Results of Scharioth Macular Lens Implant in 10 Patients with Age-Related Macular Degeneration. Uncontrolled Clinical Trial
Felipe B De Medeiros, Paulo Bernardo F Rebelo, Francisco Porfirio Neto and Hilton A G De Medeiros*
Núcleo Bandeirante, Distrito Federal, Brazil
Submission: January 11, 2019; Published: January 18, 2019
*Corresponding author: Hilton A G De Medeiros, Núcleo Bandeirante, Distrito Federal, Brazil
How to cite this article: Felipe B D M, Paulo B F R, Francisco P N, Hilton A G D M. Results of Scharioth Macular Lens Implant in 10 Patients with Age- Related Macular Degeneration. Uncontrolled Clinical Trial. JOJ Ophthal. 2019; 7(2): 555710. DOI: 10.19080/JOJO.2019.07.555710
Abstract
Ten pseudophakic patients with DMRI were submitted to the implantation of intraocular SML in the dominant eye in the period of December of 2017 to the March of 2018. All the patients had answered the Low-Vision Quality of Life Questionaire (LVQOLQ) before and after the surgery, with interval of 30 days.
Keywords: Macular Lens; Clinical trial; Surgery; Intraocular lenses; Astigmatism; Endothelial contact; Glaucoma; Acrylic lens; Pseudophakic eyes; Peripheral vision; Binocularity; Dominant eye; Fluorescein angiography; Cataract surgery; Emmetrope; Zonular dialysis; Uveitis; Glaucoma; Corneal opacification; Vision
Abbreviations: NVA: Near Visual Acuity; LVQOLQ: Low-Vision Quality of Life Questionaire; AMD: Age-Related Macular Degeneration; SML: Scharioth Macula Lens; DVA: Distance Visual Acuity; SD-OCT: Spectral Domain Optical Coherency Tomography; IOPA: Intraocular Pressure Average
Introduction
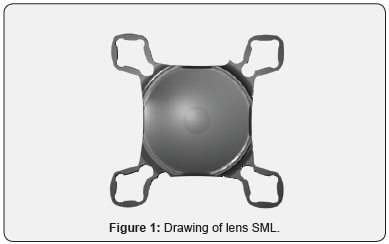
The Age-Related Macular Degeneration (AMD) is a debilitating chronic illness considered one of the most important causes of legal blindness in the world [1]. Image magnification devices have been the main method of assistance to these patients, but most of them have the inconvenience of being external and heavy, as magnifying glasses and telelupes [2]. Several drawings of intraocular lenses have been tested as an option to help these patients. However, most of them face problems, either of difficult implantation for being large devices, which generates important after-surgical astigmatism, either of the risk of endothelial contact or increase in the incidence of post-operative glaucoma [3]. Age-related macular degeneration, as a disease of great impact and high incidence in the elderly population, requires an easily reproducible treatment with a low learning curve. The Scharioth Macula Lens (SML) is an intraocular hydrophilic acrylic lens with a central button of 1,5mm and magnification of + 10.0D (Figure 1), it has four haptics of sustentation for positioning in the ridge on pseudophakic eyes [4]. SML does not affect the peripheral vision and binocularity; it only reduces the reading distance [4].
Patients and Methods
One well-experienced surgeons performed SML implantation in the dominant eye of ten pseudophakic patients with AMD in the period of December of 2017 to the March of 2018. Written informed consent was obtained from all patients after oral explanation of the purpose and complications of the surgery, and the surgeries were carried under topical anesthesia without occurrences of intraoperative complications. The inclusion criteria were bilateral presence of AMD with visual acuity in optimum eye better than 1.4 Log Mar, for Distance Visual Acuity (DVA), better than 2 letters ETDRS, for Near Visual Acuity (NVA), get visual improvement at 15cm with the use of a +6.00D external lens. In addition, all patients were pseudophakic with monofocal IOL implant at least 6 months prior to SML implantation. Patients with history of complications, modified intraocular pressure, corneal leukomas or activity of the AMD proved by the OCT were excluded from the study.
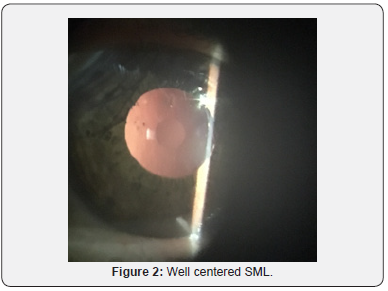
All the patients were previously submitted to fluorescein angiography and Spectral Domain Optical Coherency Tomography (SD-OCT) for evaluation of the stability of the AMD and had answered to the Low-Vision Quality of Life Questionaire (LVQOLQ) [5] before and after the surgery, with interval of 30 days in the same local of application and orientation of the same technician. The average age was of 71 years, varying from 64 to 93 years, being 5 females and 5 males. The average prior to surgery Intraocular Pressure Average (IOPA) measured by applanation tonometry was of 16 mmHg varying from 12 to 18mmHg. Mean DVA was 1.1 Log Mar, varying from 1.4 to 0.9, and the mean NVA was 5 letters ETDRS varying from 3 to 6 letters, and the median LVQOLQ score was 59 points, varying from 48 to 63 (Figure 2).
Results
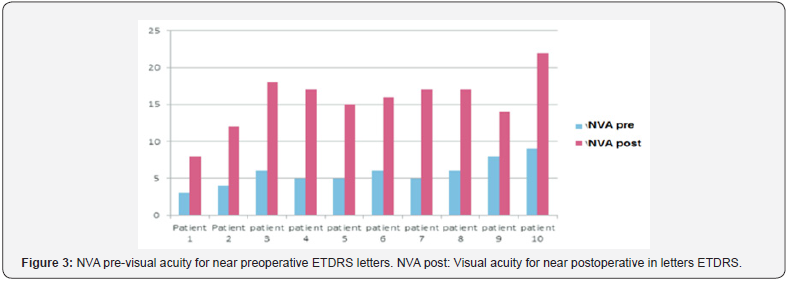
There were no intra or post-operative complications during our analysis. The average intra-ocular pressure after surgery was the same as noticed before, 16mmHg varying of 12 the 18mmHg, and none of the patients had complains about worsening of DVA. The results showed a statistically significant improvement (p< 0.05) in the NVA, without interference in the vision for far. The mean postoperative DVA was 1.0 Log Mar, ranging from 1.4 to 0.8, while the mean NVA was 15 ETDRS letters ranging from 8 to 18 letters (Figure 3). All patients had improvements in LVQOLQ, the average postoperative score was 74 points. When analyzing only the “Reading and Fine Work” questions of the questionnaire there was significant improvement as well (p< 0,05). Curiously, some patients had also mentioned improvement in some item that evaluate the DVA, specifically in the parts that evaluates the vision in general, appreciation of the images in the television and objects in movement, however it was not possible to measure such fact.
Discussion
Several intraocular devices have already been tested for improvement in visual capacity in patients with AMD. The great advantage of SML over previous devices is that its implantation very similar to any other IOL, consequently, there is almost no learning curve and can be implanted in incisions smaller than 3mm [6]. Another advantage is not having the risk of developing pupillary blockage, therefore, does not require iridotomy [7]. Although some authors have related piggyback lenses to be associated with pigmentary dispersion and increased intraocular pressure [8], lenses with characteristics proper to implants in the ciliary sulcus have demonstrated a reduction in pigment dispersion [9]. Moreover, in our sample no patient presented IOP increase postoperatively.
Another advantage of SML is to allow the visualization of the fundus of the eye and, thus, monitoring of the AMD, including with the accomplishment of complementary exams like OCT [10]. Although the SML lens can be placed at the same moment of cataract surgery with an intraocular lens “in the bag”, it is important to emphasize the need for a good biometric calculation, because, in order to achieve the best possible result, it is necessary that the patient is close to emmetrope [11]. The main contraindications for SML implantation are complicated cataract surgery, with an out-of-capsular lens, zonular dialysis, uveitis, chronic narrow-angle glaucoma, corneal opacification, AMD with active neovascular membrane and patients who do not understand the implant’s principles [4]. Even the SML implant does not interfere with DVA, we observed a qualitative improvement in the responses to LVQOLQ. Theoretically, devices with the principles of the Galileo telescope can promote improvement in vision for distance, but with a reduction in the visual field and visual impairment [12]. We believe that, in our series, the improvement observed may be related to the degree of satisfaction of the patient, which induces a better psychological state.
In his original work, Scharioth [4] reports an expressive improvement in NVA, which is easily explained by the characteristics of SML, however, there was no mention of improvement in DVA, or at least as for the improvement in the quality of life. The selection of the ideal candidates for the SML implant is another important factor. In our work we followed the recommendation initially described by Scharioth [4] and placed as VA cut point from Log Mar 1.4 to far, and 2 letters ETDRS with the addition of + 6.00D at 15cm distance. This allows to extrapolate the use of SML to other pathologies with low central visual acuity. We recently implanted SML in two patients with Recurrent Macular Hole and in one patient with Diabetic Macular Edema refractory to treatment with intraocular anti-angiogenic, drug delivery devices and vitrectomy. In all cases we obtained significant improvement for near. Although it is not the subject of this study, we believe that the information is relevant.
In summary, there was an improvement in the quality of life and in the NVA in the postoperative period, when compared to the preoperative period. Although SML implantation appears to be a good and safe option for improving NVA in selected patients with AMD, further studies are yet to be done to demonstrate the efficacy of this lens in the long term.
Discussion
What was known
a) Magnification could improve near vision and reading ability in patients with AMD.
b) A specially designed IOL with a central magnifying portion implanted in the ciliary sulcus of pseudophakic eyes can improve near vision in patients with AMD.
What this paper adds
a) Scharioth Macular Lens improves near vision in some AMD patients.
b) Scharioth Macular Lens can enhance some patient’s quality of life.






























