Choroidal Osteoma with Neovascular Membrane Managed with Aflibercept and Yellow Laser
Raphael Pereira da Silva*, Leonardo Dias Alencar, Carlos Augusto Morería Júnior and Carlos Moreira-Neto
Department of Retina and Vitreous, Eye Hospital of Paraná, Brazil
Submission: August 13, 2017; Published: September 06, 2017
*Corresponding author: Raphael Pereira da Silva, Deaprtment of Retina and Vitreous, Eye Hospital of Paraná, Brazil, Tel: 55 (92) 98272-5596; |Email: raphael_ps6@hotmail.com
How to cite this article: Raphael P S, Leonardo D A, Carlos A M, Carlos M. Choroidal Osteoma with Neovascular Membrane Managed with Aflibercept and Yellow Laser. 2017; 4(4): 555641. DOI: 10.19080/JOJO.2017.04.555641.
Abstract
To present a case of neovascular membrane due to a choroidal osteoma successfully treated with aflibercept and yellow laser. A healthy 19-year-old man presented with a dark spot on temporal field of the left eye with one month of evolution. Examination of the ocular fundus of the left eye revealed a well-circumscribed and elevated orange-yellow plaque underneath the retina around the optic disc and subretinal hemorrhages in the macular region. The patient was submitted to fluorescein angiography, ocular ultrasound, optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA), then diagnosed with choroidal osteoma associated with neovascular membrane. He was treated with a series of 3 intravitreal aflibercept injections and submitted to yellow laser. One month after the procedure, visual acuity was 20/20 and the neovascular membrane had regressed.
Keywords: Anti-VEGF therapy; Choroidal neovascularization; Choroidal osteoma; Yellow laser therapy
Abbreviations: CO: Choroidal Osteoma; OCT: Optical Coherence Tomography; OCTA: Optical Coherence Tomography Angiography; CNV: Choroidal NeoVascularization; Anti-VEGF: Anti-Vascular Endothelial Growth Fator; OCT-EDI: Optical Coherence Tomography-Enhenced Depth Imaging; AMD: Age-related Macular Disease; RPE: Retinal Pigment Epithelium; FFA: Fundus Fluorescent Angiography; SD-OCT: Spectral Domain Optical Coherence Tomography; PDT: Photo Dynamic Therapy
Introduction
Choroidal osteoma (CO) is a benign and rare tumor that is composed by mature bone cells and is more prevalent in females in the second decade of life [1]. CO is often located in juxtapapillary or macular region and is unilateral in the most of cases [2]. The most common complication of CO is choroidal neovascularization (CNV) occurring in up to 31% of cases [3]. CNV is an important cause of visual loss in patients with CO. Decalcification and serous retina detachment can be other causes of visual impairment due this tumor [4]. OCT plays fundamental role in the diagnosis and follow up of a large amount of retinal and choroidal diseases, including CNV. It has been used to evaluate singular characteristics of choroidal tumors throughoptical coherence tomography enhenced depth imaging (OCT-EDI) [5] and vascular abnormalities by the OCT- angiography (OCTA) [6].
The intravitreous injection of anti-vascular endothelial growth factor (anti-VEGF) is an effective treatment for CNV, mainly when it is subfoveal [7]. Aflibercept, a new anti-VEGF agent, has shown efficacy to those patients who are nonresponders to ranibizumab and bevacizumab in CNV associated with age-related macular disease (AMD) [8]. Similarly, the laser therapy using the yellow laser (577nm) reduces the damage of surrounding retina and of retinal pigment epithelium (RPE) cells [9], allowing a safer treatment of CNV in the macula, except in the fovea region. Herein, we report a case of a patient with COassociated CNV documented by OCTA and successfully treated by intravitreous aflibercept injections and yellow laser therapy.
Case Report
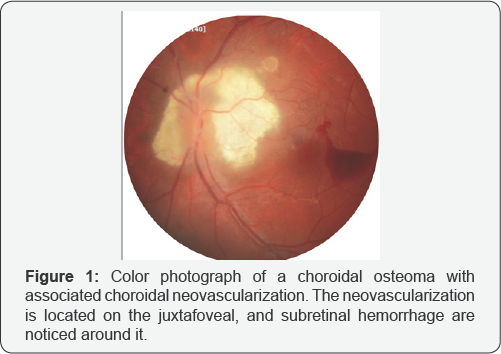
A 19-year-old caucasian male presented with a dark spot on temporal field of the left eye with one month of evolution. There was no other relevant past ocular, medical or family history. His best corrected visual acuity was 20/20 in the right eye and 20/20 in the left eye. His anterior segment examination was unremarkable, as well as ocular fundus examinationof of the right eye. Fundoscopy ofthe left eye revealed a well-circumscribed and elevated orange-yellow plaque deep to the retina, peripapillary choroidal osteoma and subretinal hemorrhages in the macular region (Figure 1).
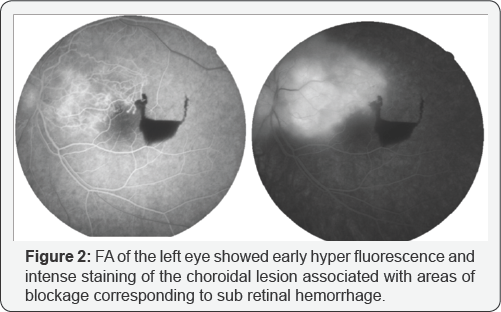
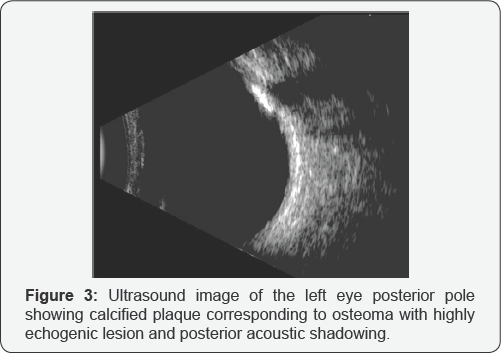
Color fundus photography, B-scan ultrasound, fundus fluorescent angiography (FFA), spectral domain optical coherence tomography (SD-OCT) (Heidelberg Engineering, Heidelberg, Germany) and optical coherence tomography angiography (OCTA) (Optovue, Inc., Fremont, CA, USA) were performed. FFA of the left eye showed early hyperfluorescence and intense staining of the choroidal lesion associated with areas of blockage corresponding to subretinal hemorrhage (Figure 2). The B-scan ultrasonography revealed a highly echogenic lesion with posterior acoustic shadowing (Figure 3).
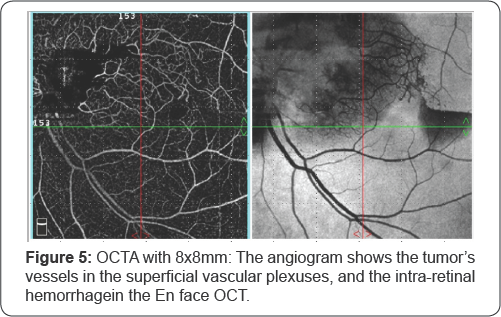
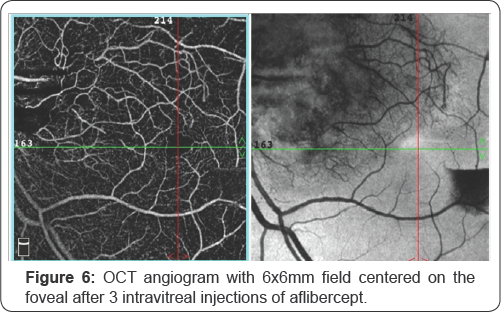
In the SD-OCT the osteoma was a well defined choroidal lesion with a sponge-like appearance because of the presence of multiple hyperreflective dots scattered among a hyporeflective mass (Figure 4). The angiogram shows the tumor's vessels in the superficial vascular plexuses, and the intra-retinal hemorrhage in the En face OCT. The osteoma showed no flow in the choriocapillaris layer (Figure 5). The diagnosis of CO complicated by CNV was confirmed, which was responsible for the intra-retinal hemorrhage. The patient underwent three consecutive monthly intravitreal injections of aflibercept (2.0mg). One month after all intravitreal aflibercept injections, OCTA showed that abnormal vascular signal was absent in the outer retina and choriocapillaris layers (Figure 6).

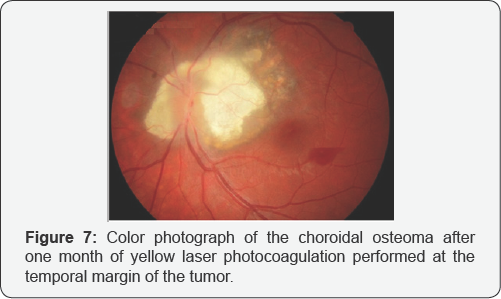
In addition, yellow laser photocoagulation was performed at the temporal margin of the tumor in order to avoid membrane recurrence (Figure 7). The final visual acuity of the patient was 20/20 and there was improvement of visual field defect in the left eye after two months of treatment.
Discussion
CNV occurs within 10 years in 31-47% of patients affected by CO and progressive vision loss marks the natural history of choroidal osteoma [10]. Several therapies have been proposed, such as laser photocoagulation, transpupillary thermal therapy, photodynamic therapy (PDT) and surgical excision, but none of them has proven effective in controlling CNV activity, as well as in improving visual acuity. Moreover, when CNV is located beneath the fovea, PDT should be avoided since decalcification of CO could result in worsening of visual acuity, impairment of both retinal pigment epithelium and choroidal perfusion can lead to a further impairment of visual function.
Photodynamic therapy has also been used as a treatment modality for CNV in patients with choroidal osteoma, based upon previous experience with PDT in exudative AMD [10]. The introduction of intravitreal anti-VEGF therapy has revolutionized the treatment of CNV secondary to age-related macular degeneration and other conditions. Several case series have described encouraging results with the use of ranibizumab or bevacizumab for CO-related CNV with an improvement of both retinal structure and visual acuity [11]. The favorable visual outcome following bevacizumab or ranibizumab injections is credited to the decrease in VEGF which, even at physiologic levels, might reduce the permeability of choroidal vessels. It has also been estimated that VEGF is up regulated secondary to chronic inflammation and mild ischemia caused by the choroidal tumor. Also the good results may be attributed to better drug availability through improved penetration of a thinned and degenerated RPE.
The patient did not present decalcification or serous retina detachment caused by the tumor. Aflibercept is a humanized fusion protein, approved in November 2011 by the Food and Drug Administration for the treatment of neovascular AMD. Differently than ranibizumab and bevacizumab, which bind selectively VEGF-A only, aflibercept targets VEGF-B, and placental growth fator (PGF) aswell.These properties leadto superior affinity for VEGF, compared to ranibizumab and bevacizumab. Moreover, the biologic qualities of aflibercept make this molecule potentially more efficient in the long-term control of neovascular activity, allowing less frequent re-injections, as supported by clinical trials [11].
In this case report, the patient was submitted to three consecutive monthly intravitreal injections of aflibercept (2.0mg). Analysis of magnified EDI-OCT images reveals a typical sponge-like pattern comprised of dense hyperreflective dots spread into hyporeflective matrix and a multilayer structure, likely because of the presence of different degrees of calcification within the tumor. It is believed that SD-OCT scan in eyes with an amelanotic lesion in the fundus can facilitate clinicians in differentiating choroidal osteomasfrom other conditions, such as sclerochoroidal calcifications, choroidal melanomas, choroidal metastasis and choroidal lymphoma [12].
The OCTA has the advantage of varying the segmentation and scrolling through the different retinal layers, and layer-specific observation of blood flow in each layer. In addition, OCTA can measure the vessel area change of CNV and provide a better appreciation of CNV, observing the efficacy more elaboratively and quantifiable. OCTA makes promising non-invasive identification of the CO-related CNV. OCTA was implemented to differentiate tumor's vessels from choroidal neovascularization [13].
References
- Gass JDM, Guerry RK, Jack RL, Harris G (1978) Choroidal osteoma. Arch Ophthalmol 96(3): 428-435.
- Aylward GW, Chang TS, Pautler SE, Gass JDM (1998) A long-term follow- up of choroidal osteoma. Arch Ophthalmol 116(10): 1337-1341.
- Shields CL, Sun H, Demirci H, Shields JA (2005) Factors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes with choroidal osteoma. Arch Ophthalmol 123(12): 1658-1666.
- Shields CL, Perez B, Materin MA, Mehta S, Shields JA (2007) Optical coherence tomography of choroidal osteoma in 22 cases: evidence for photoreceptor atrophy over the decalcified portion of the tumor. Ophthalmology 114(12): e53-e58.
- Mello PCD, Berensztejn P, Brasil OFM (2016) Enhanced depth imaging optical coherence tomography of choroidal osteoma with secondary neovascular membranes: report of two cases. Arq Bras Oftalmol 79(3): 197-199.
- Alameddine R M, Mansour AM, Kahtani E (2014) Review of choroidal osteomas. Middle East Afr J Ophthalmol 21(3): 244-250.
- Mansour AM, Arevalo JF, Al Kahtani E, Zegarra H, Abboud E, et al. (2014) Role of intravitreal antivascular endothelial growth factor injections for choroidal neovascularization due to choroidal osteoma. J Ophthal.
- Kumar N, Marsiglia M, Mrejen S, Fung ATC, Slakter J, et al. (2013) Visual and anatomical outcomes of intravitreal aflibercept in eyes with persistent subfoveal fluid despite previous treatments with ranibizumab in patients with neovascular age-related macular degeneration. Retina 33(8): 1605-1612.
- Yadav NK, Jayadev C, Rajendran A, Nagpal M (2014) Recent developments in retinal lasers and delivery systems. Indian J Ophthalmol 62(1): 50-54.
- Parodi MB, Da Pozzo S, Toto L, Saviano S, Ravalico G (2001) Photodynamic therapy for choroidal neovascularization associated with choroidal osteoma. Retina 21(6): 660-661.
- Khan MA, DeCroos FC, Storey PP, Shields JA, Garg SJ, et al. (2014) outcomes of anti-vascular endothelial growth factor therapy in the management of choroidal neovascularization associated with choroidal osteoma. Retina 34(9): 1750-1756.
- Pellegrini M, Invernizzi A, Giani A, Staurenghi G (2014) Enhanced depth imaging optical coherence tomography features of choroidal osteoma. Retina 34(5): 958-963.
- Xuan Y, Zhang Y, Wang M, Guo J, Li L, et al. (2017) Multimodal fundus imaging of outer retinal tubulations in choroidal osteoma patients. Retina.






























