Simultaneous Macular Corneal Dystrophy and Keratoconus
Mohammed A Abu ameerh*, Ahmed NS Zewar and Muawyah D Al-Bdour
Department of ophthalmology, University of Jordan, Jordan
Submission: June 18, 2017; Published: September 25, 2017
*Corresponding author: Mohammed AAA, The University of Jordan, Amman 11942 Jordan. Tel: 00962 -799060613; Fax: 009626-5353399; Email: Mohammd_73@yahoo.com
How to cite this article: Mohammed AAA, Ahmed N Z, Muawyah D A B. Simultaneous Macular Corneal Dystrophy and Keratoconus. JOJ Ophthal. 2017; 5(2): 555656. DOI: 10.19080/JOJO.2017.05.555656.
Abstract
Purpose: To investigate the relationship between simultaneous occurrence of Macular corneal dystrophy and Keratoconus.
Methods: A 19-year-old patient presented with bilateral decreased vision of 4 years' duration. Ophthalmic examination revealed a visual acuity of 0.3 and 0.4 in right and left eyes respectively and bilateral corneal deposits indicative of macular corneal dystrophy. Topographic imaging was suspicious of keratoconus and left penetrating keratoplasty was performed.
Results: Topathologic examination of the corneal button confirmed the combined presence of keratoconus and macular dystrophy. To the best of our knowledge, very few reports in the literature described this co-existence. More elaborative studies are needed to detect possible relation between these two entities.
Keywords: Keratoconus; Macular Corneal Dystrophy; Penetrating Keratoplasty
Introduction
Keratoconus (KC) is a non-inflammatory corneal ectatic disorder characterized by progressive steepening and stromal thinning leading to irregular astigmatism and poor vision; the hereditary pattern is unpredictable [1]. Corneal dystrophies are inherited, bilateral and slow lyprogressive diseases [2]. Macular corneal dystrophy (MCD) is the least common and the most severe [3,4], however, increasing rates have been noticed in the Arabian Peninsula [5]. There are few observations of the simultaneous occurrence of Macular corneal dystrophy (MCD) and Keratoconus (KC) in the literature [1,6-9]. It is not fully understood whether this association is due to a common pathogenetic mechanism or adjacent genetic defects.
Case Report
A 19-year-old female patient presented with progressive blurring of vision bilaterally, left eye more than the right, for the past 4 years; no more visual improvement with changing glasses and contact lenses. No history of ocular allergies, surgeries, traumas, or any systemic illness or medication. Family history was negative for Keratoconus (KC) or corneal dystrophies. A degree of consanguinity was evident between parents.
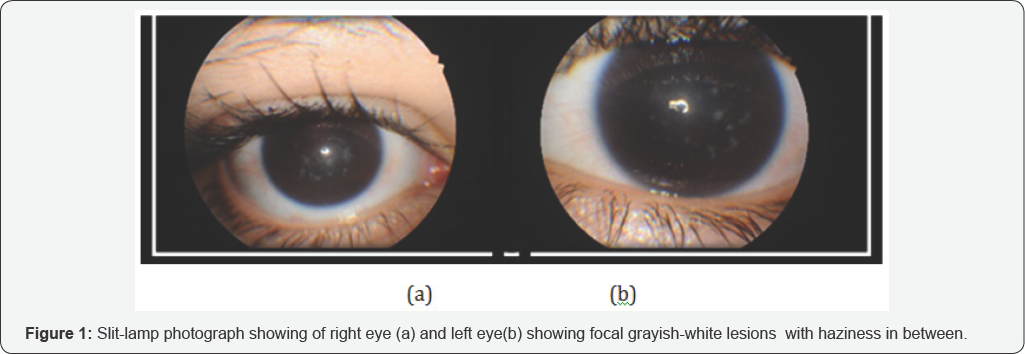
Right eye uncorrected visual acuity was 0.3 improving to 0.4 with plano /-6.00 @180 and 0.3 in the left eye not improving with refraction up to -1.50D/-7.50 @180. Retinoscopy reflex was not clear. Diffuse slit lamp examination revealed multiple focal ill-defined gray-white corneal opacities, more centrally than peripherally with diffuse interceding cloudiness (Figure 1). Optical section illumination showed peripheral superficial and central deeper stromal location of the opacities. Both eyes showed mild inferior paracentral thinning, but no vogt's stirae or Fliescher ring. The rest of the anterior and posterior segments were normal. No signs of similar pathology in her relatives.
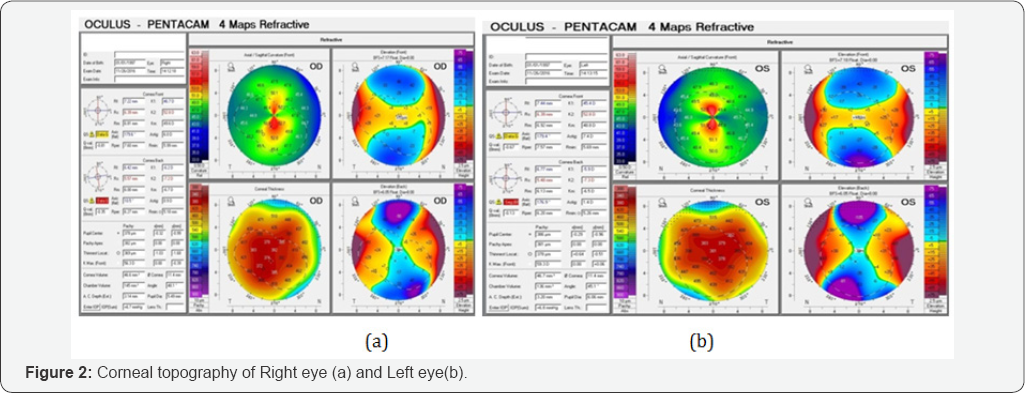
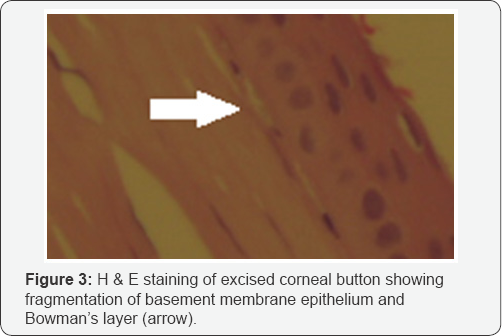
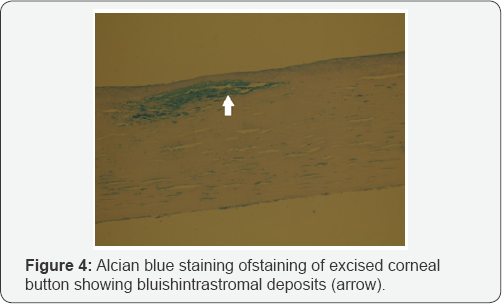
Corneal topography (Pentacam, Oculus OptikgerSte GmbH, Wetzlar, Germany) was done which revealed a suspected pattern of Keratoconus (KC) (Figure 2). Clinical diagnosis of bilateral Macular corneal dystrophy (MCD) with a clinical and topographical suspicion of KC was made and the patient underwent an uneventful left eye penetrating keratoplasty (PKP). The histopathology report of the corneal button indicated stromal multiple deposits, stained positively with both Alcian blue and Colloidal Iron, distinctive for Macular corneal dystrophy (MCD). Typical features of KC were also seen, focal disruption of the epithelial basement membrane with Bowman’s layer breaks and destruction (Figures 3 & 4).

Discussion
Macular corneal dystrophy (MCD) usually starts early in life with lesions develop initially in the superficial stroma then extend peripherally and deeply with indistinct borders and hazy intervening spaces. They are composed of glycosaminoglycans that stain with Alcian blue and colloidal iron. Keratoconus has a multifactorial etiology with involvement of more than one gene loci in addition to environmental factors (Figure 5). His topathologic changes include focal disruptions of the basement membrane and Bowman’s layer, central stromal thinning, folding or rupture of Descemet’s membrane and a variable amount of scarring [1,6]. The phenocopy of corneal astigmatism and corneal thinning is similar between Keratoconus and Macular corneal dystrophy. MCD is an autosomal recessive dystrophy with an identified genetic cause, however, the genetic contribution in (KC) development is not known [10]. The incidence of combined Keratoconus and other dystrophies may be higher than what is documented in literature because mild Keratoconus can be missed on a routine examination [1].
Although corneal thinning was documented in Macular corneal dystrophy (MCD) [10], most patients do not show corneal ectasia [7]. The causes of Keratoconus and MCDco- occurrence remain unknown but may include a molecular mechanism, genetic linkage or mere chance. Javadi et al. [6] pointed to the biochemical similarities between Keratoconus and Macular corneal dystrophy (MCD) and hypothesized that Macular corneal dystrophy (MCD) deposits cause biochemical alteration in collagen fibrils leading to thinning and ectasia [6]. Kosrirukvongs et al. [9] found that KC may develop secondary to macular dystrophy changes [10]. Alternately, this association may be caused by a single genetic modification (Figure 6). Chromosome 16q22 mutations can cause MCD, this locus contains a carbohydrate sulfotransferase gene (CHST6) which, interestingly, also present in one of the linked loci for KC (16q22.3-q23.1) [1,10].

Dudacova et al found topographical and his topathologic evidence of diffuse corneal thinning in eyes with Macular corneal dystrophy (MCD) but no clear Keratoconus features on topography especially on the posterior surface. They concluded that localized anterior curvature elevation can occur in MCD in the absence of other defining Keratoconus criteria. Therefore the sole dependence on anterior corneal maps in these cases can give false indices of Keratoconus, due to the effect of stromal deposits on capture quality, and so correlation with posterior corneal elevation maps and regional pachymetry is required. They suggest that the change in anterior corneal curvature and diffuse corneal thinning is a phenocopy of the changes that occur in KC [10]. Balestrazzi et al. [8] reported a rare case of Macular corneal dystrophy (MCD) in association with Keratoconus diagnosed histopathologically and by using confocal microscopy [8]. Our patient showed the typical clinical appearance of Macular corneal dystrophy (MCD), but absent classical KC signs and in conclusive topography; however, the histopathologic findings confirmed the associated presence of both diseases. The indefinite Keratoconus diagnosis can be explained by the advanced concomitant [2]. Macular corneal dystrophy (MCD) stage. Our case signifies the importance of excluding Keratoconus in cases of corneal dystrophy, as PTK cannot be performed in these cases due to corneal thinning leading to risk of ectasia progression [9-11]. Furthermore, we should consider Keratoconus as possible cause for visual deterioration unexplained by the amount of corneal stromal deposits and haze [7]. As KC can be the main or an additive reason for the decreased vision and can be treated with contact lenses so keratoplasty can be avoided or delayed [9].
Simultaneous appearance of Keratoconus and Macular corneal dystrophy (MCD) can occur even though it is rare, so further studies are needed regarding the possible genetic, histopathologic, pathophysiologic, and biochemical linkages. More comprehensive examination, sophisticated investigations and diagnostic criteria are required to detect Keratoconus in the presence of concurrent corneal dystrophies and so deciding the best appropriate management plan.
References
- Mohammad-Rabei H, Shojaei A, Aslani M (2012) Concurrent macular corneal dystrophy and keratoconus. Middle East Afr J Ophthalmol 19(2): 251-253.
- Wilson CM, D'Ath PJ, Parmar DN, Sykatis E (2014) Keratoconus and granular dystrophy. BMJ Case Rep 25. pii: bcr2014205584.
- Kenyon KR, Hersh PS, Starck T, Fogle JA (1998) Chapters 16,19, 20, 35/ Corneal dysgeneses, dystrophies, and degenerations. In: Tasman W, Jaeger EA (Eds), Duane's Clinical Ophthalmology 4. Philadelphia: Lippincott Williams & Wilkins, USA.
- Krachmer JH, Mannis MJ, Holland EJ (1997) Cornea and External Disease. Clinical Diagnosis and Management 2: 1045-1046, 10911093.
- Al-Faran MF, Tabbara KF (1991) Corneal dystrophies among patients undergoing keratoplasty in Saudi Arabia. Cornea 10(1):13-16.
- Javadi MA, Rafeéi AB, Kamalian N, Karimian F, Jáfarinasab MR, et al. (2004) Concomitant keratoconus and macular corneal dystrophy. Cornea 23(5): 508-512.
- Al-Hamdan G, Al-Mutairi S, Al-Adwani E, Al-Mujaini A (2009) Bilateral coexistence of keratoconus and macular corneal dystrophy. Oman J Ophthalmol 2(2): 79-81.
- Balestrazzi A, Martone G, Traversi C, Haka G, Toti P, et al. (2006) Keratoconus associated with corneal macular dystrophy: in vivo confocal microscopic evaluation. Eur J Ophthalmol 16(5): 745-750.
- Kosrirukvongs P, Ngowyutagon P, Booranapong W (2016) Keratoconus in Patients with Macular Stromal Dystrophy. J Med Assoc Thai 99(1): 65-70.
- Dudacova L, Palos M, Svobodova M, et al (2014) Macular corneal dystrophy and associated corneal thinning. Eye 28(10): 1201-1205.
- Rathi VM, Vemuganti GK, Sangwan VS, Jannabiran C (2011) Late occurrence of granular dystrophy in bilateral keratoconus: Penetrating keratoplasty and long-term follow-up. Indian journal of ophthalmology 59(5): 398-400.






























