Diabetes Screening in Rural Appalachian Population by Ocular Scatter Measurement
George Asimellis*
University of Pikeville, USA
Submission: August 02, 2017; Published: September 15, 2017
*Corresponding author: George Asimellis, Associate Professor, Kentucky College of Optometry, University of Pikeville, 147 Sycamore Street, Pikeville, KY 41501, USA, Tel: 606 218 5521,606 205 3623; Email: georgeasimellis@gmail.com; georgeasimellis@upike.edu
How to cite this article: George A. Diabetes Screening in Rural Appalachian Population by Ocular Scatter Measurement. 2017; 4(4): 555645. DOI: 10.19080/JOJO.2017.04.555645.
Abstract
Optically-based, in-vivo measurement of forward ocular scatter in the underserved population of rural Appalachia may serve the purpose of early detection and understanding of diabetes mellitus prevalence in the area. Diabetes is a condition that affects millions of people in the United States, and a leading cause of blindness in Central Appalachia [1]. This review aims to help identify the prevalence of youth diabetes in Eastern Kentucky / Rural Appalachia, and increase awareness to those at risk in order to receive health care treatment in a timely fashion.
Keywords: Diabetes; Ocular scatter; Double pass aberrometry
Abbreviations: SVL: Severe Vision Loss; PSF: Point Spread Function; CDC: Disease Control and Prevention; WHO: World Health Organization
Introduction
Diabetes is a clinical syndrome characterized by a disorder in the metabolism of carbohydrates, caused by a defect in insulin secretion, insulin action, or both. Chronic hyperglycemia affects critically not only the eye, whose prime effect is diabetic retinopathy, but also a number of organs, such as the kidneys, nerves, heart, and blood vessels [2,3]. Worldwide, diabetes has a significant impact due to its increased prevalence and high mortality rate. A prospective study shows that in developed countries there will be an 11% increase in the adult population, a 27% increase in the prevalence of adult diabetes, and a 42% increase in the number of people with diabetes, while for developing countries there will be an 82% increase in the adult population, a 48% increase in the prevalence of adult diabetes, and a 170% increase in the number of people with diabetes, between the years 1995 and 2025 [4]. According to the World Health Organization (WHO), by 2030 diabetes-affected people may reach 366 million world-wide, the International Diabetes Federation states that the prevalence of diabetes will be 10% and the number of people with diabetes will rise to 552 million people by 2030 [5,6].
Ocular complications of diabetes
Diabetes is associated with several complications within the eye, such as cataract [7-9], (up to 4*more than healthy people), glaucoma [10,11], keratopathy [12], refractive changes, oculo motor nerve paralysis, chronic inflammation of the eyelids, and diabetic retinopathy [13]. From an optical perspective, the structures directly involved in the refractive function of the eye that, when affected, deteriorate its optical quality are the tear film, the cornea, the crystalline lens, and the vitreous. It is noteworthy that of these structures are affected by diabetes. From a signal-sensation perspective, the structure directly involved in the detection of the retinal image is the retina, which is also affected by diabetes, via swelling of the retina blood vessels.
Optical quality in people with diabetes
Diabetes has important effects on every corneal substructure. There are significant and characteristic clinical signs, generally described as diabetic keratopathy. They are manifest in the majority (>70%) of diabetes affected individuals, and they affect morphological, metabolic, physiological, and the clinical function of the cornea [14]. Clinical signs include epithelial defects, recurrent epithelial erosions, delayed reepithelization, slower wound repair, increased epithelial fragility, reduced sensitivity, increased auto fluorescence, altered epithelial and endothelial barrier functions, ulcers, edema, and increased susceptibility to injury [15-17].
Affected individuals often report discomfort in certain activities, such as reading or driving, and blurred vision with their prescribed spectacle correction. This is because the refractive state of the eye is subject to frequent and intermittent variations and can be either acute or long lasting. Among the long lasting effects is the development or progression of myopia as a result of hyperglycemia [18], while relative hypoglycemia with respect to initial hyperglycemia state may lead to hyperopic shift. The main body affected by fluctuations in hyper- or hypoglycemia, by both short-term fluctuations and long terms shifts is the crystalline lens. This is also the refractive element that depends on excellent transparency. These fluctuations affect the clarity of the crystalline lens, and can affect the retinal image optically via forward scatter [19].
In affected individuals, a rapid reduction in blood glucose could cause an aggravation of both retinopathy status and refractive changes, so that visual acuity often decreases. In short, both the optical quality of the formed retinal image, as well as its perception by the retinal layer is affected by diabetes.
Ocular scattering
The objective assessment of the optical quality of the eye is of great interest in clinical practice. While visual acuity and contrast sensitivity are often used clinically to establish the optical quality, diffraction, aberrations, and scattering influence intraocular retinal image quality, therefore affecting its visual performance. The visual acuity and contrast sensitivity tests often do not include the effects of high-order aberrations and ocular scattering. In a normal healthy eye, each optical component may cause some scattering; this includes both refractive elements of the eye (cornea and lens), the media in which they are immersed (vitreous and aqueous), and the supporting structures (sclera and iris). Intraocular scattering increases with age [20,21], pigmentation, associated diseases, or ocular surgery. In an eye affected by diabetes, even in its early form, it is expected the contributions of the disease on the ocular structures increases forward scatter in the eye.
Early diagnosis of diabetes
Inasmuch in most diseases, early diagnosis and treatment are essential in a successful management of diabetes. Traditionally, the diagnosis is based on measurement of A1C levels, fasting or random blood glucose level, or oral glucose tolerance testing. These tests are considered time-consuming, not cost- effective and invasive. An alternative early diagnosis test may be offered by a purely optical, non invasive, and almost instant ocular examination. This relates to the measurement of ocular scatter. New optical technologies clinically available today offer a fast, objective, and non-invasive method for assessing the contribution of aberrations and ocular scattering to the optical quality of the retinal image. The examination is fast and simple, and can provide and establish normative baseline values for normal subjects, which can then be compared with people with diabetes. Due to the high prevalence of diabetes in our underserved area, determination of optical quality in diabetic eyes could be a useful complementary test for screening and monitoring of the condition.
Instrumentation
The technique that allows the objective measurement of scattered light on the retina is based on the double-pass principle [22,23]. In this method, a collimated beam (and, thus, plane wave front) of coherent infrared radiation is focused through the optics of the eye on the retina. This focused light serves as a secondary source of radiation that propagates in all directions, and thus a part of it propagates to the exit of the eye by passing through the optical media of the eye twice. It is practically similar to the principle of Tscherning Aberrometry.
The difference between the two techniques is that, while aberrometry typically aims to visualize the different focal positions of focused points (point spread function, PSF) over a grid, double-pass aberrometry aims to study not the location but the exact three-dimensional distribution of the PSF functions corresponding to the wave front that transcends the eye [24]. The measurement is based on comparing the white noise associated with the distribution: the PSF scattering sums in 'simple' PSF function over a continuous pedestal background, which can be associated with the scattered retinal light. This is implemented by the HD Analyzer/ Optical Quality Analysis System (OQAS, Visiometrics, Terrassa, Spain).
Outreach Potential
Located in Central Appalachia, the Kentucky College of Optometry (KYCO) serves an area that suffers from health disparities caused, in part, to a lack of healthcare resources [25]. According to the Centers for Disease Control and Prevention (CDC) [26], the region has the nation's highest incidence of severe vision loss from other factors. The CDC also includes the area in the nation’s so-called "diabetes belt" due to the prevalence of type 2 diabetes [27]. Early detection and timely treatment are critical to maintaining eye health and preventing or delaying vision impairment, defined as the best-corrected visual acuity <20/40 in the better-seeing eye [28]. Nearly 38 million persons in the United States have common eye diseases such as glaucoma, diabetic retinopathy, age-related macular degeneration, and cataracts [29]. Medical costs rise with increased duration of the disease, and lifespan is shortened by 5 to 10 years in most

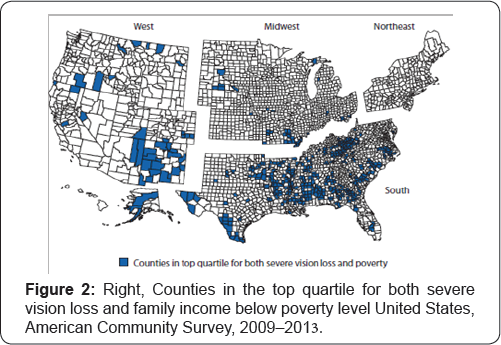
Prevention of diabetes and diabetes-related complications through treatment and disease self-management is paramount in changing this deadly and costly course and demands continued innovation in health programs and services and new partnerships among health professionals. Diabetic patients can benefit from early detection, since effective intervention is available [30] (Figure 1 & 2). In addition, distinct geographic patterns of severe vision loss (SVL) prevalence were found in the United States, 77.3% of counties in the top SVL prevalence quartile (>4.2%) were located in the South [31]. SVL was significantly correlated with poverty (r = 0.5), 437 counties were in the top quartiles for both SVL and poverty, and 83.1% of those counties were located in southern states [32]. Currently, ophthalmic complications from diabetes are not adequately screened, especially within the primary care setting, and further quality improvement measures may improve adherence to recommended screening protocols [33].
However, there are limited data and research databases at local levels, where interventions and policy decisions to reduce the burden of vision loss and eliminate disparities are often developed and implemented [34]. A search in the peer- review literature reveals only four publications that studied the prevalence of diabetes in the following Southern States: South Carolina, North Carolina, Alabama, and West Virginiab [3538]. A factor that presents additional challenges to addressing the increasing problem of the prevalence of diabetes in rural Appalachia is in differences in perceived healthy lifestyle habits and a general acceptance of a higher average body weight [39]. Factors contributing to this is the relative isolation of many of these communities.
References
- Munoz B, West SK (2002) Blindness and visual impairment in the Americas and the Caribbean. Br J Ophthalmol 86(5): 498-504.
- (2005) American Diabetes Association. Diagnosis and classifications of diabetes mellitus. Diabetes Care 28(Suppl 1): S37-42.
- (2010) American Diabetes Association. Diagnosis and classifications of diabetes mellitus. Diabetes Care 33(Suppl 1): S62-69.
- King H, Aubert RE, Herman W (1998) Global burden of diabetes, 1995- 2025: prevalence, numerical estimates, and projections. Diabetes Care 21(9): 1414-1431.
- Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27(5): 1047-1053.
- Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF Diabetes Atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94(3): 311-321.
- Ederer F, Hiller R, Taylor HR (1981) Senile lens changes and diabetes in two population studies. Am J Ophthalmol 91(3): 381-395.
- Nielsen NV, Vinding T (1984) The prevalence of cataract in insulin- dependent and non-insulin-dependent-diabetes mellitus. Acta Ophthalmol (Copenh) 62(4): 595-602.
- Klein BE, Klein R, Moss RE (1985) Prevalence of cataracts in a population- based study of persons with diabetes mellitus. Ophthalmology 92(9): 1191-1196.
- Sahin A, Bayer A, Ozge G, Mumcuoglu T (2009) Corneal biomechanical changes in diabetes mellitus and their influence on intraocular pressure measurements. Invest Ophthalmol Vis Sci 50(10): 45974604.
- Perez RC, Gutierrez OC, Gonzalez MA, Zandueta AM, Moreno SA, et al. (2015) Effect of diabetes mellitus on Corvis ST measurement process. Acta Ophthalmol 93(3): e193-198.
- Inoue K, Kato S, Ohara C, Numaga J, Amano S, et al. (2001) Ocular and systemic factors relevant to diabetic keratoepitheliopathy. Cornea 20(8): 798-801.
- Williams R, Airey M, Baxter H, Forrester J, Kennedy MT, et al. (2004) Epidemiology of diabetic retinopathy and macular oedema: a systematic review. Eye (Lond) 18(10): 963-983.
- Quadrado MJ, Popper M, Morgado AM, Murta JN, Van Best JA (2006) Diabetes and corneal cell densities in humans by in vivo confocal microscopy. Cornea 5(7): 761-768.
- Shih KC, Lam KS, Tong L (2017) A systematic review on the impact of diabetes mellitus on the ocular surface. Nutr Diabetes 7(3): e251.
- Sanchez TJC (1998) The cornea in diabetes mellitus. Int Ophthalmol Clin 38(2): 19-36.
- Herse PR (1998) A review of manifestations of diabetes mellitus in the anterior eye and cornea. Am J Optom Physiol Opt 65(3): 224-230.
- Duke EWS (1925) Changes in refraction in diabetes mellitus. Br J Ophthalmol 9(4): 167-187.
- Gwinup G, Villareal A (1976) Relationship of serum glucose concentration to changes in refraction. Diabetes 25(1): 29-31.
- Applegate RA, Ballentine C, Gross H, Sarver EJ, Sarver CA (2003) Visual acuity as a function of Zernike mode and level or root mean square error. Optom Vis Sci 80(2): 97-105.
- Artal P, Ferro M, Miranda I, Navarro R (1993) Effects of aging in retinal image quality. J Opt Soc Am A 10(7): 1656-1662.
- Flamant F (1955) Etude de la repartition de lumiere dans l'image retinienne d'une fente. Rev Optique 34: 433-459.
- Artal P, Iglesias I, Lopez GN, Green DG (1995) Double-pass measurements of the retinal-image quality with unequal entrance and exit pupil sizes and the reversibility of the eye's optical system. J Opt Soc Am A Opt Image Sci Vis 12(10): 2358-2366.
- Santamari'a J, Artal P, Bescos J (1987) Determination of the point- spread function of human eyes using a hybrid optical-digital method. J Opt Soc Am A 4(6): 1109-1114.
- McGarvey EL, Leon VM, Killos LF, Guterbock T, Cohn WF (2011) Health disparities between Appalachian and non-Appalachian counties in Virginia USA. J Community Health 36(3): 348-56.
- Kirtland KA, Saaddine JB, Geiss LS, Thompson TJ, Cotch MF, et al. (2015) Geographic Disparity of Severe Vision Loss -United States, 2009-2013. Morbidity and Mortality Weekly Report (MMWR) 64(19): 513-517.
- https://www.cdc.gov/diabetes/pdfs/data/diabetesbelt.pdf
- (2012) CDC Enhancing public health surveillance of visual impairment and eye health in the United States. Atlanta, GA: US Department of Health and Human Services, CDC.
- National Eye Institute. Healthy Vision Month.
- Javitt JC, Aiello LP (1996) Cost-effectiveness of detecting and treating diabetic retinopathy. Ann Intern Med 124(1 Pt 2): 164-169.
- http://dataferrett.census.gov/TheDataWeb/index.html.
- Kirtland KA, Saaddine JB, Geiss LS, Thompson TJ, Cotch MF (2015) Geographic Disparity of Severe Vision Loss-United States, 2009-2013. Geographic Disparity of Severe Vision Loss-United States, 2009-2013. Morbidity Mortality Weekly Report / Center for Disease Control and Prevention 64(19): 513-517.
- Silva FQ, Adhi M, Wai KM, Olansky L, Lansang MC, et al. (2016) Evaluation and Referral of Diabetic Eye Disease in the Endocrinology and Primary Care Office Settings. Ophthalmic Surg Lasers Imaging Retina 47(10): 930-934.
- Zhang X, Cotch MF, Ryskulova A, Primo SA, Nair P, et al. (2011) Vision health disparities in the United States by race/ethnicity, education, and economic status: findings from two nationally representative surveys. Am J Ophthalmol 2012; 154(Suppl): 53-62.
- Heidari K, Myers PM (2013) Brief update on the burden of diabetes in South Carolina. Am J Med Sci 345(4): 302-316.
- Konen J, Page J (2011) The state of diabetes in North Carolina. NC Med J 72(5): 373-378.
- Cherrington A, Martin MY, Hayes M, Halanych JH, Wright MA, et al. (2012) Intervention mapping as a guide for the development of a diabetes peer support intervention in rural Alabama. Prev Chronic Dis 9: E36.
- Chopra I, Chopra A (2017) Risk perception for diabetes in Appalachian women. Women Health 57(5): 534-550.
- Williams KJ, Taylor CA, Wolf KN, Lawson RF, Crespo R (2008) Cultural perceptions of healthy weight in rural Appalachian youth. Rural Remote Health 8(2): 932.






























