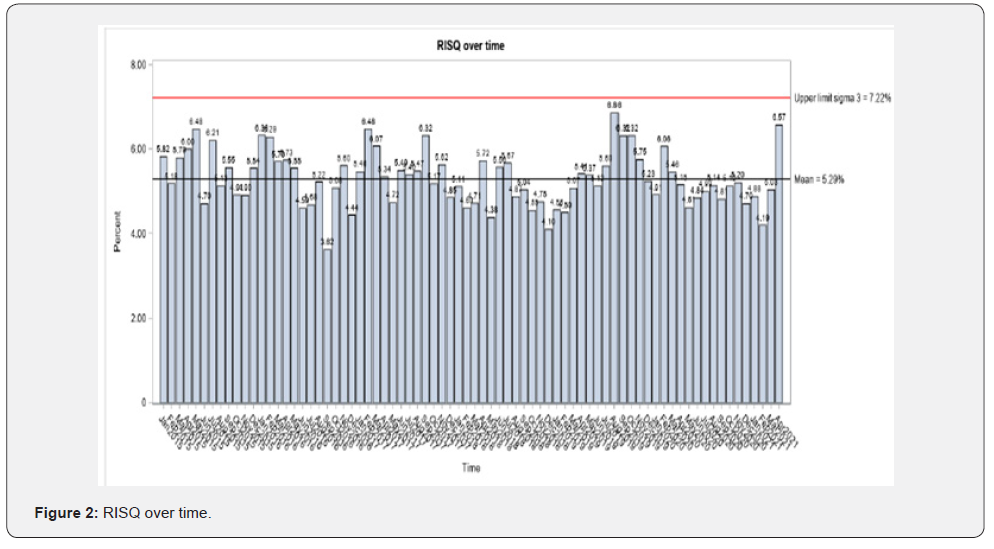
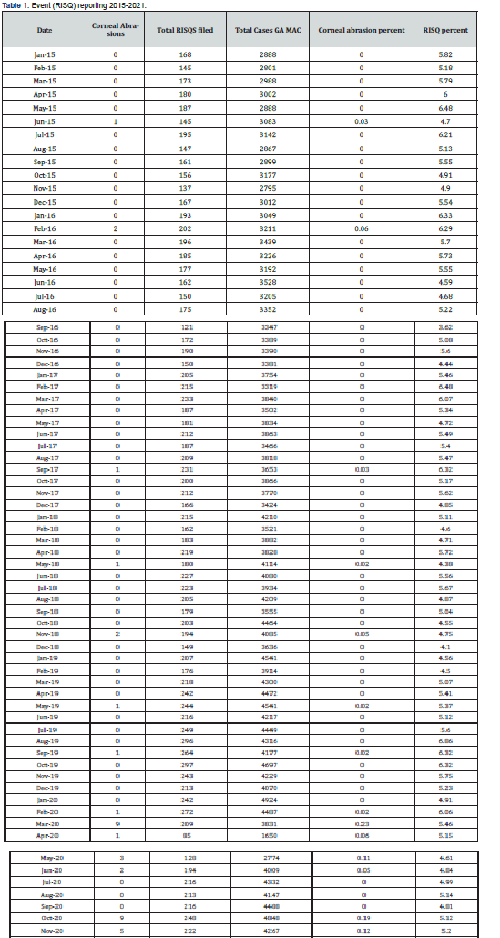
The occurrence for each bar being above the upper limit sigma 3 is rare, specifically has less than .003 probability. Corneal injury rates (in lieu of total number of events) were utilized to account for variation in perioperative volume. Using Poisson regression, we find that corneal injury rates were significantly higher after March 2020 compared to the other time points before February 2018 (rate ratio= 19.37; 95% CI (6.8-54.7); p<.001) and March 2018-Feb 2020 (rate ratio 19.27; 95% CI (4.3-24.5); p<.001). But corneal injury rates were not different between before February 2018 and between March 2018 and February 2020 (rate ratio = .53; 95% CI (.15-1.88); p=.326). Alternatively, RISQ reporting rates were significantly lower after March 2020 compared to other time points before February 2018 (rate ratio= .93; 95% CI (.89-.97); p=.001) and March 2018-Feb 2020 (rate ratio .95; 95% CI (.90-.99); p=.021). There was again no difference between before February 2018 and between March 2018 and February 2020 (rate ratio = 1.02; 95% CI (.98-1.06); p=.271) (Tables 2 & 3).

Discussion
At our institution, an increase in postoperative ocular complications was noted to coincide with the outbreak of COVID-19 in the United States. The most common postoperative ocular complication is a corneal injury due to corneal exposure, globe pressure, or direct mechanical/chemical trauma to the cornea during surgery and anesthesia. General anesthesia abolishes Bell’s phenomenon, which is the protective mechanism of upward movement of the eye upon eyelid closure, and significantly decreases tear production and tear film stability [7]. The incidence of perioperative corneal abrasion has been documented as ranging from 0.034-0.17% [8,9]. Ocular injuries account for 3-8% of anesthesia malpractice claims, of which 35% are perioperative corneal abrasions [10]. Other attributed causes of ocular complications during this pandemic include dry eye disease (computer or mask-induced), stress reactivation of ophthalmic herpes simplex virus (HSV) and herpes zoster virus (HZV), and central serous chorioretinopathy (CSC) due to physiologic stress [11]. Behavioral changes that were instituted to mitigate spread of infections have also been implicated such as the inadvertent introduction of hand sanitizer into the eye [11].
In this retrospective study, we sought to determine if there was a rise in reports of perioperative corneal injuries coinciding with the outbreak of COVID-19 in the United States in March 2020. Our source of corneal injury reports was the hospital event and near miss reporting system known as RISQ (Reporting to Improve Safety and Quality). Our data analysis supported a statistically significant uptick in perioperative ophthalmic injuries after March 2020. We recognized that the spike in ophthalmic complaints could be attributed to increased event reporting through RISQ. Therefore, we explored the rate of RISQ reporting over the same time periods used to study our corneal injury rates: before March 2018, March 2018 to Feb 2020, and after March 2020. We determined that RISQ reports did not change during this period overall and were able to exclude increased reporting as an explanation for the notable rise in cases of corneal injury. Similarly, to exclude the possibility of an increase in surgical volume resulting in a corresponding increase in corneal injuries, we used the rate of corneal injury instead of total number of cases to account for any changes in surgical volume between the comparative time groups.
In the perioperative period, unless intubated, all patients must don a mask whenever possible. In the immediate postoperative recovery period, application of face masks on patients can be challenging. Patients are often still sedated, and unable to notice or self-adjust a mask that has not been appropriately applied and may have shifted too close to the eyes thereby increasing the likelihood of scratching the corneal surface. As previously mentioned, dry eye disease (computer or mask-induced) is an identified cause of increased ocular complications during this pandemic. Pre-existing dry-eye disease may increase a patient’s risk for developing corneal injuries during the perioperative period. Widespread mask wear has been associated with an increased incidence of eye injuries such as chalazion [12].
Face masks significantly affect the direction of airflow from the mouth and nose. A poorly applied mask will force air upwards in the direction of the eyes. This constant stream of air over the surface of the eyes affects the ophthalmic tear film balance, predisposing individuals to increased eye irritation and susceptibilities [12]. Additionally, the application of supplemental oxygen via nasal canula under the face mask, serves to further disrupt tear film stability and exacerbate drying effects that predisposes to ophthalmic injuries. It is also plausible that susceptibility of the eye as a SARS-CoV-2 virus entry point, predisposes individuals with current or prior COVID-19 infections to increased ophthalmic complications in the perioperative period. Unfortunately, our study did not account for patient’s COVID-19 infection status. The increase in reporting of ophthalmic complaints during this pandemic has already been described in the literature, and the result from our study yields good evidence in support of these observations. The major weakness of our study is inability to establish causality. One possible mechanism to explain our findings is the advent of mask wearing but this study is unable to establish causality. We do not attempt to define a definitive mechanism but are instead interested in reporting the dramatic rise in corneal injuries and suggest a possible explanation. Another limitation is that incident reporting systems are qualitative and not quantitative measurement systems. As a result, our findings could be the result of reporters focusing specifically on corneal injuries more than on other incidents associated with anesthesia. This bias is unlikely given that there were no department wide initiatives or discussions surrounding corneal injuries in this time-period. Given that COVID increases other ocular manifestations independent of anesthesia, it is also theoretically possible that these injuries were pre-existing. This is unlikely, however, because these patients presented asymptomatically in advance of anesthesia. Finally, it is possible that the nature of surgery during the pandemic changed or that different staff were involved during the study time-period. An increase in procedures that were supine, or lateral could predispose patients to corneal injuries; NYC was the global epicenter of COVID during parts of the study period and many hospitals needed help from temporary staff. However, MSKCC, unlike other MSKCC institutions, did not have temporary help or substitute perioperative staff. Further, given the nature of the oncology mission, MSKCC was exempt from most of the surgical volume restrictions that other hospitals experienced. It is not felt that the type and proportion of surgical subspecialties changed sufficiently during the study period to explain these observations.
Conclusion
This study reveals an increased incidence in perioperative corneal injuries during the COVID era and should alert clinicians to this observation. Further studies will be necessary to establish cause and effect of mask-associated eye injuries and to elucidate the role of Sars-CoV-2 and infection status on the risk for ophthalmic complications [13-15].
Conflicts of Interest
LET is a grant recipient through Merck Investigator Studies Program (MISP) to fund clinical trial at MSKCC (NCT03808077). LET serves a consultancy and advisory role for Merck & Co. Pharmaceutical Company. LET serves a consultancy and advisory role for GE Healthcare.
Financial Support
1. Department of Anesthesiology and Critical Care Medicine Memorial Sloan Kettering Cancer Center, Research Fund
2. National Cancer Institute of the National Institutes of Health under Award Numbers R25CA020449 and P30CA008748
References
- Yeoh CB, Lee KJ, Rieth EF, Mapes R, Tchoudovskaia AV, et al. (2020) COVID-19 in the Cancer Patient. Anesthesia and analgesia 131(1): 16-23.
- Nasiri N, Sharifi H, Bazrafshan A, Noori A, Karamouzian M, et al. (2021) Ocular Manifestations of COVID-19: A Systematic Review and Meta-analysis. J Ophthalmic Vis Res 16(1): 103-112.
- Bostanci Ceran B, Ozates S (2020) Ocular manifestations of coronavirus disease 2019. Graefe's Archive for Clinical and Experimental Ophthalmology 258(9): 1959-1963.
- Sun Y, Pan X, Liu L, Ni R (2004) Expression of SARS coronavirus S protein functional receptor ACE2 in human and rabbit cornea and conjunctiva. Rec Adv Ophthalmol 24(5): 332-336.
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, et al. (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Annals of internal medicine 147(8): 573-577.
- Tennant R, Mohammed MA, Coleman JJ, Martin U (2007) Monitoring patients using control charts: a systematic review. International Journal for Quality in Health Care 19(4): 187-194.
- I C Francis, J A Loughhead (1984) Bell's phenomenon: a study of 508 patients. Australian Journal of Opthalmology 12(1): 15-21.
- Roth S, Thisted RA, Erickson JP, Black S, Schreider BD (1996) Eye injuries after nonocular surgery: a study of 60,965 anesthetics from 1988 to 1992. The Journal of the American Society of Anesthesiologists 85(5): 1020-1027.
- Cucchiara RF, Black S (1988) Corneal abrasion during anesthesia and surgery. Anesthesiology 69(6): 978-979.
- Gild WM, Posner KL, Caplan RA, Cheney FW (1992) Eye injuries associated with anesthesia a closed claims analysis. The Journal of the American Society of Anesthesiologists 76(2): 204-208.
- Yangzes S, Grewal S, Gailson T, Grewal SPS (2021) Hand Sanitizer–Induced Ocular Injury: A COVID-19 Hazard in Children. JAMA Ophthalmology 139(3): 362-364.
- Silkiss RZ, Paap MK, Ugradar S (2021) Increased incidence of chalazion associated with face mask wear during the COVID-19 pandemic. American Journal of Ophthalmology Case Reports 22: 101032.






























