Association of Body Mass Index, Blood Sugar and Glycated Hemoglobin Levels with Types of Macular Edema in Patients with Type-2 Diabetes Mellitus
Luxmi Singh1, Akansha Sharma2*, Pragati Garg3 and Ashutosh Chaturvedi4
Department of Ophthalmology, Era University, India
Submission:February 17, 2020;Published:August 20, 2020
*Corresponding author: Akansha Sharma, Department of Ophthalmology, Era’s Lucknow Medical College and Hospital, Era University, India JOJ Ophthalmol
How to cite this article:Luxmi S, Akansha S, Pragati G, Ashutosh C. Association of Body Mass Index, Blood Sugar and Glycated Hemoglobin Levels with Types of Macular Edema in Patients with Type-2 Diabetes Mellitus. JOJ Ophthalmol. 2020; 8(4): 555741.DOI: 10.19080/JOJO.2020.08.555741
Abstract
Introduction: Diabetes mellitus (DM) is a metabolic disease defined by elevated blood glucose. DM is a global epidemic and the prevalence is anticipated to continue to increase.
Material & Methods: After ethical approval and taking consent 130 patients with macular edema of type 2 Diabetes Mellitus (>18 years) attending were included. In this hospital-based cross-sectional study, the patients had preliminary demographic and medical evaluation along with history taking, anthropometric, complete ophthalmological and hemo-dynamic assessment were also done.
Observation & Results: There was a statistically significant trend of increasing proportion of cystoid and serous macular edema from early and simple macular edema with increasing HbA1c levels (p<0.001).
Conclusion: Keeping in view a wide spectrum of severity grades of OCT based diabetic macular edema and only a few cases in some categories (serous macular edema), the findings of present study should be considered as a preliminary attempt. Further studies on a larger population are recommended
Keywords:Retinopathy; Macular Edema; Optical coherence tomography
Introduction
Diabetes mellitus (DM) is a metabolic disease defined by elevated blood glucose. DM is a global epidemic and the prevalence is anticipated to continue to increase. DM is can be further classified as type 1 (T1DM), which causes pancreatic beta cell failure due to which insufficient insulin is type 2 (T2DM) is characterized by insulin resistance [1]. Type II diabetes is most dominant form of diabetes contributing for almost 90% of total burden of diabetes [2]. Diabetic retinopathy is a cause of visual loss on a global scale. The pathology is closely associated with vascular, glial, and neuronal components of the diabetic retina. Treatments for the vision-threatening complications of diabetic macular edema and proliferative diabetic retinopathy have greatly improved. As per recent studies, diabetes markedly impacts the retinal neurovascular unit and its interdependent vascular, neuronal, glial, and immune cells [3]. Laboratory and clinical evidence show that, microvascular changes, inflammation and retinal neurodegeneration may contribute to diabetic retinal damage in the early stages of diabetic retinopathy [4].
Clinically, diabetic changes in the retina can be divided into two stages: non-proliferative diabetic retinopathy and proliferative diabetic retinopathy. Early stage of DR is represented by NPDR, wherein the pathology is increased vascular permeability and capillary occlusion. During this stage, the fundus findings include microaneurysms, hemorrhages and hard exudates while the patients may be asymptomatic4. Proliferative diabetic retinopathy is an advanced type of DR, the patients may experience severe vision impairment. This stage is characterized by neovascularization [4]. However, in addition to hyperglycemia, other factors like hypertension, dyslipidemia, and particularly the genetic load, have an immense influence on the severity and clinical course of diabetic retinopathy (DR) [5]. Using OCT, DME can be classified into four main types presented as the OCT Classification of Diabetic Macular Edema given by Koleva-Georgieva: [6]
Type 1: Early diabetic macular edema
Type 2: Simple diabetic macular edema
Type 3: Cystoid diabetic macular edema:
3a, mild.
3b, intermediate.
3c, severe
Type 4: Serous macular detachment
Materials and Methods
The study is a hospital-based cross-sectional study. 130 diabetic patients who were attending the Outpatient Department of Ophthalmology and Outpatient Department of Medicine of our tertiary center, referred to Outpatient Department of Ophthalmology of our tertiary center were evaluated. The retinal/ macular changes were evaluated and were included in the study. Patients with macular edema of type 2 Diabetes Mellitus (>18 years) attending Ophthalmology and Medicine OPD of our tertiary health center were included. The exclusion criteria comprised of patients who had gestational DM, undergone any intra-ocular laser treatment or intra-ocular injection in the past 3 months, patients suffering from non-diabetic maculopathy (age-related macular degeneration / macular dystrophy), patients who have undergone any intraocular surgery in the past 3 months, patients with history of intake of drugs like corticosteroids, nephrotoxic in the past 3 months or any non-diabetic renal disease and patients with significant media haziness preventing adequate visualization of the fundus. Informed and written consent was obtained from the all the patients. All the patients were given the freedom to withdraw from the study, if they wished so.
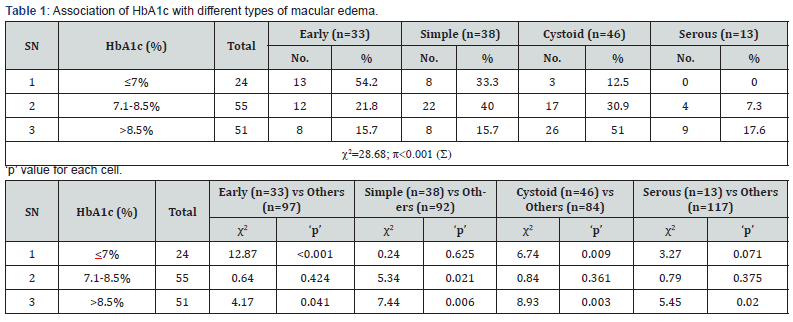
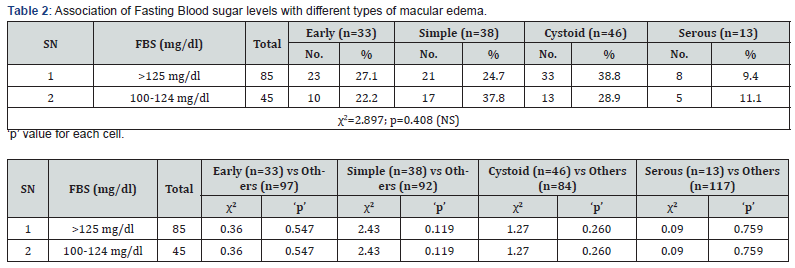
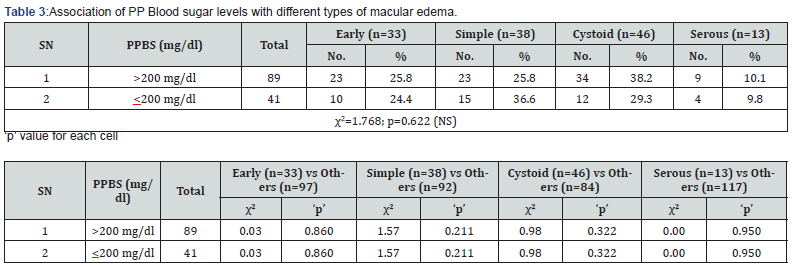
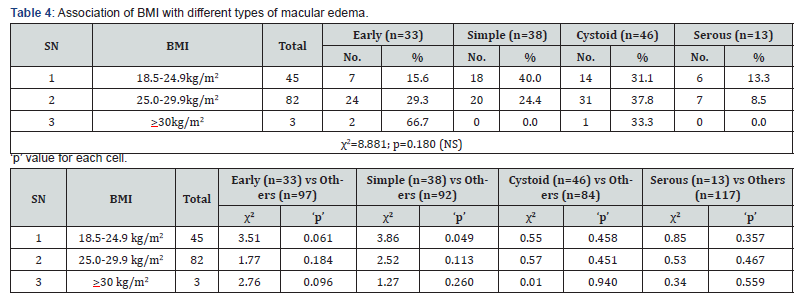
The patients included underwent a series of examinations; their best corrected visual acuity was measured using Snellen’s chart for both the eyes, which was followed by torch light examination, distant direct ophthalmoscopy, slit lamp examination, fundus evaluation by direct ophthalmoscope and fundus photography by Zeiss. Goldman’s Applanation Tonometer was used to measure the intraocular pressure (IOP). Macular edema and its severity were assessed and evaluated by using Optical Coherence Tomography (OCT) following the criteria described by Koleva-Georgieva. The patients under evaluation were subjected to preliminary demographic and medical evaluation and history taking, anthropometric and hemo-dynamic assessment were also assessed. Analysis of the data assessed was done using the Statistical Package for Social Sciences, version 21.0 or above (Tables 1-8).
Observations & Results
Among males, cystoids macular edema was most common (37.3%) followed by simple (32%), early (20%) and serous macular edema (10.7%) whereas among females early and cystoid macular edema (32.7%) were most common followed by simple (25.5%) and serous macular edema (9.1%). However, on evaluating the data statistically, no significant association between types of macular edema and gender was observed (p=0.430).
A dominance of early and simple macular edema types in age group 41-50 years and 51-60 years and a dominance of cystoid and serous macular edema in age group 61-70 years was seen. It was seen that proportion of those with early macular edema showed a declining trend with increasing age whereas other macular edema types showed an increasing trend with increasing age. Serous edema was present in only 61-70 years old patients. Statistically, the relationship between age and type of edema was significant (p=0.003).
In the normal weight group (BMI 18.5-24.9 kg/m2), maximum (40%) had simple macular edema followed by cystoid (31.1%), early (15.6%) and serous (13.3%) macular edema. In overweight group (BMI 25.0-29.9 kg/m2) too, maximum had cystoid macular edema (37.8%) followed by early (29.3%), simple (29.3%) and serous macular edema. In obese (>30 kg/m2) group, out of 3 patients, 2 (66.7%) had early macular edema while 1 (33.3%) had cystoid macular edema. On evaluating the data statistically, we did not find a significant association between BMI and types of macular edema (p=0.180).
Among those with HbA1c <7%, majority had early macular edema (54.2%) followed by simple (33.3%) and cystoid (12.5%) macular edema. Among those with HbA1c 7.1-8.5%, maximum had simple macular edema (40%) followed by cystoid (30.9%), early (21.8%) and serous (7.3%) macular edema. On the other hand, among those with HbA1c >8.5%, majority had cystoids macular edema (51%) followed by serous (17.6%), early and simple macular edema (15.7% each) respectively. Thus, there was a statistically significant trend of increasing proportion of cystoid and serous macular edema from early and simple macular edema with increasing HbA1c levels (p<0.001). Among those with fasting blood sugar >125 mg/dl, maximum (38.8%) had cystoids macular edema followed by early (27.1%), simple (24.7%) and serous (9.4%) macular edema respectively whereas among those with fasting blood sugar 100-124 mg/dl, maximum had simple macular edema (37.8%) followed by cystoid (28.9%), early (22.2%) and serous macular edema (11.1%) respectively. On evaluating the data statistically, there was no significant association between fasting blood sugar levels and types of diabetic macular edema.
Among those with post-prandial blood sugar levels >200 mg/dl, maximum (38.2%) had cystoid macular edema followed by early and simple macular edema (25.8%) and serous (10.1%) macular edema respectively whereas among those with blood sugar levels <200 mg/dl, maximum (36.6%) had simple macular edema followed by cystoid (29.3%), early (24.4%) and serous macular edema (9.8%) respectively. On evaluating the data statistically, the association between post-prandial blood sugar levels and types of macular edema was not found to be significant (p=0.622)./
Discussion
Glycemic control is an important risk factor associated with diabetic macular edema. Chronic hyperglycemia could damage the vascular endothelial cells and affects the integrity of bloodretinal barrier (BRB), which in turn results in fluid extravasation that is manifested as macular edema. In more specific terms, “hyperglycemia leads to an accumulation of free radicals and advanced glycemic end-products (AGE’s) and gluco-toxins, which form cross-links on proteins, lipids, and nucleic acids to alter the structure and function of these components within the BRB” [7]. HbA1c is a known marker of glycemic control over long term. Several studies show that odds of macular edema are 1.08 to 1.73 times higher for every 1% increase in HbA1c [8-12]. Romero- Aroca et al.12 in their study reported found the odds of macular edema to be 4.01 times higher among those with HbA1c >7% as compared to those having HbA1c <7%.
Jew OM et al, [13] evaluated the risk factors for clinically significant macular edema amongst patients in type 2 diabetes in a case control study involving 150 patients with bilateral non-proliferative diabetic retinopathy (NPDR) and CSME in either eye were compared to 150 patients with bilateral NPDR and no CSME in both eyes. The study reported CSME group to have a significantly higher HbA1c and FBG (P<0.05). The authors did not find any significant difference for BMI while, multiple logistic regression analysis showed that HbA1c had significantly high odds of developing CSME. Kamoi K et al, [14] performed a study to identify the most significant risk factors for in clinically significant macular edema type 2 diabetes mellitus and retinopathy, using optical coherence tomography in 7 subjects with clinically significant macular edema (group 1) and 124 without any clinically significant macular edema (group 2) diabetic retinopathy patients. Body mass index was found to be a significantly (p <0.001) negative predictor.
The study by Varma et al, [15] suggested a greater burden of DME among non-Hispanic blacks, individuals with high levels of HbA1c, and those with longer duration of diabetes. The study by Leveziel N et al, [16] found that 355 (12.6%) persons with type-2 diabetes also had diabetic macular edema, and diabetic macular edema had independent and significant association with age, duration of diabetes, HbA1c, systolic blood pressure, and stage of diabetic retinopathy. Prakash & Kothari [17] conducted a study among 170 type 2 diabetes mellitus patients and found out that the mean HbA1c levels were significantly higher in clinically significant macular edema group (10.09±1.74) as compared to non- clinically significant macular edema group (8.90±2.18).
Martín-Merino E et al, [18] examined the risk factors associated with the development of diabetic macular edema among patients diagnosed with type 2 diabetes in a case-control study of 2405 subjects divided in two groups of 211 diabetic macular edema patients and 2194 controls. They reported that diabetic macular edema increased with high HbA1c≥7%.
Singh et al, [19] found that cystoid macular edema and serous retinal detachment were associated with increased fasting and post prandial blood sugar levels respectively. The findings of present study, we assessed the prevalence of different types of diabetic macular edema based on OCT evaluation and to find out various risk factors associated with them. Keeping in view a wide spectrum of severity grades of OCT based diabetic macular edema and only a few cases in some categories (serous macular edema), the findings of present study should be considered as a preliminary attempt. Further studies on a larger population are recommended.
Conclusion
The results of this study depict that a substantial fraction of diabetic patients with macular edema have major association with old age, increased blood sugar fasting and post prandial blood sugar levels, glycated hemoglobulin and body mass index. Glycemic control and adoption of a healthy lifestyle are found to be of paramount importance in diabetic patients in order to avoid macular edema. Regular ophthalmic evaluation and routine follow-up should be made essential for assessment of diabetic patients especially who have had diabetes since a prolonged period.
References
- Vieira-Potter V, Karamichos D, Lee D (2016) Ocular Complications of Diabetes and Therapeutic Approaches. BioMed Research International 1-14.
- Saini JS, Khandalavla B (1995) Corneal epithelial fragility in diabetes mellitus, Canadian Journal of Ophthalmology 30(3): 142-146.
- Duh E, Sun J, Stitt A (2017) Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight 2(14): e93751.
- Wang W, Lo A (2018) Diabetic Retinopathy: Pathophysiology and Treatments. International Journal of Molecular Sciences19(6):1816.
- Corcóstegui B, Durán S, González-Albarrán M, Hernández C, Ruiz-Moreno J, et al. (2017) Update on Diagnosis and Treatment of Diabetic Retinopathy: A Consensus Guideline of the Working Group of Ocular Health (Spanish Society of Diabetes and Spanish Vitreous and Retina Society). Journal of Ophthalmology1-10.
- Koleva-Georgieva, Desislava, Sivkova, Nelly (2008)Types of diabetic macular edema assessed by optical coherence tomography. Folia medica50(3): 30-38.
- Sinclair SH, Nesler C, Foxman B, Nichols CW, Gabbe S (1984) Macular edema and pregnancy in insulin-dependent diabetes. Am J Ophthalmol97(2):154-167.
- Xu J, Xu L, Wang YX, You QS, Jonas JB, et al. Ten-year cumulative incidence of diabetic retinopathy. The Beijing Eye Study 2001/2011. PLoS One9(10):e111320.
- Jin P, Peng J, Zou H, Wang W, Fu J, et al. (2014) The 5-year onset and regression of diabetic retinopathy in Chinese type 2 diabetes patientsPLoS One9(11):e113359.
- Tam VH, Lam EP, Chu BC, Tse KK, Fung LM (2009) Incidence and progression of diabetic retinopathy in Hong Kong Chinese with type 2 diabetes mellitus. J Diabetes Complications23(3):185-193.
- Kajiwara A, Miyagawa H, Saruwatari J, Kita A, Sakata M, et al. (2014) Gender differences in the incidence and progression of diabetic retinopathy among Japanese patients with type 2 diabetes mellitus: a clinic-based retrospective longitudinal study. Diabetes Res Clin Pract103(3):e7-10.
- Henricsson M, Nystrom L, Blohme G, Ostman J, Kullberg C, et al. (2003) The incidence of retinopathy 10 years after diagnosis in young adult people with diabetes: results from the nationwide population-based Diabetes Incidence Study in Sweden (DISS) Diabetes Care26(2):349-154.
- Jew OM, Peyman M, Chen TC, Visvaraja(2012) SRisk factors for clinically significant macular edema in a multi-ethnics population with type 2 diabetes. Int J Ophthalmol5(4):499-504.
- Kamoi K, Takeda K, Hashimoto K, Tanaka R, Okuyama S (2013) Identifying risk factors for clinically significant diabetic macula edema in patients with type 2 diabetes mellitus. Curr Diabetes Rev 9(3):209-217.
- Tudor SM, Hamman RF, Baron A, Johnson DW, Shetterly SM (1998) Incidence and progression of diabetic retinopathy in Hispanics and non-Hispanic whites with type 2 diabetes. San Luis Valley Diabetes Study, Colorado. Diabetes Care21(1):53-61.
- Nicolas Leveziel, StéphanieRagot, Elise Gand, Olivier Lichtwitz, Jean Michel Halimi, et al. (2015) Association Between Diabetic Macular Edema and Cardiovascular Events in Type 2 Diabetes Patients: A Multicenter Observational Study. Medicine (Baltimore)94(33):e1220.
- Prakash GS, Kothari M (2016) Risk Factors Associated with Clinically Significant Macular Edema in Patients with Type 2 Diabetes Mellitus. International Journal of Scientific Study 3(12): 120-124.
- Martín-Merino E, Fortuny J, Rivero-Ferrer E, Lind M, Garcia-Rodriguez LA (2017) Risk factors for diabetic macular oedema in type 2 diabetes: A case-control study in a United Kingdom primary care setting. Prim Care Diabetes11(3):288-296.
- Singh L, Mullick R, Ahmed L, Garg P, Lal BB (2018) Diabetic macular edema and its association to systemic risk factors in an urban north Indian population. J Clin Ophthalmol2(2): 86-91.






























