Corneal Perforation of Mooren’s Ulcer In Melanoderm: About 13 Cases
Boni S, Ouffoue YG*, Ouattara Oas, Konan AJ, Koman CE, Kouassi LJ, Gbe K, Cheucheu W, Gombe E, Ouonnebo L, Agbohoun RP and Fanny A
University of Felix houphouet boigny, Abidjan
Submission: September 18, 2017; Published: October 27, 2017
*Corresponding author: Ouffoue YG, University of Felix houphouet boigny, Abidjan, Email: ghisouffoue@yahoo.fr
How to cite this article: Boni S, Ouffoue Y, Ouattara O, Konan A, Koman C, et al . Corneal Perforation of Mooren’s Ulcer In Melanoderm: About 13 Cases. JOJ Ophthal. 2017; 5(3): 555661. DOI: 10.19080/JOJO.2017.05.555661
Introduction
Mooren'sulcer (MU) is a peripheral or marginal corneal ulceration looking like a crescent whose anterior margin forms a very characteristic promontory over hanging the bottom of this ulceration [1]. Evoked for the first time by Bowman in 1849 through one case report, MU was described in 1867 as a single clinicalentity by Mooren. It belongs to the group of peripheral ulcerativekerat it is and occurs completely in absence of any diagnosable system icd is order that could be responsible for the progressive destruction of the cornea. It is a rare pathology but its frequency seems to be higher in Africa, China and India than in northen hemisphere. The exact pathophysiology remains uncertain, although there is evidence suggesting an auto immune basis. Mooren'sulceris a painful, relentless, chronic ulcerativekerat it is which begins peripherally and progresses in three directions:circumferentially, centrally and in depth. The clinical presentation is a redeye with photophobia, watering and visual impairment and the diagnosis requires exclusion of the other disorders that could be responsible for the progressive destruction of the cornea. At last with any treatment, this pathology can progress and reaches descemetocele and corneal perforation. The management of MU is very difficult with no codification and requires medical and surgical procedures at the stage of perforation. Recurrence is frequent and the prognos is could therefore be threatened. Epidemiological, clinical and the rapeutical datas of perforated Mooren'sulcer are scarce, especially in West Africa and mainly in Cote d'Ivoire. So it seems fairly reasonable to bring our contribution to the evaluation of this pathology through the description of epidemiologicfeatures, clinics aspects, our practice therapeutic approaches in the aim to appreciate evolution and prognosis of MU at the stage of perforation in african black people.
Patients And Method
We performed a prospective study from January 2010 to January 2016 in the university hospital of Treichville in Abidjan. This study obtained the approval of the local ethics committee. After a complete eye examination, African black people suffering of Mooren'sulcer and presenting perforated cornea at presentation were included in the study. The patients had to under go medical and surgical treatment with a regular following during the study period. They received topical corticosteroids before the surgical treatment. This surgical procedure was conjunctive ctomy associated with either corneal sutures or amniotic graft. Post operative treatment was topical corticosteroids and eye drops of cyclophosphamide at 1% obtained by magisterial preparation. Statistical analysis was performed with Epi InfoTM 7 software in its 1.3.3 version (CDC, Atlanta). Descriptive analysis was carried out and p < 0,05 was considered statistically significant.
Results
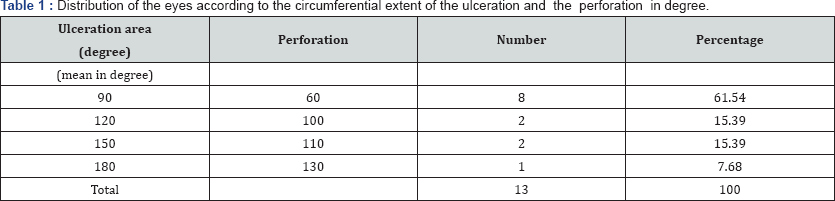
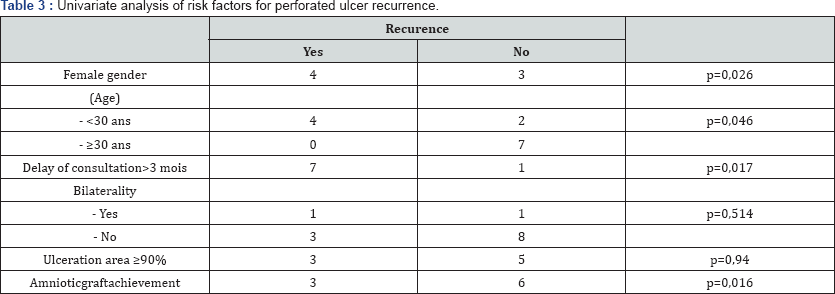
Thirteen eyes of eleven patients with 2 bilateral cases were involved during this period of 6 years. The mean age was 29.54 years with extremes of 21-38 years and the sex ratio was 0.57. Any previous ocular health history was found among 69.23 % of patients while past history of pterygium surgery and ocular burn were respectively seen in 23.08% and 7.69% of cases. We observed a delay in reaching out the hospital center in 61.54 % of cases and blindness (visualacuitylowerthan 1/20) was found in 9 eyes where as 4 eyes were in visual impairment (visualacuity between 1/20 and 3/10). Corneal perforation was located in nasal sector in 61.54 % of cases, this perforation mean size was lower than the associated ulcer as seen in Table 1. Conjunctivectomy combined with corneal sutures was performed in 76.92% of cases and amniotic graft in 23.08%. We noticed a improvement of visual acuity between one line and four lines after treatment in 53.85% of cases whereas the visual acuity was stationary in 38.46%of cases. After medical and surgical procedures 30.77% of patients presented legal blindness and the Table 2 shows final visual acuity. No complication was observed in 10 eyes while cataract and uveitis were respectively seen in two and one eye. 30.77% of cases experience drecurrence and the univariate analysis (Table 3) showed that the risks factors of recurrence were the female sex, a age under 30 and a delay of consultation more than 3 months. Amniotic graft (AG) was more reliable than corneal suture because when AG is not achieved, there is a great risk of recurrence.

Discussion
Mooren'sulcer is a rare affection with many disparities concerning epidemiology, clinical features, the rapeutic approaches and prognosis. These disparities refer mainly to the geographics areas of the world. In Northen Hemisphere countries, this pathologyis not very frequent with a slow progression and barely reaches the perforation stage. On the contrary, it is most frequent in China, India and West Africa and it affects young people, is more aggressive with a rapid evolution towards perforation (Figure 1). The last disparity is about treatment, nothern countries where MU is less severe offer keratoplasty, the gold standard treatment not available yetin many countries in West Africa. The mean age of the study population was 29.54 years with extremes of 21 and 38 years. This is similar to Fasina's study mean age [4] in Nigeria (30.9years), but is lower than Chen's study mean age [5] in China (48, 4 years). Thus, in light of these studies, the young age of people with Mooren'sulcerin Africa is «currently seen». In our study, some patients had a previous ocular health history of pterygium surgery and ocular burn. Many authors [4] report that trauma is a trigger for the onset of MU, no matter of the stage. Indeed, we believe that pterygium surgery could be a triggering factor in exposing the corneal antibodies during the excision of the pterygium head. These fragilized antibodies would be more vulnerable to aggression of the conjunctival antigens in the adjacent area to the excised pterygium. Thus the trauma by inducing an immunological conflict seems to be a promoting factor with out being the cause of the ulcer since no antecedent was found in 69.23% of the patients.
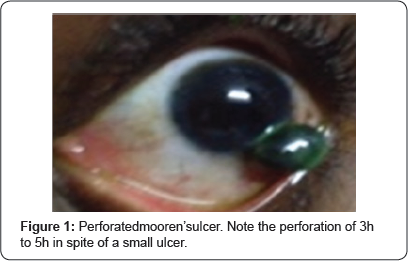
In this study, we reported 69.23% cases of blindness secondary to MU at the perforation stage; this emphasized once again that severe stage of MU had a major impact on visual acuity. This high blindness rate could also bein relationship with the long delay of consultation mentioned above, which exceeds three months in the majority of cases (61.54% of the eyes) and the subsequent delay in treatment. The analysis of ulcer associated with corneal perforation shows that this perforation area is always smaller than the ulcer area. Perforation usually occurs in the central zone of the ulcer, which seems to be the first area where the ulcer would have begun before its perilimbic circumferential extension. This central area is early destroyed in depth at the origin of the perforation. This analysis of the extent reveals that this pathology in our tropics tends to go faster in depth than in periphery (Figure 1). Indeed no total peripheral involvement of 360 degrees was observed, unlike Srinivasan in India, which found 15% of total peripheral ulceration [6]. This rapid evolution in depth is very threatening for the prognosis because very often leading to evisceration. The treatment of MU is difficult and long. It sometimes requires the combination of several therapeutic approaches and must be adapted to the clinical response. At the stage of perforation, the treatment is resolutely surgical associated with a medical therapy made of corticosteroids and / or immuno suppressive drugs.
The use of local and general corticosteroids is justified by the accessibility of these molecules in our regions and also by the recovery of some cases of less aggressive MU by means of cortico therapy which constitutes the first line treatment of the pathology. The broad use of immuno suppress ants in the patient’s management in our study is due to the aggressive nature of this disease in black people. Indeed this molecule has proved effectiveness in melano derms but its its systemically use is at the origin of important side effects. Nevertheless, this immuno suppressive treatment in the context of a perforated ulcer must be systematically associated with a surgical treatment Figure 2, the only one able to restore the anatomical integrity of the eye ball. In fact, the immuno suppress ant or corticosteroids treatment brings healing of the ulcer but have no influence on the corneal perforation as well as hernia of iris. Conjunctival resection and its low cost are justifiable reasons which make this technique a therapeutic approach of choice in the treatment of MU [8]. Easy access of this surgical technique keeps promoting this procedure in the management of MU in Cote d’Ivoire. It has the advantage of being able to be carried out without an operating microscope. Moreover, this technique has a therapeutic advantage and allows a histological diagnosis of the resected conjunctiva.
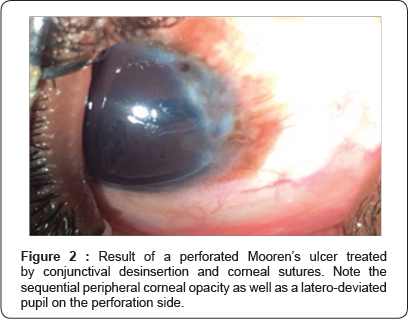
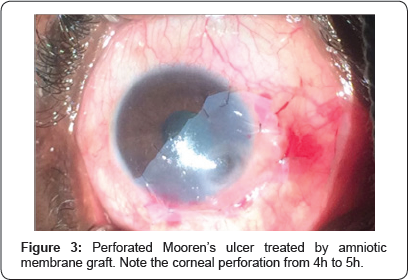
The corneal sutures after iris viable reintegration is often difficult to achieve in case of significant substance loss of the cornea. It is almost made under tension and is performed with separate simple corneo-limbic or corneo-scleral points. Only three cases (23.08%) in this study received human amniotic membrane graft (Figure 3). Amniotic membrane grafting is a recent therapeutic approach in the management of MU. This idea comes from the good results seen in treatment with amniotic membrane transplantation in corneal ulceration due to other causes.Its interest in the treatment of MU at the perforation stage is two fold: anatomical in order to compensate the loss of substance and by creating an immunosuppressive environment conducive to wound healing [9]. After medico- surgical treatment, a stationary acuity was noted in 38.46% of the cases. This stationary visual acuity could be judged un satisfactory after the treatment performed during this study. But the target of treating a perforated MU is the preservation of the anatomical integrity of the eyeball in order to avoid spontaneous evisceration Complications may occur during the evolution of a perforated MU. We noted two cases of cataract and one case of uveitis in respectively 15.4% and 7.7% of cases. As for Chen [5] in China, he found these two complications at respective rates of 6.8% and 2.3%. Cataract is frequent during this pathology especially at the stage of perforation. The treatment of this cataract is difficult and must be done best by phacoemulsification or by the technique of «small incision cataract surgery». Indeed, Srinivasan [6] points out that the limbic incision in manual extracapsular cataract surgery would be a real risk factor for progression and even recurrence. The scleral incision would have the double advantage of moving the incision site away from the limbus, which is the inflammatory location of origin of this ulceration, and not to unmask the target corneal antigens.
Recurrences after healing are frequen tduring MU. We report 30.77% of recurrences in this study, this result is close to the results observed in Chen's study [5] in China which reported 25.6% of recurrences. This pathology is readily recurrent as described in the literature. This appears to be due to the fact that there are unknown etiologies of the MU and the most likely cause of this disease would be an immunological conflict. This recurrence is frequently encountered during these so-called «idiopathic» pathologies. The patient should be informed of the functional symptomatology of the recurrence in order to consult as soon as possible. The analysis of the risks factors of recurrence of this pathology shows that any young melanoderm patient under 30 years of age, female and who would have a late consultation of more than 3 months would have more risk of recurrence of perforation secondary to MU. In these cases, amniotic graft would have better results in terms of visual function as well as a safety factor to avoid a possible recurrence.
Conclusion
MU at the stage of perforation is a rare but redoubt able pathology and seriously threatening for the organic and visual prognosis. It is more aggressive in melano derm young people. The medical and surgical treatment has maintained the integrity of the eye ball. The functional prognosis due to the corneal opacities is far to be satisfactory. Keratoplasty could improve this functional prognosis in cases of perforated MU in black African people.
References
- Mooren A (1867) Ophthalmiatrish Beobachtungen A Hirschwald Berlin 1867: 107-110.
- Bowman W (1849) The parts concerned in the operation of the eye. Case 12: 112.
- Tuft S (2003) Mooren'sulcer. In: Johnson GJ, Minassian DC, Weale RA, West SK (Eds.), Epidemiology of eye disease. London. Arnold 209-211.
- Fasina O, Ogundipe AO, Ezichi EI (2013) Moren'sulcer in Ibadan Southwest Nigeria. J West Afr Coll Surg 3: 102-19.
- Chen J, Hanping X (2000) Mooren's ulcer in China: A study of clinical characteristics and treatement. Br J Ophthalmol 84(11): 1244-9
- Srinivasan M, Michael EZ (2007) Clinical characteristics of Mooren's Ulcer in South India. Br J Ophthalmol 91(5): 570-575.
- Zhao JC, Xiu Ying J (1993) Immunological analysis and treatement of Mooren's ulcer with cyclosporin A applied topically. Cornea 12(6): 481488.
- Lambiase A, Sacchetti M, Sgrulletta R (2005) Amniotic membrane transplantation associated with conjonctivalperitomy in the management of Mooren's ulcer: a case report. eur J Ophthalmol 15(2): 274-276.
- Naacke H, Borderie V (2000) Perforation corneenne marginale liee a herpes virus simplex chez un patient atteint de porphyrie cutanee essentielle. J Fr Ophtalmol 23(7) : 699
- Lewallen S, Courtright P (1990) Problems with current concepts of the epidemiology of Mooren'scorneal ulcer. Ann ophthalmol 22(2): 52-55.






























